Search
Search
New imaging tool for diagnosing heart disease
An international team led by scientists from Lawson Health Research Institute and Cedars-Sinai Medical Center are the first to show that Magnetic Resonance Imaging (MRI) can be used to measure how the heart uses oxygen for both healthy patients and those with heart disease.
Reduced blood flow to the heart muscle is the leading cause of death in the Western world. Currently, the diagnostic tests available to measure blood flow to the heart require injection of radioactive chemicals or contrast agents that change the MRI signal and detect the presence of disease. There are small but finite associated risks and it is not recommended for a variety of patients including those with poor kidney function.
Standard methods
More than 500,000 of these tests are performed each year in Canada. A patient suspected of coronary heart disease for example may have reasonably normal blood flow at rest but as soon as they exercise they have pain or feel out of breath. They need more oxygen delivered to the heart tissue but due to vessels being compromised that doesn’t happen.
The standard technique is usually done in two days with the goal of seeing if the heart can increase blood flow when more oxygen is needed. The first test studies the patient at rest to see what the blood flow is like in the heart. This is a nuclear medicine imaging test that requires radioactive material to be injected and takes about an hour or more to complete.
They next day, they come for the same test but with the introduction of a stressor. That can be physical exercise but more often they are given an injection of a chemical drug which stimulates the heart and increases blood flow. This is in addition to a second injection of the radioactive material. The heart is imaged to see the level of oxygen getting to different parts of the heart and whether there are obstructions or reduction in size of the surrounding arteries.
A new stress test
“We wanted a non-invasive way to image the heart and replace the stress stimulus, and drastically reduce the amount of time needed for testing,” says Dr. Frank Prato, Lawson Assistant Director for Imaging. “This new method, cardiac functional MRI (cfMRI), does not require needles or chemicals being injected into the body. It eliminates the existing risks and can be used on all patients."
The team included researchers from Lawson; Cedars-Sinai Medical Center and University of California; King’s College in the United Kingdom; University Health Network and the University of Toronto; Siemens Healthineers; and, University of Edinburgh in the United Kingdom.
“Our discovery shows that we can use MRI to study heart muscle activity,” explains Dr. Prato. “We’ve been successful in using a pre-clinical model and now we are preparing to show this can be used to accurately detect heart disease in patients.”
To replace the stress test, this new technique uses repeat exposure to carbon dioxide to test how well the heart’s blood vessels are working to deliver oxygen to the muscle. A breathing machine changes the concentration of carbon dioxide in the blood. Levels are brought up for three minutes and then back down to normal four times. These changes should result in a change in blood flow to the heart, but does not happen when disease is present.
The cfMRI method reliably detects whether these changes are present and is comparable to the information gathered from the current two-day technique – in much less time and without injections. Dr. Prato notes that “we don’t want to stress the heart. We want to see whether there is capacity in the heart to increase blood flow if the heart needs to work harder.”
A brilliant discovery
Other researchers have explored oxygenation-sensitive MRI but initial results contained a high level of ‘noise’ with blurry images. Project leader and partner Dr. Rohan Dharmakumar, Associate Director of the Biomedical Imaging Research Institute at Cedars-Sinai Medical Center, believed that the noise was actually variation in the heart’s processing of oxygen. He engineered a way to average this variation and through testing at Lawson the team discovered that the noise is actually a new way to study how the heart works.
“We’ve opened the door to a new era and totally novel way of doing cardiac stress testing to identify patients with ischemic heart disease” says Dr. Dharmakumar. “This approach overcomes the limitations of all the current diagnostics – there would no longer be a need for injections or physical stress testing like running on treadmills.”
Through investigating this technique, they learned that the blurry images were showing normal physiological variability. People often think of heart rate as being stable, but in fact a heart that is unable to keep up with stressors indicates that disease is developing. In a healthy heart, the oxygen distribution to the tissue needs to vary.
“It’s a very exciting time. We had to bring all the technologies together to be able to image these kinds of changes in blood flow moment to moment,” says Dr. Prato.
He adds that “using MRI will not only be safer than present methods, but also provide more detailed information and much earlier on in the disease process.” Following initial testing through clinical trials, he sees this being used with patients clinically within a few years.
Moving forward
In addition to studying coronary artery disease, the method could be used in other cases where heart blood flow is affected such as the effects of a heart attack or damages to the heart during cancer treatment. Due to its minimal risk, this new tool could be safely used with the same patient multiple times to better select the right treatment and find out early on if it is working. Dr. Prato notes that “with this new window into how the heart works, we have a lot to explore when it comes to the role of oxygen in health and disease.”
The next steps of the research include a proof of principle study in London, Ontario with 20 patients. Following standard tests using the conventional technique at other sites, the participants will then come in for the experimental test to show that it produces the same result. The research would then move into a multi-centre clinical trial internationally.
The study “Accurate needle-free assessment of myocardial oxygenation for ischemic heart disease in canines using Magnetic Resonance Imaging” is published in Science Translational Medicine.
New national strategy to tackle dementia
Researchers in London, Ontario have been awarded $1.345 million over five years through the second phase of the Canadian Consortium on Neurodegeneration in Aging (CCNA), announced today as part of Canada’s first national dementia strategy. CCNA is a collaborative research program tackling the challenge of dementia and other neurodegenerative illnesses.
A Dementia Strategy for Canada: Together We Aspire focuses on preventing dementia, advancing therapies and finding a cure, as well as improving quality of life for people living with dementia and caregivers.
Clinician researchers from across the country working together
Dr. Manuel Montero-Odasso, Scientist at Lawson Health Research Institute, is world renowned for his findings on the relationship between cognition and mobility in the elderly, and gait as a predictor of frailty and dementia. He leads the Mobility, Exercise and Cognition (MEC) Team in London, comprised of top researchers in the areas of mobility, exercise and brain health.
“Evidence from other countries with dementia strategies shows that coordinated, targeted efforts at the national level improves results for all aspects of dementia care and also for research,” says Dr. Montero-Odasso, also a geriatrician and Director of the Gait and Brain Lab at Parkwood Institute, a part of St. Joseph’s Health Care London.
CCNA was purpose-built to synergize dementia research within the Canadian context. Phase I saw the creation of infrastructure fostering collaboration amongst Canadian researchers, and there are now 20 teams built around important research topics.
“This kind of effective national collaboration by scientists and clinicians from many disciplines gives the CCNA a cutting edge in research, prevention, treatment and management of all forms of dementia,” explains Dr. Montero-ODasso. “We created a national network of researchers form west to east coast with a high level of expertise to deliver lifestyle interventions to improve cognition and slow down progression to dementia. I feel privileged working with such excellent investigators and leading this important endeavour locally.”
Preventing dementia through lifestyle changes
The MEC team has several projects in the works, but the majority of the new funding is to complete the SYNERGIC Trial, SYNchronizing Exercises and Remedies on Gait and Cognition.
This first-in-the-world clinical study is testing a triple intervention aimed at treating Mild Cognitive Impairment (MCI) and delaying the onset of dementia. The SYNERGIC Trial incorporates physical exercises and cognitive training, along with vitamin D supplementation to determine the best treatment for improving mobility and cognition.
“We are looking at how interventions will work together and targeting cognitive decline at its earliest stage – individuals with MIC,” explains Dr. Montero-Odasso. “Both physical and cognitive exercises have shown promising effects for maintaining cognition, while vitamin D deficiency is associated with cognitive decline.”
A professor at Western University’s Schulich Medicine & Dentistry, Dr. Montero-Odasso partners with researchers from across the city including Dr. Rob Bartha, imaging scientist at Schulich Medicine & Dentistry and Robarts Research Institute at Western University, and Dr. Kevin Schoemaker who leads the Laboratory for Brain and Heart Health.
Study participants in the SYNERGIC Trial are asked to complete an individualized and progressive routine of exercises and cognitive training three times a week for six months, with one final assessment at 12 months. The main site for the study is Parkwood Institute with the physical exercises taking place at the Labatt Health Sciences Building on the Western campus.
To date, 138 research patients has been recruited across multiple sites in Canada.
One participant’s experience
One day, Peter Saracino saw an advertisement about a research study. They were looking for participants who were a minimum age of 60 and had minor cognitive impairment. He felt he fit the bill and he was interested in this kind of research.
“I have family members who suffered from forms of dementia and Parkinson’s Disease. I really understand how hard it hits and I liked that this study was about prevention,” explains Peter.
Going into it, Peter thought he was in pretty good shape. He has two dogs and walks them regularly. “But by going to the gym and doing the exercises and faster-paced walking, I realized that I wasn’t in as good shape as I thought. My diet was under control but I was still taking blood pressure medication. I didn’t have much energy.”
After 10 weeks in the study, he feels better than he has for over a decade. “I can garden for longer. I took two notches off my belt. I no longer take my blood pressure medication. I actually feel younger.”
He remembered that last year he slipped and fell four times, which was very unusual for him. Part of his cognitive impairment is that he had trouble with balance, and that has improved for him as well.
Peter feels that “this is exactly the kind of research that the government should be investing in – an ounce of prevention is worth a pound of cure. This kind of research leads to keeping people independent and healthier as they get older. People are happier. They feel like doing more. There is no downside to improving someone’s health through lifestyle changes, and in fact it is cost effective and helps ease the burden on the health care system.”
Looking forward
“Our preliminary analysis from SYNERGIC is giving us a strong indication that a multimodal approach, combining physical exercise, cognitive training and supplementation, has a synergistic effect. It seems the whole is greater than the sum of its parts,” says Dr. Montero-Odasso.
A major goal for the work of the MEC team in London is to translate their research findings into clinical guidelines that can be used at the front line of care. “Practitioners understand the overall importance of exercise and cognitive vitality, but we are missing more specific guidelines on what kind and how much will work for different patients. Basically, what is an effective lifestyle prescription.”

Dr. Montero-Odasso adds that “as our population ages, a comprehensive strategy is vital to ensure the growing number of those living with dementia receive the care and support they deserve. Over half a million Canadians are currently living with dementia. By 2031, this number is expected to nearly double.” More than one third of dementia cases might be preventable.
CCNA Phase II
In CCNA’s Phase II, researchers are working on analyzing the overall health of every patient in a large clinical cohort study, COMPASS-ND. This information will be used to enhance understanding of how changes in the brain affect dementia severity and ways to reduce and prevent this through lifestyle changes. Lawson is the leading recruitment site for COMPASS-ND and the London team will be instrumental in the larger lifestyle interventions moving forward.
CCNA is funded by the Government of Canada, Canadian Institutes of Health Research (CIHR) and other funding partners. CIHR is providing $31.6 million, and partners—including provincial agencies and non-profit organizations—are providing an additional $14.4 million for a total investment of $46 million over five years. The research on dementia prevention, diagnosis, treatment and care as part of Phase II of the CCNA will support the national strategy.
Related stories
New research on reducing harm for people who use methamphetamine
At a virtual event, a research team led by Lawson Health Research Institute announced details of the Methamphetamine Harm Reduction Project that will study the integration of harm reduction strategies into hospital settings for people who use methamphetamine.
Evidence-based harm reduction strategies for methamphetamine use, for example needle/syringe services, supervised injection sites and safe supplies, have been used in the community to reduce health risks such as infection and overdose.
“Harm reduction strategies are rarely used within hospitals in Canada. The current standard of care does not allow the use of illicit substances in hospitals as the safe consumption of substances requires an exemption under section 56.1 of the Controlled Drugs and Substances Act from Health Canada,” explains Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and study co-principal investigator.
Recent studies from London, Ontario found that substance use in hospital is happening and poses a greater risk of infection than in the community.
“There is an assumption that people in hospital aren’t using, but in fact we’ve found that almost 50 per cent of patients admitted to hospital with an infection related to substance use are continuing to inject during their stay. That is clearly an underestimate because many patients are worried about being stigmatized or other consequences of using in hospital and so may not be willing to report it to researchers or tell their health care providers,” explains Dr. Michael Silverman, Associate Scientist at Lawson, city-wide Chair/Chief of Infectious Diseases for London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, and study co-principal investigator.
Findings have shown that patients are more likely to get an infection related to substance use when being treated in the hospital as opposed to other settings and many people who are using leave hospital against medical advice, putting their health and safety at risk. “People aren’t able to access safe ways to use substances and they are doing it in secret, so it’s not the best way to do it to prevent infection. There are also gaps in support for withdrawal and other addiction services,” says Dr. Silverman.
The research team will lead a four-year project with recruitment of up to 360 adults aged 16-85 years with past experience or current use of methamphetamine, including inpatients, outpatients and those in community outreach programs. Up to 180 health care and service providers will be recruited to share their perspectives on harm reduction strategies. After the consultation phase in the first year, with approval from Health Canada, the identified set of strategies based on the perspectives of people with lived experience will be implemented within LHSC and St. Joseph’s hospital sites.
“To our knowledge, there are only five supervised consumption services based in acute care hospitals in the world. Three of these sites are in Europe and there are two locations in Canada that have implemented a similar approach. London will be the second place in North America to implement harm reduction strategies for substance users within hospital walls,” adds Dr. Forchuk.
“We are leading the way towards a groundbreaking shift to greatly improve health care for Canadians who use substances.”
Potential harm reduction strategies are safe injection sites or safe places to use substances, new needles and syringes, available Sharp boxes, support for detox and withdrawal, medication, resources at discharge, and enhanced addiction services and counseling.
Sonja Burke, the Director of Harm Reduction Services at the Regional HIV/AIDS Connection, notes there has been a marked increase in more complex health care needs and a high rate of deaths in the community for people who are experiencing homelessness and addiction.
“Harm reduction is about meeting people where they are without stigma or assumptions, accepting that substance use is a part of their life,” says Burke. “Our experience in the supervised consumption services proves that once a person is able to use their pre-obtained substances, they will engage in further supports for their health care. We have to change how the supports are being provided within the system to ensure we are reducing health risks and death.”
New research on reducing harm for people who use methamphetamine in hospital
LONDON, ON – At a virtual event today, a research team from Lawson Health Research Institute is announcing details of the Methamphetamine Harm Reduction Project that will test the integration of harm reduction strategies into hospital settings for people who use methamphetamine.
Evidence-based harm reduction strategies for methamphetamine use, for example needle/syringe services, supervised injection sites and safe supplies, have been used in the community to reduce health risks such as infection and overdose. “Harm reduction strategies are rarely used within hospitals in Canada. The current standard of care does not allow the use of illicit substances in hospitals as the safe consumption of substances requires an exemption under section 56.1 of the Controlled Drugs and Substances Act from Health Canada,” explains Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and study co-principal investigator.
Recent studies from London, Ontario found that substance use in hospital is happening and poses a greater risk of infection than in the community.
“There is an assumption that people in hospital aren’t using, but in fact we’ve found that almost 50 per cent of patients admitted to hospital with an infection related to substance use are continuing to inject during their stay. That is clearly an underestimate because many patients are worried about being stigmatized or other consequences of using in hospital and so may not be willing to report it to researchers or tell their health care providers,” explains Dr. Michael Silverman, Associate Scientist at Lawson, city-wide Chair/Chief of Infectious Diseases for London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, and study co-principal investigator.
Findings have shown that patients are more likely to get an infection related to substance use when being treated in the hospital as opposed to other settings and many people who are using leave hospital against medical advice, putting their health and safety at risk. “People aren’t able to access safe ways to use substances and they are doing it in secret, so it’s not the best way to do it to prevent infection. There are also gaps in support for withdrawal and other addiction services,” says Dr. Silverman.
The research team will lead a four-year project with recruitment of up to 360 adults aged 16-85 years with past experience or current use of methamphetamine, including inpatients, outpatients and those in community outreach programs. Up to 180 health care and service providers will be recruited to share their perspectives on harm reduction strategies. After the consultation phase in the first year, with approval from Health Canada, the identified set of strategies based on the perspectives of people with lived experience will be implemented within LHSC and St. Joseph’s hospital sites.
“To our knowledge, there are only five supervised consumption services based in acute care hospitals in the world. Three of these sites are in Europe and there are two locations in Canada that have implemented a similar approach. London will be the second place in North America to implement harm reduction strategies for substance users within hospital walls,” adds Dr. Forchuk. “We are leading the way towards a groundbreaking shift to greatly improve health care for Canadians who use substances.”
Potential harm reduction strategies are safe injection sites or safe places to use substances, new needles and syringes, available Sharp boxes, support for detox and withdrawal, medication, resources at discharge, and enhanced addiction services and counseling.
Sonja Burke, the Director of Harm Reduction Services at the Regional HIV/AIDS Connection, notes there has been a marked increase in more complex health care needs and a high rate of deaths in the community for people who are experiencing homelessness and addiction.
“Harm reduction is about meeting people where they are without stigma or assumptions, accepting that substance use is a part of their life,” says Burke. “Our experience in the supervised consumption services proves that once a person is able to use their pre-obtained substances, they will engage in further supports for their health care. We have to change how the supports are being provided within the system to ensure we are reducing health risks and death.”
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New robotic 3D ultrasound may improve accuracy of liver cancer ablation therapy
LONDON, ON – A new system that turns ultrasounds into a 3D image could make treatment of liver cancer using thermal ablation more accurate, a new simulated study from Lawson Health Research Institute and Western University has found.
Liver cancer is the fourth leading cause of cancer death globally. While surgery is one treatment option, thermal ablation, using heat to destroy the cancerous tumour, can have fewer complications and a shorter recovery time. It can also be used for patients who are not surgical candidates.
Thermal ablation requires precise needle placement to treat the cancer without damaging the vital organs and blood vessels around it.
“It's very important that we get the needle right in the centre of the tumour,” says Dr. Derek Cool, Associate Scientist at Lawson, Assistant Professor at Western University’s Schulich School of Medicine & Dentistry and Interventional Radiologist at London Health Sciences Centre (LHSC). “If the treatment area doesn't fully cover the tumour, patients are left with a small amount of residual cancer, risking recurrence and the need for additional treatment.”
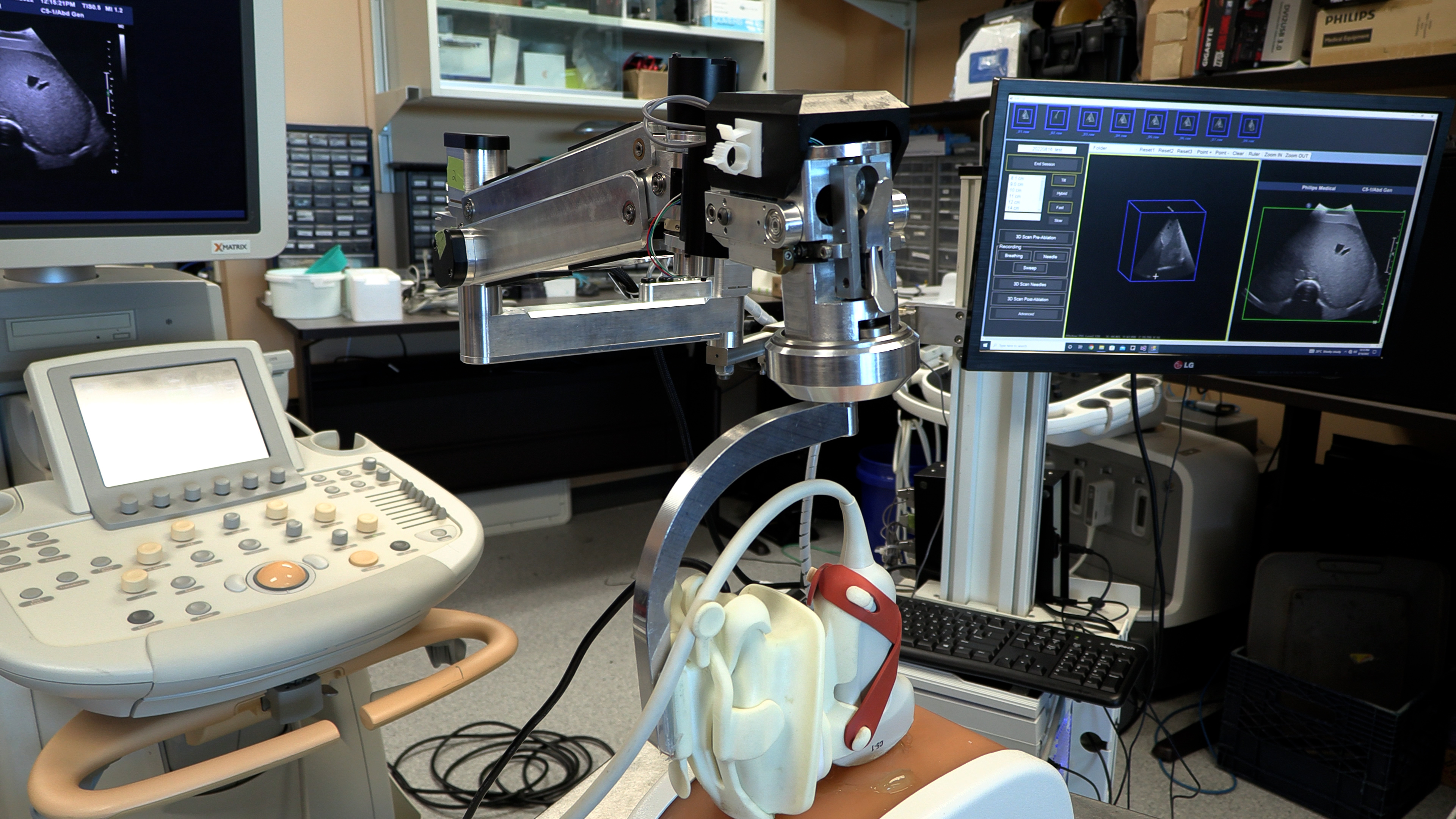
Ultrasound or CT (computerized tomography) imaging is normally used to guide needle placement, but both are limited. Ultrasound is widely available and can be done in real-time, but only delivers a 2D image. While a CT scan provides a 3D image, it isn’t in real-time and can be a lengthy process.
“We developed a new 3D ultrasound method that shows promise in analyzing whether the complete liver tumour will be ablated by the procedure,” explains Dr. Aaron Fenster, a Professor at Schulich and Scientist at Robarts Research Institute. “And we're now using the same system to guide the needle directly into the centre of the tumor.”
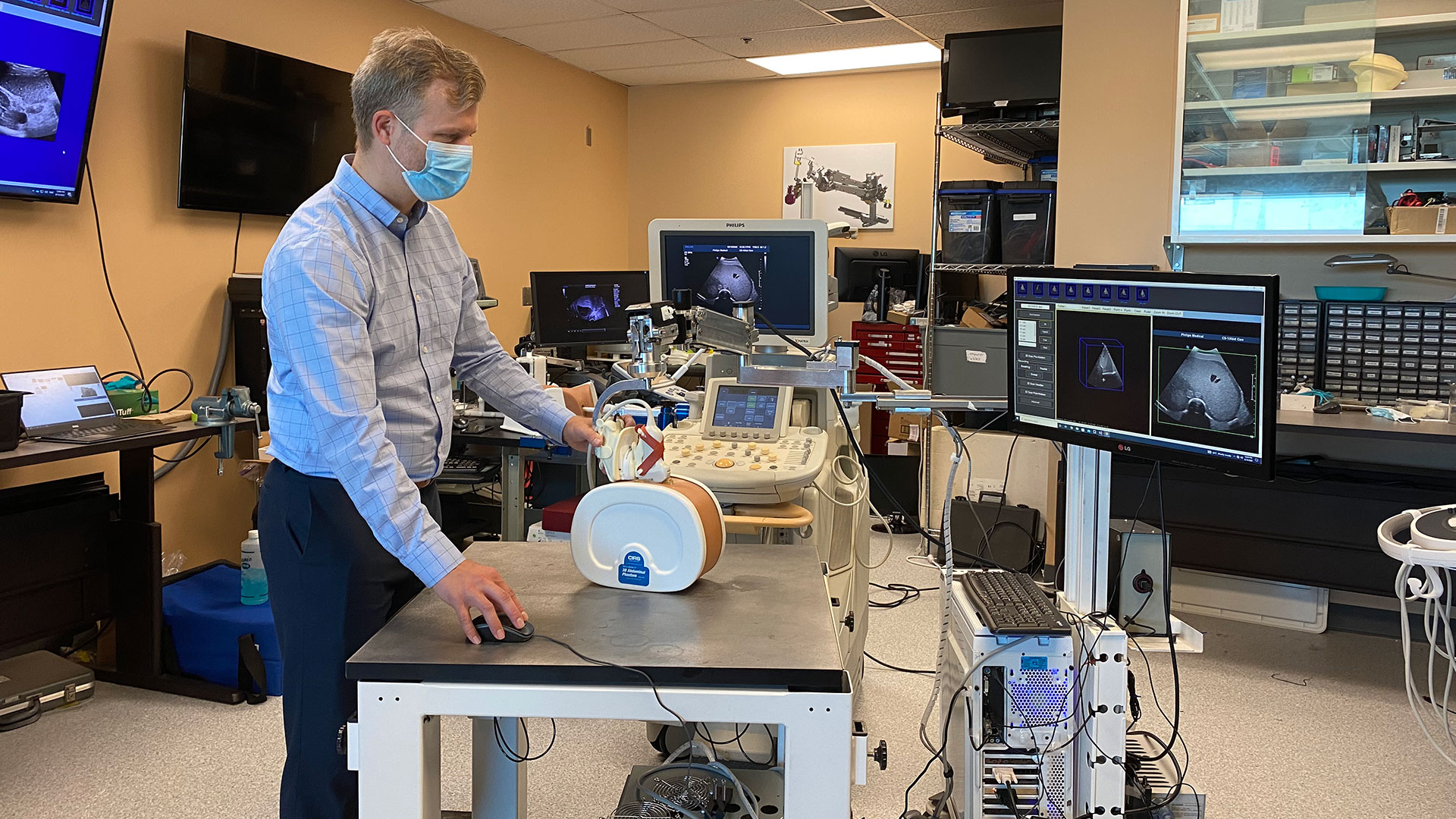
To create the 3D ultrasound images, a robotic cradle moves a standard ultrasound probe, collecting images and stacking them like puzzle pieces.
The simulated study, published in IEEE Transactions on Medical Imaging, used data from 14 patient cases at LHSC to analyze accuracy of the technology. It found that while 64.3 per cent of cases showed complete tumour coverage with standard imaging methods, the new system could result in complete coverage for 92.9 per cent of cases (13 of 14 cases). The researchers found that the remaining case could benefit from increasing the ablation time or intensity.
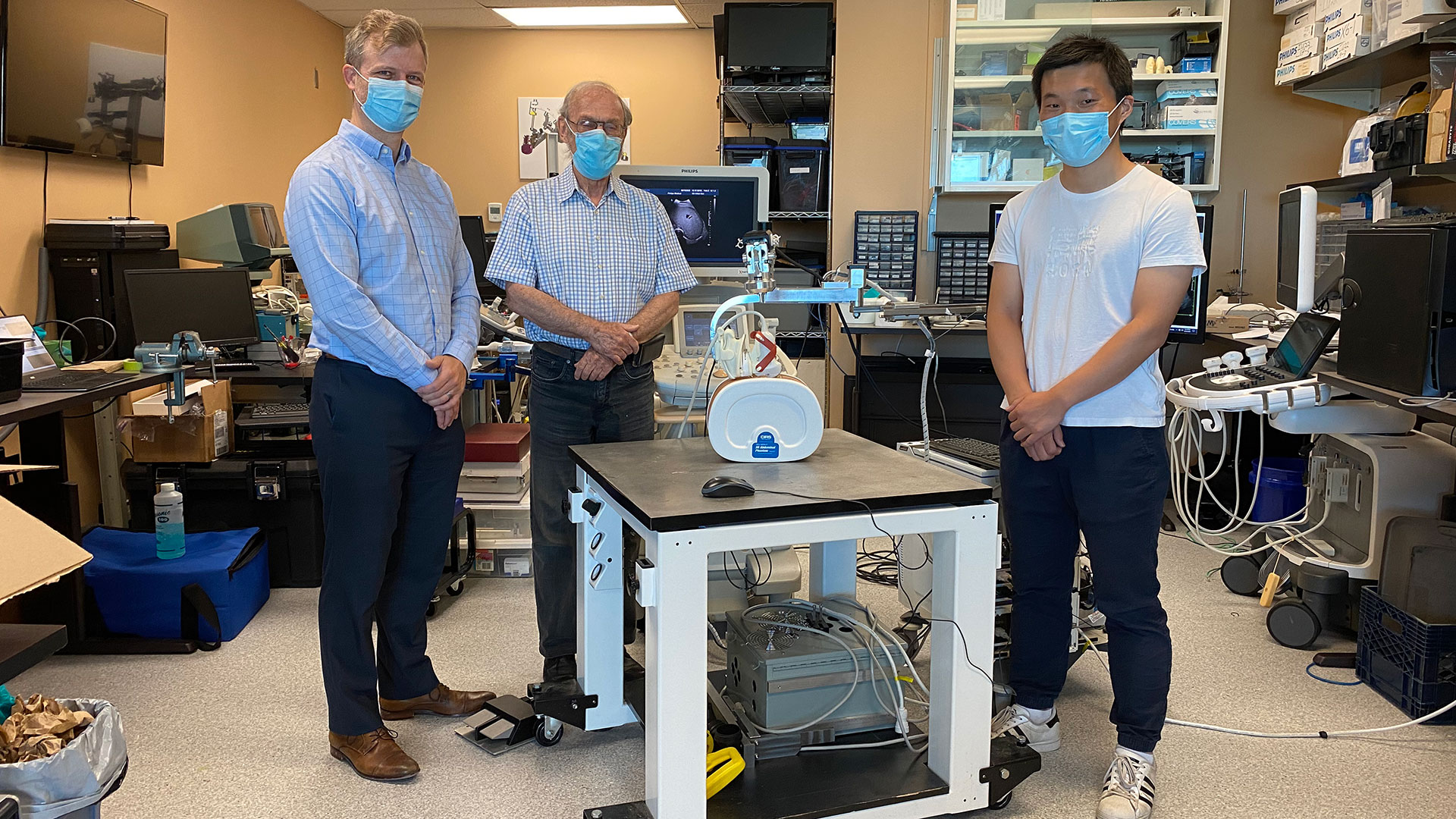
“Our next step is to move from simulation studies to a clinical trial,” says Dr. Cool.
If proven effective, the robotic ultrasound system’s portability could potentially allow for more widespread use of 3D ultrasound imaging, including in smaller health care centres. By eliminating the need for CT scans, it could also help to reduce imaging wait times.
“If a clinical trial shows the approach is more accurate and more precise than conventional techniques, there would be a direct impact on patient care,” says Dr. Fenster. “We hope to explore commercialization to license the technology and distribute it worldwide.”

Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
New study examining if probiotics can improve outcomes in knee replacement surgeries
Researchers at Lawson Health Research Institute are examining whether the use of a daily probiotic can improve outcomes in patients who undergo a total knee replacement surgery.
There are more than 70,000 knee replacement surgeries in Canada each year, and up to 10 per cent of patients experience complications following the procedure.
“One in five patients are dissatisfied after surgery due to pain and discomfort, and some patients need a repeat surgery because there is complication, infection or loosening of the joint,” says Dr. Matthew Teeter, Lawson Scientist at London Health Sciences Centre (LHSC).

Dr. Teeter and the research team are focused on improving patient outcomes. Recognizing that knee replacement patients who are considered healthy tend to have better outcomes, they are interested in how they can better support patients’ overall health as one way to optimize their outcomes.
“The knee replacement patients I see in clinic are very diverse - from young healthy active patients to medically complex to socioeconomically disadvantaged,” says Dr. Brent Lanting, Lawson Scientist and Orthopaedic Surgeon at LHSC. “We know those with poor health do not do as well as those with good health, good diet, and good supports. This study is profound in that it investigates a core aspect of our health – the gut microbiome.”

The research team will recruit 30 participants who are scheduled for a knee replacement surgery. Half of the participants will receive a daily probiotic for six-weeks ahead of the surgery, and the other half will act as a control group.
“Our microbiome is a large part of why we are healthy. A healthy person has a microbiome that produces vitamins and other things which cross over to our system and helps promote healing,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph’s Health Care London. “We are hoping it will improve more deep healing and prevention of the rejection of the joint by improving the microbiota by giving probiotics.”
The team will assess outcomes using CT imaging, looking at the bone and implant and how it is fixing into place. They will also use PET/MRI to look at the cellular activity around the joint and inflammation.
“This should give us a sharp focus of what is going on with the joint and help us determine if there was a positive effect by using probiotics,” explains Dr. Teeter.
If the pilot study proves to be promising, the team will then work towards a larger clinical trial, combining probiotics into pre-surgical care.
“Ultimately, we want better patient outcomes with a simple treatment,” adds Dr. Burton. “If we can help improve outcomes with the use of a daily probiotic, that is a great win.”
The research team received a New Frontiers in Research Fund (NFRF) of $250,000 over three years to conduct this study.
New study shows technology could play an important role in mental health support
LONDON - In a study published in MDPI Journal, a team of researchers at Lawson Health Research Institute have shown that the use of technology may assist in better outcomes for those living with both mental health and physical disorders.
Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson, and her team embarked on a pilot study that used smart home monitoring solutions to assist those living with both a mental health disorder and other health challenges. The purpose of this pilot study was to see if technology could improve overall lifestyle and wellbeing.
“We began our research by using hospital prototype apartments – apartment style care spaces within hospital settings – that were equipped with smart home technology solutions such as a screen device, activity trackers, weigh scales and medication dispensers,” says Dr. Forchuk who is also the Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery at St. Joseph’s Health care London. “Once we tested it in a hospital setting, we wanted to find a way to take this idea out into the community in different kinds of housing and living situations to see if it would be beneficial.”
The research team partnered with the Canadian Mental Health Association (CMHA) and the London and Middlesex Community Housing (LMCH) to work together to retrofit the homes of the 13 study participants.
“We worked together with the participants and their care providers to choose what combination of technology they felt would be best for them,” says Dr. Forchuk. “No matter their health condition each participant wanted to be more active and independent, with the goal of staying out of hospital.”
All smart devices were connected to the Lawson Integrated Database, which is a database that can securely collect data from multiple sources such as health devices. This allowed care providers to send reminders to participants, while also tracking usage and results.
“The key benefits we noted was that study participants started to live healthier lives,” says Jonathan Serrato, Lawson Research Associate. “Participants logged going for walks and exercising more often, as well as making healthier food choices. Those who used the medication dispensers did not miss a single dose. The touch screen devices also allowed participants to easily communicate with care providers and support networks, and access more resources.”
Following the pilot study, the research team also published a subsequent paper, as a ‘how-to guide’ for utilizing smart home technology interventions as a health care tool.
“This paper is a helpful resource that outlines implications and considerations when it comes to smart home technologies,” adds Serrato. “There are many areas we touch upon such as security, privacy and feasibility as well as hardware and software information for those who would like to take on their own similar type of smart home technology project.”
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New study will assess fecal transplants in treatment of pancreatic cancer
Scientists examining microbiome to improve cancer therapies
MEDIA RELEASE
For Immediate Release
LONDON, ON- Pancreatic cancer is an aggressive disease that affects up to six-thousand Canadians a year and is the third leading cause of cancer deaths. In a new study a multidisciplinary team of scientists at Lawson Health Research Institute are examining the microbiome in the gut, as a possible gateway to improving treatment outcomes.
“Pancreatic cancer is very hard to treat, partially because when it’s detected, the cancer is usually in a later stage and spreads very quickly,” explains Dr. John Lenehan, Medical Oncologist at London Health Sciences Centre’s London Regional Cancer Program (LRCP) and Associate Scientist at Lawson. “Our best chemotherapy treatments for the average patient, will give them a little less than a year to live.”
With the goal of improving treatments for these patients the research team led by Dr. Saman Maleki, Scientist at Lawson, is studying whether changing the gut microbiome can result in better response to cancer treatments.
“We know that the microbiome plays an important role in patients’ response to various forms of systemic treatments such as immunotherapy and chemotherapy for different cancers,” says Dr. Maleki.
This unique study will happen in three stages. The first stage is an observational study to examine fecal samples of 52 patients at LRCP with advanced pancreatic cancer. The second stage will focus on using the samples from these patients in preclinical models to test new combinations of treatments. The final stage of the study will focus on intervention through human clinical trials by modifying a patient’s microbiome with something called a fecal transplant prior to treatment.
“The microbiome is involved in many aspects of cancer development and these organisms aren’t just living in the gut but also within the tumor,” says Dr. Michael Silverman, Lawson Scientist and Chair/Chief of Infectious Diseases at LHSC and St. Joseph’s Health Care London. “We believe that by giving people a fecal transplant, we can change the bacteria that live within the tumor and gut and then optimize the immune response to both the tumour and to treatment, with the goal of improving patient outcomes.”
Fecal transplants involve collecting stool from a healthy donor, preparing it in a lab and safely transplanting it to the patient, in this case with a capsule. The goal is to transplant the donor’s microbiome so that healthy bacteria will colonize in the patient’s gut.
“If you think of microbiome, each bacterium is like a little factory and all together they are a giant factory within us producing things we need,” explains Dr. Jeremy Burton, Lawson Scientist who specializes in human microbiome research. “Over time, a person’s diet, medications, and lifestyle can change the microbiome and it can have a big impact to the rest of our body.”
The research team was recently awarded a $450,000 Catalyst 2021 grant from the Weston Family Foundation to conduct this study, which is the first in the world focusing on prospectively modifying the microbiome in pancreatic cancer patients for treatments and outcomes.
“We normally don’t see this in one study where we go through the full spectrum of learning from patients, to looking at treatments, and then moving to a final intervention stage,” explains Dr. Maleki. “This has not been tried in pancreatic cancer before, but we think leveraging the microbiome and improving the immune response can potentially move the needle in this patient population.”
The team is recruiting both pancreatic cancer patients, as well as healthy volunteers for fecal transplant samples. Those interested in helping with fecal transplant donations can contact Dr. Seema Parvathy at 519-646-6100 ext. 61726 or email seemanair@@email
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New study will assess fecal transplants in treatment of pancreatic cancer
Pancreatic cancer is an aggressive disease that affects up to six-thousand Canadians a year and is the third leading cause of cancer deaths. In a new study a multidisciplinary team of scientists at Lawson Health Research Institute are examining the microbiome in the gut, as a possible gateway to improving treatment outcomes.
“Pancreatic cancer is very hard to treat, partially because when it’s detected, the cancer is usually in a later stage and spreads very quickly,” explains Dr. John Lenehan, Medical Oncologist at London Health Sciences Centre’s London Regional Cancer Program (LRCP) and Associate Scientist at Lawson. “Our best chemotherapy treatments for the average patient, will give them a little less than a year to live.”
With the goal of improving treatments for these patients the research team led by Dr. Saman Maleki, Scientist at Lawson, is studying whether changing the gut microbiome can result in better response to cancer treatments. “We know that the microbiome plays an important role in patients’ response to various forms of systemic treatments such as immunotherapy and chemotherapy for different cancers,” says Dr. Maleki.

Dr. John Lenehan, Dr. Jeremy Burton and Dr. Saman Maleki
This unique study will happen in three stages. The first stage is an observational study to examine fecal samples of 52 patients at LRCP with advanced pancreatic cancer. The second stage will focus on using the samples from these patients in preclinical models to test new combinations of treatments. The final stage of the study will focus on intervention through human clinical trials by modifying a patient’s microbiome with something called a fecal transplant prior to treatment.
“The microbiome is involved in many aspects of cancer development and these organisms aren’t just living in the gut but also within the tumor,” says Dr. Michael Silverman, Lawson Scientist and Chair/Chief of Infectious Diseases at LHSC and St. Joseph’s Health Care London. “We believe that by giving people a fecal transplant, we can change the bacteria that live within the tumor and gut and then optimize the immune response to both the tumour and to treatment, with the goal of improving patient outcomes.”
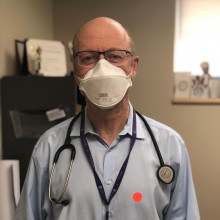
Dr. Michal Silverman, Lawson Associate Scientist
Fecal transplants involve collecting stool from a healthy donor, preparing it in a lab and safely transplanting it to the patient, in this case with a capsule. The goal is to transplant the donor’s microbiome so that healthy bacteria will colonize in the patient’s gut. “If you think of microbiome, each bacterium is like a little factory and all together they are a giant factory within us producing things we need,” explains Dr. Jeremy Burton, Lawson Scientist who specializes in human microbiome research. “Over time, a person’s diet, medications, and lifestyle can change the microbiome and it can have a big impact to the rest of our body.”
The research team was recently awarded a $450,000 Catalyst 2021 grant from the Weston Family Foundation to conduct this study, which is the first in the world focusing on prospectively modifying the microbiome in pancreatic cancer patients for treatments and outcomes.
“We normally don’t see this in one study where we go through the full spectrum of learning from patients, to looking at treatments, and then moving to a final intervention stage,” explains Dr. Maleki. “This has not been tried in pancreatic cancer before, but we think leveraging the microbiome and improving the immune response can potentially move the needle in this patient population.”
The team is recruiting both pancreatic cancer patients, as well as healthy volunteers for fecal transplant samples. Those interested in helping with fecal transplant donations can contact Dr. Seema Parvathy at 519-646-6100 ext. 61726 or email seemanair@@email
New urinary microbiome study could be first step in providing personalized care to patients with ureteral stents
LONDON, ONTARIO - For patients with kidney stones, ureteral stents (hollow devices placed in the ureter – the tube between the kidney and bladder) can be used temporarily to relieve urinary obstruction. Despite the use of antibiotics, ureteral stents often become encrusted with minerals and coated with bacteria. This can lead to complications like infection and the need for replacement surgery.
Published today in Cell Reports Medicine, researchers at Lawson Health Research Institute and Western University conducted a novel microbiome study to examine bacteria associated with ureteral stents. They found that nearly all the stents, whether visibly coated or not, had unique bacterial profiles that were most associated with a patient’s medical condition rather than antibiotic use. For patients with ureteral stents, they may benefit from a personalized approach to care and antibiotic treatment.
The study included 241 patients from St. Joseph’s Health Care London. The research team collected and analyzed patient urine samples and ureteral stents following surgical removal, as well as relevant patient information such as antibiotic use and history of infections.
“We wanted to know which bacteria were present and whether the bacteria found in urine samples corresponded to the bacteria found on a patient’s stent,” explains Dr. Kait Al, Postdoctoral Fellow at Lawson and at Western’s Schulich School of Medicine & Dentistry. “We found that there was a bacterial community present on almost all stents, even if they were not visibly affected, and that it differed from the bacterial community found in a patient’s urine.”
These findings challenge long-held beliefs that the urinary tract is a sterile environment devoid of bacteria.
The study revealed that the bacteria present were determined by an individual patient’s medical condition. They differed significantly based on comorbidities like irritable bowel syndrome, obesity and hypertension. Antibiotic use within the past 30 days did not seem to have an effect on the types of bacteria detected on the stents.
“While more research is needed, our study suggests that antibiotic use during the placement of these stents could one day be more conservative or targeted based on each patient’s condition,” says Dr. Jeremy Burton, Lawson Scientist and Associate Professor at Schulich Medicine & Dentistry.
The team also discovered that in patients needing multiple stents, the bacterial community remained stable over time, suggesting that infections on a patient’s previous stent could direct the course of treatment for their future device placements.
“This is the largest study of its kind, investigating bacteria both in urine and adhered to ureteral stents,” states Dr. Hassan Razvi, Urologist at St. Joseph’s, Lawson Associate Scientist and Professor at Schulich Medicine & Dentistry. “We hope this will be the first step towards personalized care, ultimately leading to fewer stent-associated infections.”
The study was made possible through the generous support of The W. Garfield Weston Foundation and St. Joseph’s Health Care Foundation.
-30-
DOWNLOADABLE MEDIA

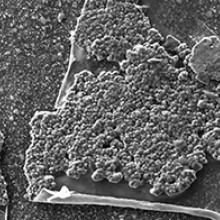
Scanning electron microscopy images showing organic material, crystals, and bacteria present on the surface of the ureteral stents.
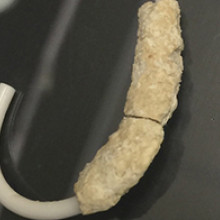
Recovered ureteral stent encrusted with minerals and bacteria.
See all Lawson Media Releases
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New urinary microbiome study could be first step in providing personalized care to patients with ureteral stents
For patients with kidney stones, ureteral stents (hollow devices placed in the ureter – the tube between the kidney and bladder) can be used temporarily to relieve urinary obstruction. Despite the use of antibiotics, ureteral stents often become encrusted with minerals and coated with bacteria. This can lead to complications like infection and the need for replacement surgery.
Published today in Cell Reports Medicine, researchers at Lawson Health Research Institute and Western University conducted a novel microbiome study to examine bacteria associated with ureteral stents. They found that nearly all the stents, whether visibly coated or not, had unique bacterial profiles that were most associated with a patient’s medical condition rather than antibiotic use. For patients with ureteral stents, they may benefit from a personalized approach to care and antibiotic treatment.

The study included 241 patients from St. Joseph’s Health Care London. The research team collected and analyzed patient urine samples and ureteral stents following surgical removal, as well as relevant patient information such as antibiotic use and history of infections.
“We wanted to know which bacteria were present and whether the bacteria found in urine samples corresponded to the bacteria found on a patient’s stent,” explains Dr. Kait Al, Postdoctoral Fellow at Lawson and at Western’s Schulich School of Medicine & Dentistry. “We found that there was a bacterial community present on almost all stents, even if they were not visibly affected, and that it differed from the bacterial community found in a patient’s urine.”
These findings challenge long-held beliefs that the urinary tract is a sterile environment devoid of bacteria.
The study revealed that the bacteria present were determined by an individual patient’s medical condition. They differed significantly based on comorbidities like irritable bowel syndrome, obesity and hypertension. Antibiotic use within the past 30 days did not seem to have an effect on the types of bacteria detected on the stents.
“While more research is needed, our study suggests that antibiotic use during the placement of these stents could one day be more conservative or targeted based on each patient’s condition,” says Dr. Jeremy Burton, Lawson Scientist and Associate Professor at Schulich Medicine & Dentistry.
The team also discovered that in patients needing multiple stents, the bacterial community remained stable over time, suggesting that infections on a patient’s previous stent could direct the course of treatment for their future device placements.
“This is the largest study of its kind, investigating bacteria both in urine and adhered to ureteral stents,” states Dr. Hassan Razvi, Urologist at St. Joseph’s, Lawson Associate Scientist and Professor at Schulich Medicine & Dentistry. “We hope this will be the first step towards personalized care, ultimately leading to fewer stent-associated infections.”
The study was made possible through the generous support of The W. Garfield Weston Foundation and St. Joseph’s Health Care Foundation.
Dr. Kait Al, Postdoctoral Fellow at Lawson and Schulich Medicine & Dentistry
noteWORTHY – Teamwork and patients inspire clinical research assistant
St. Joseph’s celebrates people who provide exceptional care, grow stronger communities and contribute to a healthier world. Today, meet Heather LaPier, a clinical research assistant whose work helps keep clinical research running smoothly for four Lawson research scientists in diabetes and nephrology. She is a liaison among patients, researchers, clinicians, ethicists, regulatory bodies and pharmaceutical companies.
What values or people inspire your work:
I couldn’t ask for better than the physicians and researchers I work with. It’s a true team. We can bring our own ideas and expertise and know that we’re valued. We’re all good at showing appreciation for each other.
Best part of your workday:
Visiting with people receiving dialysis. They have treatment four hours a day, three times a week, so they’re used to talking with physicians and staff and we get to know them really well. They’re honest and funny – and, despite living with a chronic illness, they’re some of the most positive people I’ve ever met.
What one thing do you wish people knew about your work?
Our job is to advocate for patients and protect them, so every study is carefully designed, planned, regulated and monitored. We work to find solutions to patients’ health issues, and that means putting them first.
One big thing people should know is that participants in clinical trials and research studies get extra care and attention. Other patients have regular appointments, maybe every six months, but as a participant in research they’ll have even more frequent monitoring. So even though they’re helping advance medical knowledge generally and there’s no certainty of direct benefit to them from a specific clinical trial, they do have a whole team of people fully involved in their current care. Any time they have a question, they have direct access to an endocrinologist or nephrologist.
Why this work is meaningful to you:
It’s definitely exciting and always interesting. It can be easy to get caught up in the day-to-day tasks – but I never want to lose sight of the fact patients are living longer and better lives because of the work we’re doing. I have a front-row seat when patients come in for visits and tell us a diabetes treatment or a dialysis intervention is making them feel better.
Back-story:
My mom has been a nurse for over 30 years, so I grew up in a home where we talked about health and patient care a lot. We have a shared language. After my university degree, I applied to college for either forensic science or clinical research. I’m so glad clinical research is where I landed.
One other thing:
I love learning about the history of the Second World War, specifically naval ships and naval battles. It seems totally random, but I studied it as one of my non-science courses in university. I still find it fascinating.
Well said:
Heather is a true gem – highly skilled, creative, and an outstanding team player who expertly manages multiple research projects and investigators. She has been a game-changer for diabetes, metabolic, and chronic disease research at Lawson Research Institute, supporting everything from qualitative studies to large randomized-controlled trials with innovative designs. Our successes wouldn’t have been possible without her.
- Dr. Kristen Clemens, St. Joseph’s endocrinologist and Lawson Research Institute scientist
