Search
Search
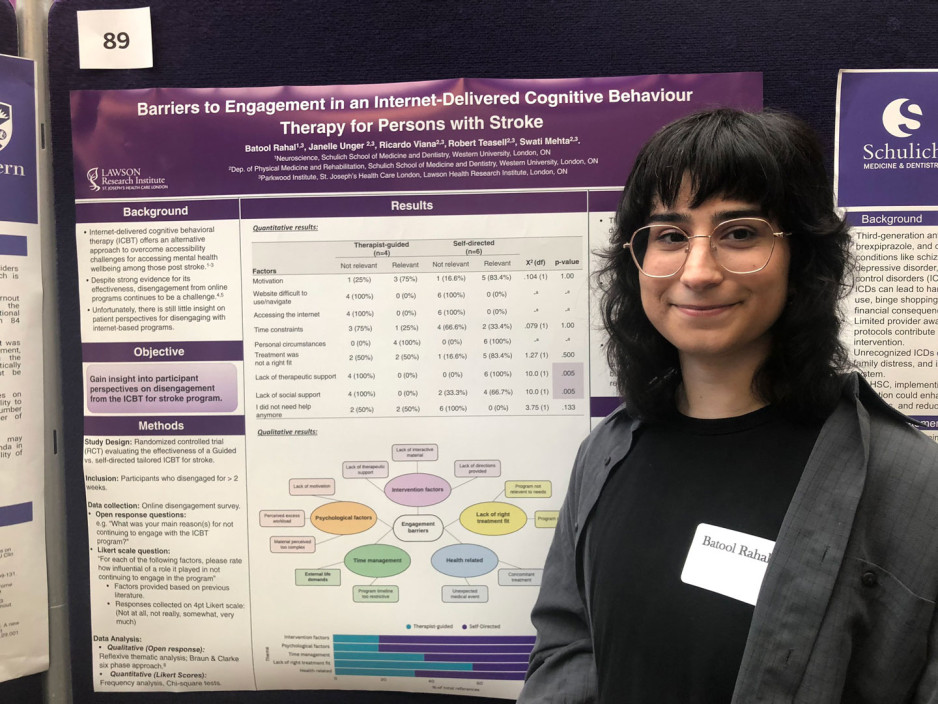
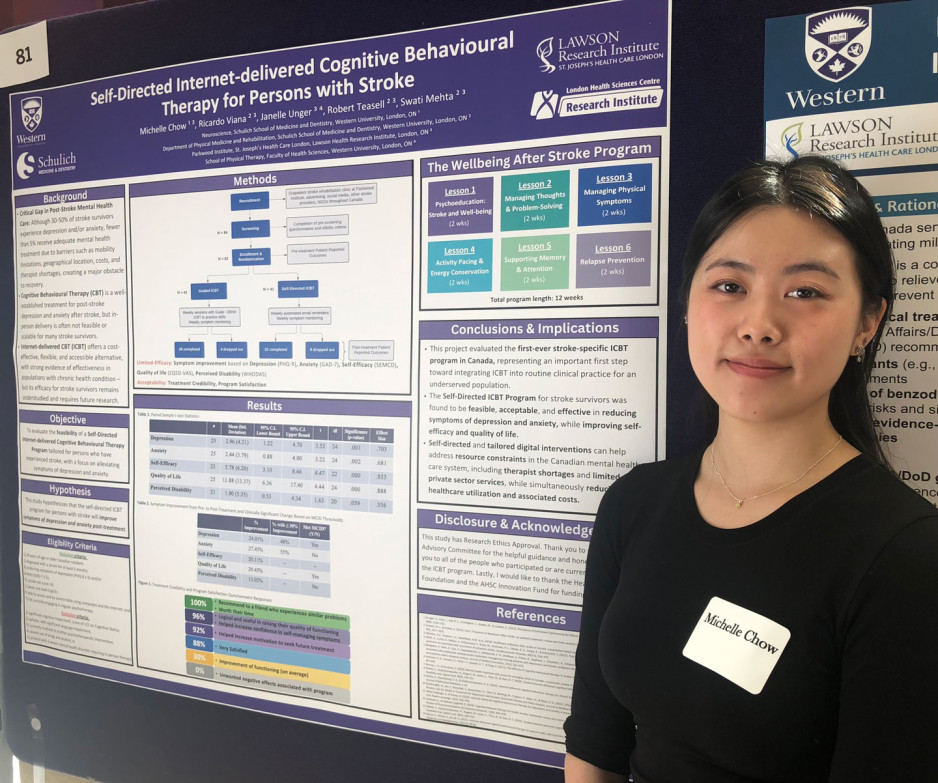
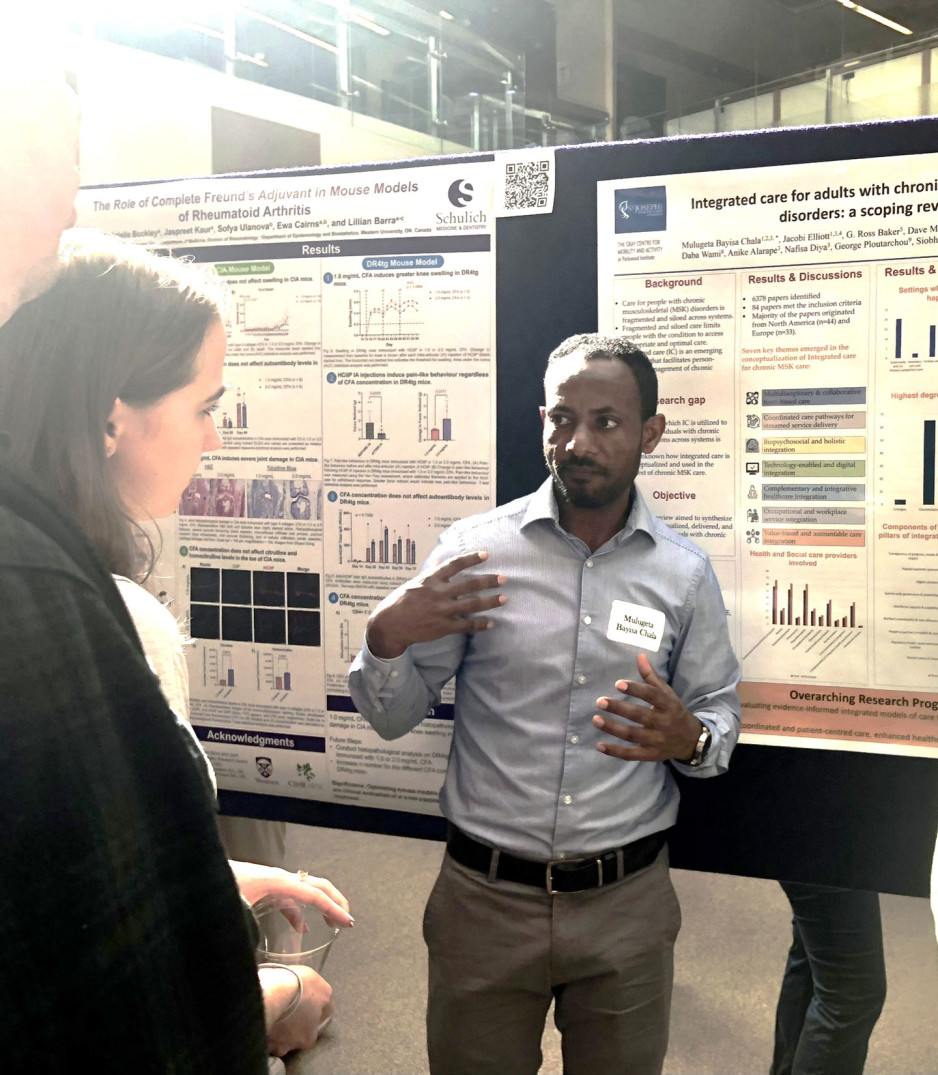
Student innovators showcase work at London Health Research Day 2025
The region’s largest celebration of emerging researchers’ work, London Health Research Day featured oral and poster presentations from undergraduates, grad students, postgraduates and trainees.
They shared their work with peers and globally renowned scientists in an array of specialized health and medical fields.
Their projects were as diverse as concussion treatment for children; large-language models to evaluate cancer diagnoses; brain imaging in people with dementia; and health system change to reduce surgical wait times.
Dozens of projects had Lawson Research Institute connections, included chronic pain’s impact on the brain; self-directed cognitive behavioural therapy for people recovering from stroke; and triaging care for people with shoulder injury.
Participants were also treated to a keynote address by Professor Francesca Ciccarelli, PhD, a global leader in cancer genomics who shared groundbreaking insights into the future of cancer research and precision medicine.
Her presentation was part of the Lucille and Norton Wolf Health Research Lecture Series through the generosity of the Bernard and Norton Wolf Family Foundation.
All told, about 500 people took in the day’s events, including several professional- and career-development workshops.
Student innovators showcase work at London Health Research Day 2025
The region’s largest celebration of emerging researchers’ work, London Health Research Day featured oral and poster presentations from undergraduates, grad students, postgraduates and trainees.
They shared their work with peers and globally renowned scientists in an array of specialized health and medical fields.
Their projects were as diverse as concussion treatment for children; large-language models to evaluate cancer diagnoses; brain imaging in people with dementia; and health system change to reduce surgical wait times.
Dozens of projects had Lawson Research Institute connections, included chronic pain’s impact on the brain; self-directed cognitive behavioural therapy for people recovering from stroke; and triaging care for people with shoulder injury.
Participants were also treated to a keynote address by Professor Francesca Ciccarelli, PhD, a global leader in cancer genomics who shared groundbreaking insights into the future of cancer research and precision medicine.
Her presentation was part of the Lucille and Norton Wolf Health Research Lecture Series through the generosity of the Bernard and Norton Wolf Family Foundation.
London Health Research Day is a shared project of Western’s Schulich School of Medicine & Dentistry, the Faculty of Health Sciences, Lawson Research Institute of St. Joseph's Health Care London and London Health Sciences Centre Research Institute.
All told, about 500 people took in the day’s events, including several professional- and career-development workshops.
Study examines new forms of treatment for those suffering from post-traumatic stress disorder
Researchers looking to better personalize treatment for PTSD
MEDIA RELEASE
For immediate release
January 25th, 2022
LONDON, ON – Post-traumatic stress disorder (PTSD) is a condition that often develops in those who have experienced a traumatic event. PTSD affects close to 10 per cent of Canadians, and in some cases, can be difficult to treat.
In a new study through Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry, scientists are looking at a form of treatment called deep brain reorienting (DBR) for those suffering from PTSD.
“In our study we are looking at ways of trauma processing at the foundation of the stress response,” explains Dr. Ruth Lanius, Associate Scientist at Lawson and Professor at Western’s Schulich School of Medicine & Dentistry. “When you are faced with a stressor the first thing you do is turn your attention to it, and when you do that you engage your head and neck muscles.”
DBR was developed by Scottish psychiatrist Dr. Frank Corrigan and focuses on the muscles of the shoulders, neck, head and face of patients when recalling a traumatic event. This form of trauma processing starts right at the moment the stressor is noticed by the individual, which is often quickly followed by a moment of shock. By addressing the stressor at this level, doctors can target the foundation of where the stress response begins.
“When patients bring up a trigger in their mind, we look at what happens in terms of the tension in their head and neck. We process that gently by asking the patient to notice and stay with that tension without trying to release it, and over time the tension usually decreases,” explains Dr. Lanius, who is also a Psychiatrist at London Health Sciences Centre. “The second part involves addressing the shock response. You turn your attention to the stressor and then notice any moments of shock that follows, which is often associated with tension behind the eyes and in the shoulders. Finally, you address the visceral sensations associated with feelings and emotions associated with the stressor.”
Dr. Lanius believes that by using DBR and focusing on muscle and visceral responses, it will help patients suffering from PTSD to process the visceral feelings associated with the trauma and its triggers.
“After this form of treatment, patients often say they feel safer and don’t see themselves negatively, like they did in the past,” says Dr. Lanius. “This is because we change those intense visceral feelings and it allows the person to reevaluate who they are and how they interact with the world.”
The research team is hoping to recruit approximately 60 people to take part in the DBR study. Participants will undergo a psychological interview and an MRI, then eight sessions of treatments. Following those sessions, participants will have another interview and MRI to assess if any positive changes were made within the neurological networks and/or in psychological systems.
“Our hopes are to really personalize treatment for those living with PTSD,” says Dr. Lanius. “Some people have difficulty tolerating some forms of trauma processing and in my experience this treatment is a gentler approach for those individuals.”
Interested participants who have been diagnosed with PTSD can contact Suzy Southwell, Research Coordinator, at 519-685-8500 ext. 35186 or @email.
MEDIA CONTACT
Celine Zadorsky, Communications & External Relations, Lawson Health Research Institute, T: 519-685-8500 ext. 75664, C: 519-619-3872
ABOUT LAWSON HEALTH RESEARCH INSTITUTE
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world.
ABOUT WESTERN
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
ABOUT THE SCHULICH SCHOOL OF MEDICINE & DENTISTRY
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study finds children in marginalized communities more likely to experience cardiac arrests
A new study shows children living in marginalized communities are at a higher risk of experiencing paediatric out-of-hospital cardiac arrest (POHCA) – a rare, life-threatening event occurring outside a hospital setting in which a child’s heart suddenly stops beating. It is estimated in other studies that the survival rate for POHCA is less than 10 per cent, and one-third of the children who survive POHCA will develop a significant neurological condition.
A province-wide case-control study from Western University, Lawson Health Research Institute and the Institute for Clinical Evaluative Sciences (ICES) addressed a gap in current literature related to how social determinants of health impact the risk of POHCA. The study was published in the Journal of the American Heart Association.
“We know the outcomes for children who experience POHCA are really poor. Most don’t survive, and those who do often develop new and severe neurological impairments,” said lead author Samina Idrees, an epidemiology and biostatistics Masters graduate, who completed the work while studying at Western. “Given the significance of this health outcome and its potential preventability, we wanted to investigate further and shed light on any potential disparities.”
The study established that the odds of POHCA were higher for children living in areas with the highest levels of material deprivation – which incorporates average income, education, the proportion of lone parent families and housing quality. The likelihood of experiencing POHCA was also greater for those living in urban centres in Northern Ontario (relative to those in urban centres in Southern Ontario) with a population greater than 10,000, rural areas in Southern Ontario, and in areas with highest levels of unpaid professions, unemployment or non-working age individuals, high levels of instability and lower levels of ethnic diversity.
“Racialized communities sometimes have higher risks for certain health conditions,” said Idrees, in reference to the finding that children living in areas with the lowest levels of ethnic diversity had a higher risk of POHCA. “However, these findings are in line with the finding that immigrants have a lower risk of experiencing POHCA relative to those born in the country, likely due to the healthy immigrant effect, where immigrants arriving in Canada are usually in good health.”
Most cases of POHCA are caused by respiratory failure, and cardiac arrests in children can be attributed to a wide range of preventable and unpreventable factors, including drowning, sudden infant death syndrome, accidental ingestion or existing medical conditions.
Dr. Janice Tijssen, senior author on the study, Associate Scientist at Lawson, Professor at Western and Adjunct Scientist at ICES, noted that while there is a variety of factors that may contribute to out-of-hospital cardiac arrests in children, a common theme was that kids living in these marginalized communities are at higher risk of experiencing cardiac arrest.

The case study group included 1,826 children, aged one day to 17 years, who were transported to an emergency department in Ontario after they suffered an out-of-hospital cardiac arrest between April 1, 2004 and March 31, 2020. The case study group was matched to a control group on a one-to-four ratio and researchers identified cases of POHCA using the National Ambulatory Care Reporting System – which contains data for hospital-based and community-based ambulatory care.
Solutions to reduce rates of POHCA in marginalized communities
The researchers emphasized that these findings underscore the need to address disparities through targeted prevention and intervention efforts to reduce the odds of POHCA. These include finding opportunities to increase public health education and awareness around POHCA, as well as implementing measures related to social determinants of health such as improving access to health care, health literacy and preventative healthcare.
The study also suggests other ways for communities to help reduce incidents of POHCA, such as improving emergency medical services, providing education to equip more people with cardiopulmonary resuscitation (CPR) skills and improving access to automated external defibrillators (AED).
“Information on how to provide CPR or how to apply an AED is very simple and anyone can learn,” said Tijssen, Associate Professor in the Departments of Paediatrics and Epidemiology & Biostatistics at the Schulich School of Medicine & Dentistry and Medical Director of the Paediatric Critical Care Unit at Children's Hospital at London Health Sciences Centre. “Children as young as six or eight can learn how to respond to a cardiac arrest so it’s crucial to get out to these communities with this information.”
The team also included Western researchers Kelly Anderson and Yun-Hee Choi.
Study finds high percentage of patients with a severe COVID-19 infection will end up with kidney injury, often fatal
Acute kidney injury associated with severe COVID-19 leads to high mortality rates
For Immediate Release
Severe cases of a COVID-19 infection can cause a host of serious complications, one of them being acute kidney injury. In a recent published study, scientists at Lawson Health Research Institute (Lawson) have found that acute kidney injury in patients with a severe COVID-19 infection is leading to a high mortality rate.
“These are patients who did not have kidney disease, or kidney injury prior to contracting COVID-19,” explains Dr. Peter Blake, Lawson researcher and Provincial Medical Director at the Ontario Renal Network. “This is what we call acute kidney injury, and in the case of these severe COVID-19 patients the kidney injury led to the need for acute dialysis.”
By accessing data collected through the Ontario Renal Network (ORN), Dr. Blake and his colleagues were able to examine 271 people at 27 renal programs across the province, including patients at London Health Sciences Centre (LHSC), who received acute dialysis for acute kidney injury due to a COVID-19 infection. The data examined was from the duration of the first two waves of the pandemic, up to January 31st, 2021.
“This is a complication that is occurs in 10 per cent of ICU COVID-19 cases,” says Dr. Blake, who is also a nephrologist at LHSC. “Men accounted for more than 75 per cent of this condition, half of the patients were diabetic and the majority of these patients were not seniors in the later stages of life, but rather middle-aged people.”
The provincially-collected data through the ORN also showed that patient populations living in postal codes with high ethnocultural deprivation were more likely to get this condition, at a rate of more than 60 per cent, and survival rates were not promising.
“The mortality rate was shockingly high with 64 per cent of these patients dying within 90 days,” adds Dr. Blake. “Many of those who survived remained in hospital for a long period of time and the one in five that did survive have remained on long-term dialysis.”
This study has been published in the Clinical Kidney Journal. Looking ahead, the research team plans to follow up with patients who have survived this severe complication to track what lasting health affects occur within a six-to twelve-month post-survival period.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study offers hope for hard-to-treat type 2 diabetes
A landmark international study involving patients and researchers at St. Joseph’s Health Care London shows automated insulin pump delivery can be ‘life-changing’ for people with type 2 diabetes
Lisa Mercer had tried just about everything to regulate the ups and downs of her blood sugars, from a strict diet to medication to four-a-day-day insulin shots.
But her busy life with type 2 diabetes finally started to feel better when she enrolled in a clinical trial at St. Joseph’s Health Care London to test the effectiveness of a system that combined glucose monitoring with an automated insulin pump.
“It was life-changing for me. I was diagnosed with type 2 diabetes 25 years ago and my blood sugars have always been all over the map. I felt sort of helpless. I said yes to this clinical trial because I hoped it would return some normalcy to my life,” she says. Now that study, with results newly published in the prestigious New England Journal of Medicine, is being heralded as a big step forward for patients with hard-to-treat type 2 diabetes.
“This is an exciting finding because it shows we can improve patients’ blood sugars and hopefully prevent long-term negative consequences of high sugars while at the same time making it easier for patients to manage the disease,” says Dr. Tamara Spaic, Medical Director of St. Joseph’s Diabetes Education Centre and the lead Canadian researcher for the multi-site international study based at the Jaeb Center for Health Research in Tampa, Fla.
Study participants were placed either in a group testing the effectiveness of a new system called Control IQ+ or a control group continuing their existing diabetes management regimen.
The intervention group wore glucose monitors that electronically talked with high-tech pumps that delivered insulin – automatically, in the right dose and at the right time – with minimal patient input.
While the device was approved about five years ago for people with type 1 diabetes, this is the first examination of its effectiveness managing the complexities of type 2 diabetes.
“The biggest burden in diabetes control is that it’s 24/7 vigilance: did I eat or not; what did I eat and how much; did I exercise; do I need to wake up for an insulin shot in the middle of the night? This system largely removes those variables to bring blood sugars to target levels,” says Spaic, who is also a Lawson Research Institute scientist and professor of endocrinology and metabolism at Western University’s Schulich School of Medicine & Dentistry.
“What surprised us was that this worked so well across all populations regardless of duration of the disease, amount of insulin needed, whether they used other medications or not, whether they were tech-savvy or not. It worked for everyone regardless of their ethnicity, socioeconomics, and whether they were male or female, old or young,” she adds.
Researchers even asked participants in the intervention group to skip insulin with meals on occasion – generally a no-no in the highly regimented life of someone with insulin-managed diabetes – and the automated system responded appropriately and quickly to adjust blood sugars.
Mercer found improvement within a couple of weeks: “Before the pump, I felt awful. When my sugars were too low, I got the shakes, I had trouble communicating and thinking clearly and I got extremely tired. When my sugars were too high, I was exhausted. It dominated every day and was tough on my job as a police officer. Now I feel better. I feel more in control.
“Is it perfect? No. But my sugars are stable and consistent more often than not.”
Not yet approved in Canada
In February, the US Food and Drug Administration cleared the use of the Control IQ+ system in adults with type 2 diabetes – approval that also meant the expense could be covered through health insurance.
However, it has not yet been brought to Health Canada regulators for approval, Spaic says.
Even so, several of her patients, including Foster, decided to continue using the system after the 13-week trial, paying out-of-pocket or through private insurance.
Spaic and St. Joseph’s colleagues, endocrinologist Dr. Selina Liu and nurse coordinator Marsha Driscoll, were extensively involved in the design of the study, recruiting and monitoring participants and reporting results.
Diabetes type 2 usually develops in adulthood and is a condition in which body cannot make enough insulin or does not properly use the insulin it makes to regulate the amount of glucose (sugar) in the blood.
While most people with type 2 diabetes can control their blood sugars through lifestyle changes or with new treatments such as non-insulin glucose-lowering medications, the sub-set of North Americans who require insulin still numbers in the millions.
THE STUDY:
What: 13-week, large-scale clinical trial to test the effectiveness of a system combining automated insulin delivery with continuous glucose monitoring for people with type 2 diabetes.
Who: 319 study participants – including 13 at Lawson Research Institute of St. Joseph’s Health Care London – all needing multiple daily insulin doses. Age range 19 to 87, from 21 centres across the U.S. and Canada. Study led by Jaeb Centre for Health Research in Tampa, Fla., and funded by Tandem Diabetes Care, which also provided the automated insulin-delivery systems
How: Two-thirds of patients received an automated insulin pump, continuous glucose monitor and transmitter to track and automatically administer insulin to regulate their blood sugars. A control group continued their existing insulin-delivery method and also received glucose monitors.
Results: The intervention group had more stable blood sugar levels – with 3.4 more hours per day in the target glucose range – than the control group. Use of automated insulin devices was successful and safe even for patients without previous experience with an insulin pump
Why it matters: Automated insulin delivery can help insulin-dependent patients manage their type 2 diabetes better than before. Better management means improved quality of life and may result in fewer diabetes complications such as heart disease and damage to the eyes, kidneys and nerves.
Study to examine health impacts of the COVID-19 pandemic for mothers and their new babies
LONDON, ON - The COVID-19 pandemic has drastically altered many people’s lifestyles. Parents may be working from home, providing additional childcare or experiencing social isolation. Some are dealing with decreased work hours and loss of employment. With all these factors at hand, a team of researchers from Lawson Health Research Institute and Western University are investigating the possible health impacts on mothers and their babies who were born or will be born during the pandemic.
“This has been a stressful and pivotal time for everyone in the world, but we know the post-partum experience can greatly affect both the birthing person and their baby, in the short and long term,” says Dr. Genevieve Eastabrook, Associate Scientist at Lawson and Assistant Professor at Western’s Schulich School of Medicine & Dentistry. “We know perceived stress in the perinatal period may have a contribution to health later in life for the birthing person and their children in terms of overall cardiovascular and metabolic health, bonding experiences, and risk of mood disorders.” Dr. Eastabrook is also an obstetrician-gynecologist (OB-GYN) at London Health Sciences Centre (LHSC).
As part of the new study, the London research team is using an approach called ‘One Health’ which offers a holistic perspective to explore how various risk factors and social determinants of health interact to affect health. This is being studied through the Department of Pathology and Laboratory Medicine at Western. “It’s important for us to think of the environment as all of our surroundings, including the things around us like health care, grocery stores, education and employment,” says Mei Yuan, MSc research student at Schulich Medicine & Dentistry. “The purpose of this study is to look at the pandemic response rather than the pandemic itself. We know that even if women haven’t been infected with COVID-19, it doesn’t mean they haven’t been impacted.”
Study participants are asked to complete a 30-minute questionnaire at around 6-12 weeks after their delivery. The questionnaire focuses on perceived stress, postpartum depressive symptoms, perceived social support, the impact of COVID-19, health-care access and breastfeeding. Data from the questionnaire will be linked with participants’ medical records to look for associations between the various factors and pregnancy outcomes. “Even though the study is mainly focused on maternal health, studies have shown that once mental health is affected it really does impact the infant’s health, especially in the area of attachment between baby and caregivers,” explains Yuan.
Data from the study will be compared to the Maternity Experiences Survey, a national survey of Canadian women compiled in 2007 which looked at experience, perception, knowledge and practice during pregnancy, birth and the early months of parenthood. “The unique aspect here is that we have a comparative group using a historic cohort to see whether or not there are differences in markers that increase risk of depression, perceived stress and lack of social support,” adds Dr. Eastabrook. “We will also look at some unique things from the pandemic, such as how the use of virtual care for antenatal, postpartum and baby care impacted people’s experiences.”
The research team hopes to recruit 300 mothers for this study who have given birth at LHSC, specifically during the pandemic. Interested participants can email the Pregnancy Research Group at @email. Once all the data is collected the goal will be to use the findings to improve post-partum care for mothers and their babies within this population group.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca