Search
Search
Imaging “hidden” regions of the heart
After suffering a heart attack, some patients develop a microvascular obstruction, an area of the injured heart with extremely poor blood flow. These patients are at an increased risk of developing heart failure in the future.
Medical imaging technologies such as magnetic resonance imaging (MRI) and positron emission tomography (PET) can be used to study the remodeling process after a heart attack that can lead to a microvascular obstruction. However, poor blood flow makes it difficult to get contrast agents into the obstruction. Contrast agents are used in medical imaging to show contrast between different types of tissue, such as damaged and healthy tissue.
Benjamin Wilk, a PhD candidate at Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry, will investigate whether a hybrid PET/MRI system and a new method of administering contrast agents can allow researchers to image microvascular obstructions and study these “hidden” regions in the heart.
Contrast agents are usually injected as a bolus, meaning the entire injection is administered immediately. In this study, participants will instead receive a constant infusion of an MRI contrast agent and PET tracer, which means the injection will be delivered over the course of an hour. The MRI contrast agent they are using is sensitive to blood flow and scar tissue, and the PET tracer is sensitive to inflammatory cells.
This will allow researchers to study the anatomy, blood flow and inflammatory processes in microvascular obstructions a week after heart attack. Participants will then be imaged again after six weeks to study the long-term effects on heart function.
“Studying the heart after a heart attack using novel contrast agent injection strategies with simultaneous PET/MRI could provide crucial information for treatment planning, helping us reduce the number of people affected by heart failure in the future,” says Wilk. “This project could also lead to further research into finding better ways to administer PET tracers and MRI contrast agents. These methods could be applied to different diseases as well.”
Wilk received a Lawson Internal Research Fund (IRF) Studentship to conduct the study, which will be supervised by Dr. Frank Prato, Assistant Director, Lawson and leader of the Lawson Imaging research program at St. Joseph’s Health Care London.
“Lawson's IRF is valuable for students for many reasons. It not only allows us to conduct further research, it also enriches our experience by giving us opportunities to write grants and attend conferences,” adds Wilk.
The IRF is designed to provide Lawson scientists the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
Imaging the microbiome
Normally samples of bacteria must be removed from their microbiome environment for analysis, which can lead to changes in their metabolic activity and other behaviors, hindering our ability to accurately study the gut or urogenital microbiome.
“This could be avoided if we are able to observe the bacteria in the body using Magnetic Resonance Imaging (MRI),” says Sarah Donnelly, MSc student at Lawson Health Research Institute and the Department of Microbiology and Immunology and collaborative Molecular Imaging program at Western University’s Schulich School of Medicine & Dentistry.
She is investigating the possibility of using magnetically-labelled bacteria with MRI to more directly study microbial interactions in urological and other conditions.
“The hope is that in the future we can use imaging technologies to visualize aspects of the microbiome in its healthy state compared to diseased states to see the early signs of disease and take preventative measures or allow for early intervention,” she says.
Donnelly has received a Lawson Internal Research Fund (IRF) Studentship to conduct the study, which will be supervised by Dr. Jeremy Burton, scientist in Lawson’s Human Microbiome and Probiotics research program at St. Joseph’s Health Care London (St. Joseph’s) and appointed to the Departments of Surgery and Microbiology & Immunology at Schulich Medicine & Dentistry; and Dr. Donna Goldhawk, scientist in Lawson’s Imaging research program at St. Joseph’s and assistant professor in the Department of Medical Biophysics at Schulich Medicine & Dentistry.
Escherichia coli (E. coli) are a common bacterium found in the human gut microbiome and frequently cause non-intestinal conditions like urinary tract infections. The researchers will program E. coli to express an iron uptake gene, magA. This gene is taken from another type of bacteria called magnetotactic because of their response to Earth’s magnetic field. The researchers will study whether the increase in iron uptake caused by magA expression will allow MRI to detect the magnetic signal more clearly than it would in images of untransformed E.coli. This would make it possible to see the bacteria’s behavior in living subjects without removing the bacteria cells from the microbiome environment.
They will then use this technique to study how magA labelled bacteria affect biofilm on medical devices. A biofilm is a structure produced when certain bacteria adhere to a surface and then stick together.
They will also analyze how lithotripsy affects the bacteria’s spatial distribution and interactions in three-dimensional models of kidney stones. Lithotripsy uses shockwaves to break up kidney stones into smaller pieces that are able to pass naturally out of the body. However, these shockwaves not only affect kidney stones. The waves are sent throughout the tissue, and the bacteria living on these tissues may also be affected.
“While lithotripsy is effective in treating kidney stones, we don’t know the side effects of lithotripsy on the microbiome. The shockwaves could disturb the bacteria, potentially leading to diseases caused by an imbalance between helpful and harmful bacteria,” says Donnelly.
These laboratory models will allow the researchers to perform studies in vivo (in animal models) in the future.
“Health research is very important for the development of new technologies and treatments but it is often difficult to secure funding. The IRF program allows students to pursue research that would not otherwise be possible,” explains Donnelly.
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
Improving palliative cancer treatment with existing diagnostic scans: Study reveals promising results
A recent study from London Health Sciences Centre and Lawson Health Research Institute suggests that using existing diagnostic CT scans in planning simple palliative radiation treatments can significantly cut down the waiting time for urgent treatment, resulting in a better experience for cancer patients.
“Reducing the time patients spend in a cancer centre has far-reaching benefits,” said lead study author Melissa O’Neil an Advanced Practice Radiation Therapist at London Health Sciences Centre’s (LHSC) London Regional Cancer Program (LRCP). “Faster treatment initiation means quicker relief from symptoms for patients. Utilizing existing scans is also cost-effective and frees up appointment slots or staff, allowing us to accommodate and assist more patients in need.”

Palliative radiation therapy is used to relieve symptoms in patients whose cancers cannot be cured. It’s often used when tumours cause pain, neurological issues or breathing problems such as blocked airways.
In the current standard practice, patients referred for palliative radiation typically require a CT simulation scan before starting their treatment. This scan creates 3D images that the patient's health care team uses to develop a customized radiation treatment plan. Unfortunately, this process often takes several hours, even with efforts to speed it up.
However, many of these patients have undergone previous diagnostic CT scans as part of their routine medical care. Previous research has shown that radiation oncology teams can create suitable palliative treatment plans for patients with bone and soft tissue metastases using these existing scans. This approach is less time-consuming than the more intensive simulation scans.
In the current study, O’Neil and her colleagues explored whether using existing CT scans to plan treatment before a patient arrives at the cancer centre could reduce their wait time while still ensuring appropriate care. They randomly assigned 33 patients who needed palliative radiation for tumours in their chest, abdomen or pelvis to either the standard treatment planning with on-site CT simulation scans or to treatment planning using diagnostic CT scans taken within the previous 28 days.
The study found that patients who didn't need the extra CT simulation scan spent much less time at the cancer centre on the day of their treatment – just under 30 minutes compared to nearly five hours for the others. Treatments were delivered successfully, and patient perception on time spent at the cancer centre was improved for those whose treatment planning used diagnostic CT scans taken without the previous 28 days.
"For patients who need radiation to help treat symptoms of cancer, it's important for us to get them treated quickly and to minimize the time they spend waiting for medical appointments,” said Dr. David Palma, Radiation Oncologist at LHSC and Associate Scientist at Lawson. “This trial shows that this new approach not only saves resources by reducing the number of scans we do, but also substantially reduces the time patients spend waiting for urgent radiation.”
"These findings are incredibly promising, especially in light of the nationwide shortage of radiation therapists," said Dr. Michael Ott, Physician Department Executive for Oncology at LHSC. “Work like this has benefits that can reach far beyond London, offering more relief for patients across the country."
The findings were presented at the American Society for Radiation Oncology’s Annual Meeting on Oct. 3, 2023. This meeting is recognized globally as the leading radiation oncology scientific event, drawing more than 8,500 attendees each year.
While the study shows promise, the research team said it's important to note that using prior diagnostic scans may not be suitable for every type of cancer or patient. It depends on the specific area being treated and the technique used.
For more information, please contact:
Jessica Rabaey
Communications Consultant
London Health Sciences Centre
T: 519-685-8500 ext. 77728
Jessica.rabaey@lhsc.on.ca
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Improving surgery for wrist arthritis
Wrist arthritis can cause debilitating pain, weakness and decreased range of motion. When patients are first diagnosed, the condition can often be managed with activity modification and pain medication. However, as symptoms progress, patients eventually require surgery.
Surgeons typically perform a procedure called four-corner fusion to preserve wrist motion and provide pain relief. This surgery involves removing one of the carpal bones and fusing four of the remaining carpal bones. Although this procedure is one of the most common treatments for wrist arthritis, it is not known how the position of the fusion of the wrist bones affects range of motion and joint contact.
Lawson associate scientist Dr. Nina Suh is leading a study with the goal of improving the surgical technique for four-corner fusion to maximize wrist function and symptom relief, and delay wrist arthritis progression.
Dr. Suh and her team will use a customized active-motion wrist simulator to create different carpal bone fusion positions. They will then assess how these positions affect wrist motion and joint contact area.
“We hope this research will lead to new surgical techniques that will help us to more effectively manage wrist arthritis with four-corner fusion,” says Dr. Suh, who is also an orthopaedic surgeon at the Roth McFarlane Hand and Upper Limb Centre (HULC) at St. Joseph’s Health Care London and an assistant professor at Western University’s Schulich School of Medicine & Dentistry. “The project will also advance our understanding of wrist biomechanics, providing a foundation for the development of enhanced patient-specific surgical tools, such as custom wrist fusion devices and implants.”
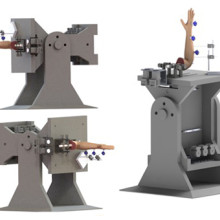
Image of the customized active-motion wrist simulator Dr. Nina Suh and her team are using to create different carpal bone fusion positions. They will then assess how these positions affect wrist motion and joint contact area.
The study is being funded through the Lawson Internal Research Fund (IRF), designed to allow scientists the opportunity to obtain start-up funds for new projects with exciting potential.
“The IRF program is valuable for scientists as external funding sources routinely require preliminary data to strengthen applications,” says Dr. Suh. “Particularly for new scientists such as myself, these grants provide seed funding that allows us to demonstrate the validity of our methodology and the clinical usefulness of our results.”
The IRF is designed to provide Lawson scientists the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
Injection of opioids linked to significant increase in bacterial heart infections
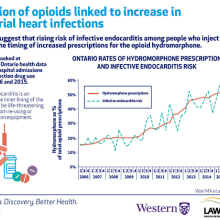
People who inject drugs are at a high risk for a number of health issues. In a new study from ICES, Lawson Health Research Institute and Western University, researchers discovered a significant rise in the risk of infective endocarditis, a serious heart infection, among Ontarians who inject drugs. When examining opioid prescriptions in the province, the research team discovered the increased risk of infective endocarditis may be related to the growing use of a specific opioid, hydromorphone.
The researchers looked at de-identified Ontario health data for 60,529 hospital admissions related to injection drug use between 2006 and 2015. Of the 60,529 admissions, 733 patients had infective endocarditis. Although hospital admission rates in people who inject drugs were stable over the study period, the risk of infective endocarditis increased from 13.4 admissions to 35.1 admissions every three months.
“Rates of infective endocarditis in people who inject drugs have been increasing around the world and our study shows this is true in Ontario,” says Dr. Matthew Weir, adjunct scientist at ICES, associate scientist at Lawson and assistant professor at Schulich School of Medicine & Dentistry, Western University. “We wondered if a change in the types of drugs people inject was responsible for this higher risk.”
Through further analysis of Ontario health data, the team discovered the increasing risk of infective endocarditis may be linked to a rise in prescriptions of the opioid hydromorphone. The number of hydromorphone prescriptions in Ontario increased from 16 per cent of all opioid prescriptions in 2006 to 53 per cent by 2015. This parallels the timing for increased risk of infective endocarditis among people who inject drugs.
The researchers initially suspected the increased risk for infective endocarditis would begin when controlled-release oxycodone was removed from the market in 2011.
“We thought hydromorphone prescriptions would increase when controlled-release oxycodone was removed from the market, leading to increased risk of heart infection,” says Dr. Michael Silverman, associate scientist at Lawson and associate professor at Schulich Medicine & Dentistry. “However, while the study did show a substantial increase in risk for infective endocarditis, it began in 2010.”
Traditional controlled-release oxycodone was easily dissolvable and people who inject drugs did not save or reuse their injection equipment. Controlled-release hydromorphone, the more common form of the drug, is more difficult to dissolve. Since residue of the drug gets left in injection equipment, injection drug users save the equipment for future use or to share with others. Reusing injection equipment allows multiple opportunities for bacterial contamination, increasing the chances that bacteria will be injected when the equipment is next used.
Infective endocarditis occurs when the inner lining of the heart becomes infected. It can be a life-threatening illness and research suggests it can be caused by sharing or re-using injection equipment, possibly through the injection of bacteria.
“While the timing was not what we expected, we did find a correlation between the rise in infective endocarditis and hydromorphone prescriptions,” says Dr. Sharon Koivu, Lawson scientist and associate professor at Schulich Medicine & Dentistry. “Our research is now focused on better understanding the potential relationship between the injection of hydromorphone and risk of infective endocarditis.”
The team is conducting ongoing studies that are looking at whether bacteria that cause infective endocarditis are more likely to survive in equipment used to prepare hydromorphone compared to other drugs.
“The opioid crisis is one of the most pressing health issues of our time. Our findings not only confirm an increasing risk of infective endocarditis in persons who inject drugs but also offer the first evidence for why it might be happening,” says Dr. Weir. “Through research and collaboration, we hope to further collect the evidence needed to address this global problem.”
The study, “The risk of infective endocarditis among people who inject drugs: A retrospective, population-based time series analysis,” is published today in CMAJ (Canadian Medical Association Journal).
Institute Team
Administration
Research Administration: responsible for the Lawson Approval process, delivery of Lawson’s Quality Assurance and Education program for clinical research, contract negotiation and approval for research, including industry-sponsored and investigator-initiated contracts, and fee-for-service support through Lawson Clinical Research Services.
Finance: responsible for the ongoing management of all research grants and contracts awarded to Lawson researchers; works closely with researchers, administrative staff, and funding sponsors to ensure adherence to funding guidelines and policies; manages the post-award functions for all research grants and contracts at the institute, including financial reporting, financial analysis and forecasting, cash flow and expenditure monitoring, compliance oversight, audit facilitation, and communicating with funding sponsors.
Research Human Resources: responsible for providing human resource services for Lawson researchers and staff, including acting as liaison between hospital Human Resources (HR) departments and Western faculties; the health and safety component facilitates standardizing safety processes and ensuring relevant legislation and safety standards are being met.
Research Operations & Technical Services: responsible for organizing the operations of Lawson’s vivarium/animal care facilities and services, as well as coordinating laboratory space, renovations, equipment and maintenance aspects of Lawson.
Research Informatics: responsible for supporting clinical researchers who have software development and database requirements by providing robust infrastructure to support their research activities, on a safe, secure IT platform to ensure patient confidentiality for clinical activities; and providing assistance with application development, data collection, data extraction, archiving, collaboration, analysis and reporting.
Strategic Planning and Development
Communications & External Relations: responsible for building and managing the Lawson brand and reputation, including public relations, media relations, marketing, special events, web presence and social media, advocacy, strategic planning and issues management.
Grant Development: responsible for facilitating the full spectrum of research grant submissions, including grant coordination for large government grant applications; development of grantsmanship; dissemination of new information pertaining to research and training grants opportunities; and, institution submissions and sign-off processes for CIHR, CFI, ORF, etc.
Business Development: responsible for providing services to Lawson investigators to facilitate the transfer of medical research from the laboratory to commercial use, including assisting with patenting new discoveries and finding commercial partners for collaborative research and licensing. Expertise is offered in the areas of intellectual property protection, marketing, licensing agreements and formation of start-up companies. Commercialization opportunities at Lawson are managed through WORLDiscoveries®, the business development arm of London’s extensive research network and the bridge between local invention and global industry.
Research Infrastructure: responsible for the development and implementation of a research master plan for all Lawson sites, including identifying potential research space solutions to meet the evolving needs of researchers, and working with the Facilities Planning departments at both hospitals to operationalize research space plans.
Investing in life-changing research
Through donor support, endowed research chairs are exploring and answering some of the most profound and complex research questions of our time.
Among cherished family photos and special mementos in the office of Jeremy Burton, PhD, is a slightly faded photo of a young woman. Burton points out the framed photo as he enthusiastically talks about his work. It’s a young Miriam Burnett, after whom the Miriam Burnett Chair in Urological Sciences is named. It’s also the first endowed research chair position Burton held at St. Joseph’s Health Care London (St. Joseph’s).
As the research chair for seven years, Burton speaks fondly about the relationship he has with the Burnett family and the crucial role their support has played in advancing his research.
“Thanks to their funding, we became one of the world leaders in urological microbiome research,” he says.
Endowed research chairs at St. Joseph’s receive consistent and sustainable funding so that research leaders and their teams can answer the most profound and complex health questions of our time.
For decades, donors have been inspired by the clinical research taking place at St. Joseph’s and have heavily invested in endowed research chairs. Today, St. Joseph’s Health Care Foundation manages seven endowed chairs focused on several areas, including molecular imaging, fetal and newborn growth and diabetes. Working in partnership with Western University, and with donor support, the foundation recently established four new endowed chairs in mobility, medical biophysics, medical imaging and ophthalmology.
“Medical research in Canada is chronically underfunded, and there is almost no sustainable funding for hospital-based research positions,” says Michelle Campbell, President & CEO, St. Joseph’s Health Care Foundation. “Private philanthropy has filled that gap for years. When a donor gives to an endowed research chair, they are building capacity in the present day and creating future value and opportunity. An endowed gift has a multiplier effect.”
Burton, now the endowed Research Chair in Human Microbiome and Probiotics, has many reasons to be grateful for this support. Not only does the endowed fund pay for Burton’s research salary, it also partially supports the salaries of a lab manager and technical team – all vital for a sophisticated lab to be successful.
The funding also provides the gift of time – a diminishing commodity for any busy research team.
“Scientists need more time to think,” says Burton, a Lawson Research Institute (Lawson) scientist. “We are incrementally being stretched in multiple directions, and the funding gives us the time to do what we are meant to do – find answers to important clinical questions and find solutions to medical problems.”
Distinguished Lawson scientist and university professor Cheryl Forchuk, PhD, wholeheartedly agrees. She recently completed her final term as The Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation & Recovery, another endowed position. As Chair, Forchuk provided scientific and administrative leadership to a large group of researchers based at St. Joseph’s Parkwood Institute focused on mental health, activity and mobility, and cognitive vitality and brain health.
Many research leaders, she explains, can afford to spend only two days a week on their own research projects. Endowed chair positions change that.
“Imagine travelling across the country to create a national study focused on homelessness, two days a week at a time,” she suggests candidly. “You couldn’t.”
Forchuk is referring to her landmark project to better understand how many people in Canada are homeless and who they are. The goal was to develop more accurate sources of data and recommend appropriate support and services. Her work is already resulting in important changes.
Today, Forchuk is embarking on another cross-country research project to find solutions related to homelessness for Canadian veterans who are women.
Like Forchuk, Burton’s Chair position requires him to provide operational and research leadership, including developing research networks and partnerships nationally and internationally to advance studies that will revolutionize care.
“As the Chair, I think it is important that I have wide-ranging projects that benefit people in our own community and beyond,” says Burton, who is optimistic about the outcomes of several of his team’s studies.
He recently partnered with London’s First Episode Mood and Anxiety Program to study the impact of fermented foods on the microbiome of young people taking medications for mental health conditions.
One of the side effects of these medications is weight gain, which deters some patients from taking it. By providing patients with slow-release apple cider capsules, which have similar properties to fermented foods and positively affect the microbiome, they have seen an overall improvement in participants’ mental health and cholesterol after just a few months.
Reflecting on his team’s research achievements to date and the potential of what’s to come, Burton emphasizes how vital endowed chairs are to the sustainability of research and the hope to translate newly discovered knowledge into medical practice.
“Research funding from other sources comes and goes,” he says, “but endowed chair positions that are focused on improving human health provide continuity, build research and create change benefiting all of us.”