Search
Search
Top 12 research stories of 2022
As the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, our teams impact the lives of people in Ontario, Canada and around the globe with groundbreaking studies, world firsts and translational research that enhances care, health and wellbeing. Here are some of Lawson Health Research Institute’s top research highlights of 2022.
Researchers looking to better personalize treatment for PTSD

In a new study through Lawson and Western University’s Schulich School of Medicine & Dentistry, scientists are looking at a form of treatment called deep brain reorienting (DBR) for those suffering from post-traumatic stress disorder (PTSD). Read more.
Virtual care associated with significant environmental and patient cost savings

A new study by researchers at ICES, Lawson and Western finds that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs. Read more.
Novel test that could easily diagnose blast injury created by local scientists

In a world first, researchers at Lawson and Defence Research and Development Canada have developed a breath test that could be used to diagnose repetitive blast injury – a mild traumatic brain injury resulting from pressure changes that occur during explosions. The device will soon go through clinical trials to validate its efficacy. Read more.
Local researchers using artificial intelligence to lead the way in bedside lung imaging
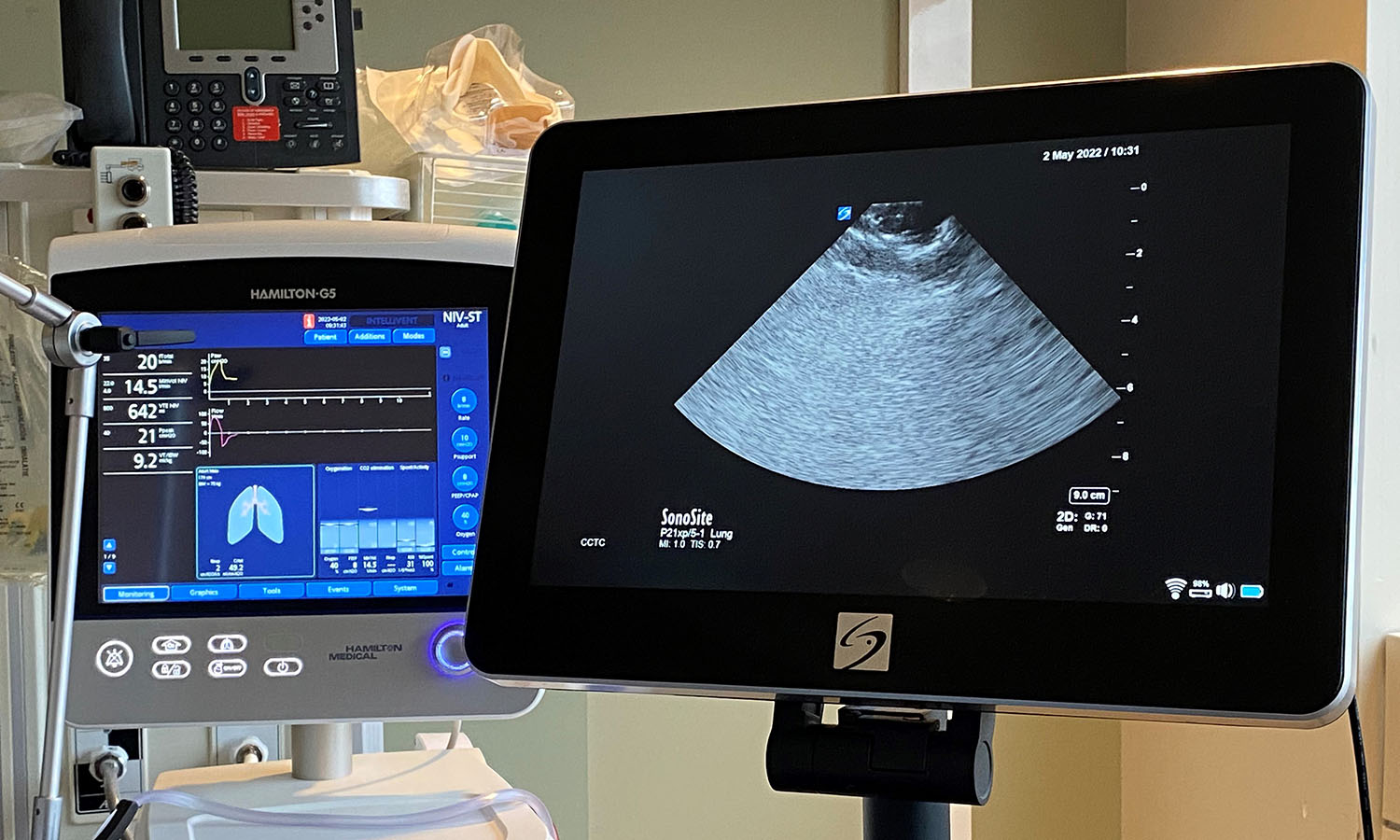
A team at Lawson is testing a new form of artificial intelligence (AI), paired with portable ultrasound machines, to image and identify lung concerns in real time, right at the beside of critically ill patients. Approximately 100 critical care patients at LHSC will be part of this study. Read more.
New tool shows promise in helping people manage traumatic brain injuries one pace at a time

A team at Lawson has developed a new app called MyBrainPacer™ which aims to better assist and treat those living with mild traumatic brain injuries (mTBI), including concussions. mTBI may come with lasting effects that can alter a person’s life. Although a person with a mTBI may appear fine on the outside, many have to pace their day-to-day activities in order to allow the time needed for the brain to properly heal. Much like point tracking used by dieters to monitor food choices, through MyBrainPacer™ App, users can assign values to tasks like driving, grocery shopping, screen use and exercise so they can plan and pace their daily activity. Read more.
Study shows a decline in Veterans' mental health throughout the pandemic

When it comes to mental health conditions, Veterans are an at-risk population, often having higher rates of depression and post-traumatic stress disorder (PTSD). When the COVID-19 pandemic hit, scientists at Lawson wanted to understand its effects on this already at-risk population. They found that more than half of Canadian Veterans reported a decline in their mental health. Read more.
Growing evidence that PSMA imaging improves prostate cancer detection
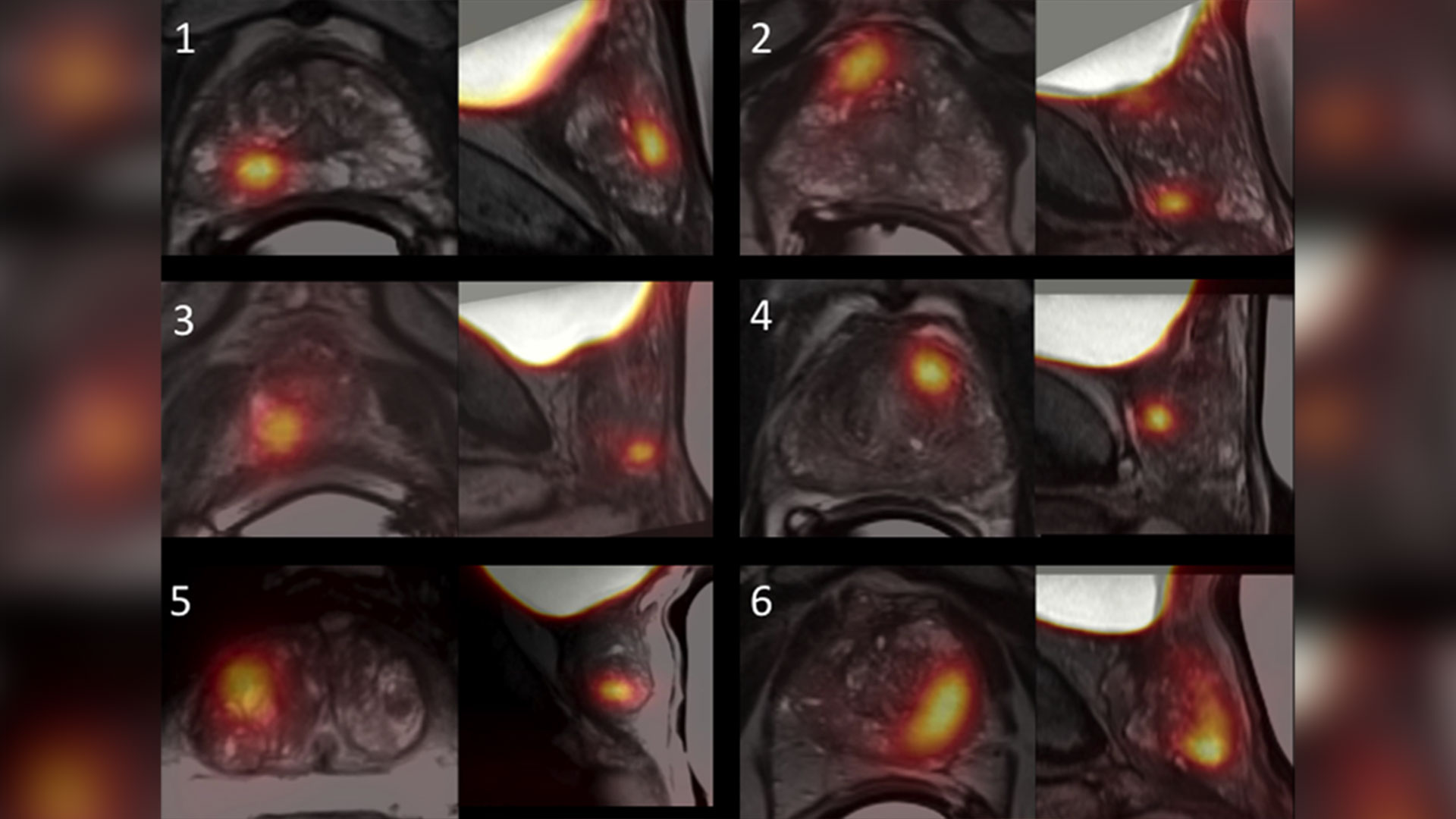
Scientists at Lawson are leading the way in using specialized imaging to detect prostate cancer – the fifth leading cause of cancer death in men around the world. Early evidence indicates that PSMA PET scans have changed how prostate cancer is being treated, but more work is underway to understand the impact of those treatment changes. Read more.
Leveraging virtual reality to manage pain in paediatric patients

A study underway through Lawson and Children’s Hospital at LHSC is using virtual reality (VR) to help paediatric patients during painful and distressing procedures. The study is focusing on paediatric patients who need port access. A port is a little reservoir that sits underneath the skin that allows access to blood or medication with the use of a needle. Ports are most commonly used in paediatric cancer patients. Read more.
Team players: FMT and microbiome research could have widespread impact

There is still much to learn about the human microbiome and its role in fighting disease, but ongoing studies at Lawson, including a focus on fecal microbial transplants (FMT), are making strides in harnessing this complex system. FMT is being studied in connection with conditions as varied as non-alcoholic fatty liver disease, rheumatoid arthritis, atherosclerosis, HIV, cancer and multiple sclerosis. Read more.
London researchers adapt MRI technology to image salt within the kidneys

Scientists at Lawson have adapted PET/MRI technology to accurately image salt within the kidneys of patients with kidney disease. Imaging salt within the kidneys has never been accurately accomplished in patients with kidney disease, but Dr. McIntyre and his team developed new technology and software that was adaptable to a PET/MRI machine at St. Joseph’s. Read more.
London researchers discover novel method to diagnose long COVID
Published in Molecular Medicine, researchers at Lawson have found that patients with post-COVID-19 condition (long COVID) have unique biomarkers in their blood. The team is now working on developing a first of its kind blood test that could be used to diagnose long COVID. The discovery could also lead to new therapeutics for this condition. Read more.
Largest trial ever done in hemodialysis care examines optimal dialysis temperature

Published in the Lancet findings from a large clinical trial through Lawson, ICES Western and Western University suggest that lowering dialysis temperatures does not lead to improved patient outcomes, despite previous studies suggesting otherwise. Read more.
To learn more about Lawson research studies, please visit our News and Media page
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Using artificial intelligence and brain stimulation to improve treatment for psychosis
Leading the Canadian arm of the project is Dr. Lena Palaniyappan who is using Artificial Intelligence to help personalize treatment for patients with psychosis. Dr. Palaniyappan is an Associate Scientist at Lawson Health Research Institute, Associate Professor at Schulich Medicine & Dentistry and Scientist at Robarts Research Institute.

Dr. Lena Palaniyappan who is using AI to help personalize treatment for patients with psychosis.
In collaboration with five European centres, Dr. Palaniyappan and a team at Robarts Research Institute and Lawson Health Research Institute, the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, will be collecting brain scans and genetic information from more than 60,000 patients in order to understand the relationship between genetics and brain development.
“The study itself involves collecting neuroimaging and genetic information from multiple sites in order to understand the mechanisms of mental illness,” said Dr. Palaniyappan. “The translational portion of this is applying this information to clinic. How genes and brain networks interact to cause mental disorders, and how we can use this information to match patients to specific treatment choices.”
The group is specifically studying a treatment called magnetic stimulation which will be delivered within the mental health care program at St. Parkwood Institute, a part of St. Joseph’s, in collaboration with Dr. Amer Burhan. Dr. Burhan is a Lawson Associate Scientist, Associate Professor at Schulich Medicine & Dentistry and Clinical Physician Lead for Therapeutic Brain Stimulation (ECT and TMS) at Parkwood Institute.

Dr. Lena Palaniyappan is collaborating with Dr. Amer Burhan for this study.
The treatment uses focused magnetic pulses that stimulate a specific group of neurons. Dr. Palaniyappan says the treatment is very effective, but only in one-third of patients.
“We want to know if there are clear markers that show who will respond to this treatment, and who will not. This will help reduce the burden of failed treatment trials for this challenging illness,” said Dr. Palaniyappan.
To enable this, the researchers will look for patterns in a very large amount of imaging and clinical data collected in Europe and Canada. That’s where Artificial Intelligence comes in. In order to understand the patterns that are clinically useful, they use a technique called Machine Learning that trains a computer to recognize expected patterns and then make predictions for new patients.
The data is being collected from six centres, coordinated by Dr. Emanuel Schwarz at the University of Heidelberg, Mannheim, Germany. In addition to the centre here in London, Ontario, other partners include Munich, Germany; Oslo, Norway; Rotterdam, Netherlands; and Montpellier, France.
The research project will also mean that this form of magnetic stimulation treatment will be offered for psychosis patients in London for the first time.
“Magnetic brain stimulation is a safe and well-tolerated treatment that is used currently in London to treat depression, but now we will be able to offer this to patients with psychosis as well,” said Dr. Palaniyappan.
The project will begin in May 2019 and will continue until the end of 2022.
View St. Joseph’s Health Care London's 2017-2018 Annual Report
St. Joseph’s Health Care London’s 2017-2018 Annual Report features stories about patients and residents, and their journey of care and recovery.
The following research is highlighted in the 2017-2018 Annual Report:
- Smart tech, smart treatment: Many mobile applications are on the market to help people struggling with mental health issues, but these aren’t necessarily created or used by health care providers. Creating an entire smart mental health system is one of the strategic priorities of St. Joseph’s and Lawson’s Mental Health Research Group led by Dr. Cheryl Forchuk, Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery. Numerous projects have been identified as components of a plan spanning seven years.
- Walking while talking a possible early predictor of dementia: In a new study, researchers at Lawson and Western University are demonstrating that gait, or motion testing, while simultaneously performing a cognitively demanding task can effectively predict the progression to dementia and eventually help with earlier diagnosis. To date, there is no definitive way for health care professionals to forecast the onset of dementia in a patient with memory complaints.
Walking the labyrinth: A path for meaning, insight and reflection
At Southwest Centre for Forensic Mental Health Care (Southwest Centre) in Elgin County, the unique story of every individual is honoured as care practitioners assist in the journey toward recovery. Part of the St. Joseph’s Health Care London family, Southwest Centre is devoted to caring for people with a mental illness who have also come into contact with the criminal justice system.
A new study by Lawson Health Research Institute shows that the use of labyrinths contributes to recovery by promoting spiritual self-care, insight development and personal meaning-making reflection. The research was co-authored by Lawson Allied Scientist and Certified Spiritual Care Practitioner at Southwest Centre, Stephen Yeo, along with his colleagues Dr. Clark Patrick Heard and Jared Scott, both Lawson Associate Scientists and Occupational Therapists.
“Research has demonstrated that labyrinth-walking can result in increased focus and calm, along with a reduction in blood pressure and stress,” explains Yeo. “Additionally, labyrinth-walking is narrative-driven and highly constructivist in nature, which promotes the opportunity for one to critically reflect on his or her unfolding story.”
This can be done in solitude or a trained facilitator can support important narrative reflection and invite opportunities for integration.
The process of reflecting and making meaning helps individuals to think about what they observed or did, why it mattered and how they might think or act differently based on new knowledge. This allows them to set goals and use what they’ve learned from the past to inform future action, and to consider the real-life implications.
Participation supports patients as they cope with mental illness, and the impact is magnified for individuals who have come into contact with the criminal justice system. Their experience can increase existential questions along with spiritual pain and distress.
Even in the most complex and difficult circumstances, walking the labyrinth facilitates a variety of coping approaches including:
- stress reduction and mindfulness;
- understanding one’s awareness of relationship with that which is sacred to them (transcendence) and the environment;
- development of ongoing personal narrative and meaning-making; and,
- kinesthetic prayer and meditation.
Unlike mazes that are like puzzles with many choices of path and direction, labyrinths are created using continuous lines and are easier to navigate with one route to and from the centre. There are two permanent labyrinths at Southwest Centre – one indoors and one outdoors. For the most part, the labyrinths are accessible for self-guided walking and, throughout the year, various group opportunities are scheduled for invited participation. This activity can be continued in the community, as there are labyrinths in various places across the province such as parks, faith communities and other health-care settings.
“Labyrinth participation supports themes related to hope, coping, resiliency, autonomy – all of which are significant contributors to recovery and the maintenance of well-being. Future research in this area could examine the benefits for different patient populations and also for those who reside in the community.”
Labyrinths are trans-religious and their application can be beneficial to religious and non-religious participants. They are also easy to maintain and can be installed in a variety of locations.
Along with his study co-authors, Yeo was honoured with the CASC Group Research Award from the Canadian Association for Spiritual Care. The award recognizes a CASC member who collaborates with other professionals in the research field of spirituality, religion and wellbeing. The recipient supports the core values of professional connection and interdependence, promoting positive relationship with colleagues of various professionals as well as clients.
“Given that this was my first foray into research at this level, I was very humbled to have been nominated for, and to have received, this award,” says Yeo. “I remain especially grateful to the professional guidance and support of my research colleagues.”
“Walking the Labyrinth: Considering mental health consumer experience, meaning making, and the illumination of the sacred in forensic mental health setting” was published in the December 2015 issue of the Journal of Pastoral Care and Counseling. This study is believed to be a first of its kind in a forensic mental health care facility.
Image

|
Left: Photo of the indoor labyrinth at the Southwest Centre for Forensic Mental Health Care. |
Wide range of research showcased at Parkwood Institute Research's 2017 Spring Update
Lawson researchers at Parkwood Institute, part of the St. Joseph’s Health Care London family, work to improve both physical and mental health care based on the understanding that conditions of the body and mind are integrally linked. From studies on mobility after brain and spinal cord injury to treatment-resistant depression, a range of different research areas were highlighted on April 21, 2017 at Parkwood Institute Research’s 2017 Spring Update Half-Day event.
Parkwood Institute Research is a Lawson program that represents inter-disciplinary clinical research. At the second annual Spring Update event celebrating this work, attendees learned about research from across Parkwood Institute’s three core research themes: Cognitive Vitality & Brain Health, Mobility & Activity, and Mental Health Care. New this year was the addition of poster presentations, which provided another opportunity for researchers and trainees to promote and share their work.
Learn more about the work Lawson scientists at Parkwood Institute presented at the event:
Cognitive Vitality & Brain Health
Dr. Stephen Pasternak was one of the presenters in the Cognitive Vitality & Brain Health theme. Dr. Pasternak and his team are conducting a phase 2 randomized controlled trial looking at whether a European over-the-counter cough medicine, Ambroxol, could also treat Parkinson’s Disease Dementia (PDD).
“There are currently no effective treatments for cognitive impairment experienced by PDD patients. Existing treatments only treat the symptoms of Parkinson’s disease, but do not stop the disease process itself,” says Dr. Pasternak.
Parkinson’s disease is believed to be caused by the buildup of a protein called alpha-synuclein in the brain. Ambroxol increases the levels of an enzyme called β-Glucocerebrosidase (GCase), which has been shown to reduce the buildup of alpha-synuclein in animal and cell cultures models, suggesting that this could be used as a treatment for PDD.
This trial is well underway and the first participants have completed the first year of treatment. If successful, this trial will be the first to demonstrate that it is possible to change the underlying cause of PDD.
Mobility & Activity
As part of the Mobility & Activity themed presentations, Dr. Dalton Wolfe discussed an initiative supported by the St. Joseph’s Health Care Foundation and Ontario Neurotrauma Foundation to help improve mobility in patients with acquired brain and spinal cord injuries.
Called the Parkwood Program for Rehabilitation Innovations in Movement Enhancement (PRIME), a key goal of this initiative is to develop and implement a clinical decision support system that integrates approaches to activity-based therapy. Clinicians, researchers, administrators and IT specialists have combined their efforts to initiate development on this system.
“PRIME will provide recommendations for treatment based on patients’ injury level and type, and clinical characteristics,” says Dr. Wolfe. “It will also have suggestions for what to monitor for each patient to challenge them to optimize recovery, as well as to reduce risk of injury or secondary complications.”
This system will also enable electronic tracking of practices and outcomes, moving away from the current paper-based model and creating a practice-based research platform.
Mental Health Care
Dr. Amer Burhan presented his research on Transcranial Magnetic Stimulation (TMS) in the Mental Health Care portion of the presentations. TMS is a non-invasive method that uses magnetic fields to stimulate nerve cells in the brain. An electromagnetic coil is held against the head and short magnetic pulses are administered, causing a change in activity level in specific targeted areas and allowing for a study of the function and interconnectivity of the brain. The method has been approved to treat depression resistant to medications and has potential to be used to treat other mental and neurological disorders.
Dr. Burhan’s talk focused on the effectiveness of a certain type of TMS, bilateral theta-burst stimulation, in treating patients with depression who are not responsive to medication. This is a new method of TMS that is designed to facilitate change in brain activity and connectivity more efficiently. He presented preliminary results on the first 60 patients treated with this method. So far the treatment has resulted in significant improvement in over half of the patients.
“More studies are planned to understand predictors of response and facilitate individualized selection of treatment for patients struggling with this very disabling illness,” says Dr. Burhan.
Women with complications after pelvic mesh implants at increased risk of depression and suicide
Dr. Blayne Welk, a urologist at St. Joseph’s Health Care London, noticed that some of his patients were experiencing depression and other issues following complications related to pelvic mesh-based slings.
“A lot of patients were very emotional telling their story,” notes Dr. Welk.
“They told me about a lot of frustrations related to treatment options for complications. A lot of patients manage for years with problems and didn’t know the source of the issue, or that there is something that can be done to address it. Unfortunately, there are some cases where we can’t fix all the complications, but there are things that we can do to improve the situation. I think a lot of women get frustrated along the journey of finding that solution.”

Dr. Welk is also an adjunct scientist with ICES, associate scientist at Lawson Health Research Institute and assistant professor at Western University’s Schulich School of Medicine & Dentistry. Following his observations in the clinic, he led a research project to study the impact of the complications some women were facing.
“There have been regulatory warnings and lawsuits related to significant transvaginal mesh complications. We wanted to quantify the serious psychological complications that can occur in women as a result of complications from transvaginal midurethral slings,” said Dr. Welk.
Complications are rare but when they happen they can be difficult and challenging to fix, as well as quite impactful for patient lives. They can experience chronic pain, new or changing urinary symptoms and erosions where some of the mesh becomes exposed in surrounding tissue.
To determine whether women who experience midurethral sling mesh complications requiring surgical intervention have an increased risk of depression or self-harm behaviour, Welk's team tracked the number of Ontario women who needed a follow-up surgery to remove or fix a mesh implant and if they received treatment for depression or self-harm. The study, published in the journal JAMA Surgery, included almost 60,000 women who had the procedure January 2004 through December 2015.
The researchers found that 2. 8 per cent (1586 women) underwent a surgical procedure for a mesh complication. Of those women, 11 per cent (175 women) were treated for depression compared to eight per cent of women (4,470) who didn’t have corrective surgery. Of the women who needed corrective surgery, 2.77 per cent of women suffered from self-harm behaviour compared to only 1.15 per cent of women who did not need corrective surgery. These risks were highest in younger women, in particular those 46 years old and younger.
“Younger women are the ones who are most at risk of these mental health complications. We suspect that’s because of a stronger negative association between the complications and intimacy among this age group. They are also more likely to still be working full-time and raising children.”
The study reinforces some of the consequences that can occur from slings, and that those can be quite serious.
“It is important to note that a lot of women are going into these operations to improve their quality of life. It’s not necessarily a dangerous condition when you have stress incontinence. There is a decision made to treat it. I think that in those rare cases when someone does experience severe complications, it can lead to decisional regret.”
There is often not an easy solution, with patients often requiring multiple different therapies to address the complications. This can include pain management, surgery, consultations with pain specialists and psychological support along the way. In some cases, removing the mesh does not resolve the pain and it can be very difficult to identify which individuals will benefit from what therapy, including surgery, notes Dr. Welk.
The researchers add that when women experience midurethral sling complications, both they and their surgeons should be aware of the potential serious psychological impact of these complications.
Author block: Blayne Welk, Jennifer Reid, Erin Kelly, You (Maria) Wu.
World Labyrinth Days highlight how this form of ‘walking meditation’ can benefit everyone
Following a labyrinth is a spiritual practice that’s good for body, mind and spirit.
It leads to increased calm, reduced blood pressure and stress, and improved mental health and well-being, say researchers and patient care experts at St. Joseph’s Southwest Centre for Forensic Mental Health Care (Southwest Centre).
On World Labyrinth Days - May 3 and May 4, staff, patients and residents at St. Joseph’s are invited to join thousands across the globe who “walk as one at 1 pm.”
While books and movie culture often show labyrinths as places where people get hopelessly lost, ground-breaking studies conducted through Lawson Health Research Institute show labyrinths can be just the opposite: they’re places people can find hope and find themselves.
Unlike mazes that are puzzles with many choices and many dead ends, labyrinths have continuous lines that lead to and from the centre.
“Walking a labyrinth is a form of walking mediation,” says Rev. Stephen Yeo, spiritual care practitioner at Southwest Centre and a Lawson researcher. “It is a wonderful way to look after one’s body, mind and spirit. It is a very inclusive practice, regardless of how you engage the sacred in your life and in the world.”
There are two permanent labyrinths at Southwest Centre – one indoors and one outdoors. In addition, this spiritual tradition is available at all St. Joseph’s sites. The Parkwood Institute Mental Health Care Building has an indoor labyrinth in the Multifaith Room and an outdoor labyrinth as well—all of them suitable for people who walk or wheel.
In addition, Mount Hope and St. Joseph’s Hospital each have finger labyrinths available for meditation in their multifaith rooms. Other labyrinth opportunities exist across sites including an opportunity to walk a portable labyrinth at the Parkwood Institute Main Building in the Multifaith Room every Friday at noon.
Southwest Centre in Elgin County also has a portable labyrinth, with lines painted on canvas, that’s often used at other locations. “Have labyrinth, will travel,” Stephen quips.
For nearly a decade, he has facilitated walking labyrinths at Southwest Centre with larger groups during seasonal times of solstice and equinox, as a purposeful step that’s also part of truth and reconciliation practices with Indigenous peoples.
“While it may be world labyrinth day this weekend, it’s labyrinth day here at Southwest Centre regularly as something that’s incorporated into our care and practice,” Stephen says.
The research team’s work examining the benefits of labyrinth-walking in a forensic mental health care setting has been cited globally.
Says principal investigator Clark Heard, “I see significant benefit in labyrinth-walking in settings such as mental health care facilities, although I would stress that these benefits could also be generalized to any participant in a community setting.”
“Walking a labyrinth is a regenerative and restorative experience that helps people connect with the personally sacred,” says Clark, who is an occupational therapist at Southwest Centre and is an Associate Scientist at Lawson.
They promote self-care, hope, resilience and coping. They help connect people to the spiritual side of themselves and to relationships sacred to ourselves and the environment.
“Our team’s work identified that labyrinth participation can support meaning-making in the most difficult of circumstances, while at the same time making room for important aspects of mental wellness such as the quest for hope and search for meaning,” Clark says.
Stephen first walked a labyrinth three decades ago during a retreat at a monastery in Winnipeg. It became part of his regular practice of engaging the sacred in his life, and he is now a certified labyrinth facilitator.
“A labyrinth is so simple that you don’t need someone to lead you through. Whether it's facilitated or not, a person inevitably benefits from walking one,” he says.
Youth expectations of mental health care differ significantly from reality of care, study finds
In a recent study, researchers at Lawson Health Research Institute and Western University examined the expectations of young adults entering psychiatric treatment at an early intervention program and how those expectations differ from the reality of care. The research team found that young adults hold incorrect assumptions about the mental health care environment, relationships with care providers and the trajectory of psychiatric care.
The study included 20 patients from the First Episode Mood and Anxiety Program (FEMAP) at London Health Sciences Centre (LHSC), a novel outpatient mental health program that combines medication management and talk therapy, generally delivered by the same clinician, to help older teens and young adults with emotional concerns that fall into the categories of mood and anxiety symptoms. The vast majority of patients in the study described feelings of apprehension before entering treatment.
“Expectations and assumptions impact the way youth engage in psychiatric treatment, and their success and satisfaction with treatment,” said Dr. Sarah Armstrong, the study’s first author, a clinician-researcher at Lawson, assistant professor at Western’s Schulich School of Medicine & Dentistry and psychiatrist at FEMAP. “It’s critical that we understand the myths around mental health care so we can work to dispel them.”
The study identified three major misconceptions of patients entering care at FEMAP. The first is that patients expected a cold and unwelcoming care environment. “I thought it was umm…like you go to a psych ward and they like tie you up because they think you’re crazy,” one participant noted. Many patients acknowledged that this myth, a caricature of psychiatric care, was strongly influenced by portrayals in popular culture. In reality, they found care providers, staff members and the physical environment at FEMAP to be warm and welcoming which helped to relieve the anxiety around psychiatric care.
Patients also expected an authoritarian approach to care where they would play a passive role. This differed from the reality of care at FEMAP where patients found treatment was a collaborative effort between themselves and their care providers. Patients felt like they had a voice, that their opinions were respected and even felt comfortable disagreeing. They realized they could work towards making effective change for themselves by learning different ways of coping with symptoms and achieving personal goals.
Finally, patients expected quick treatment with an immediate recovery. The reality of treatment was more complicated, more time consuming and required more work than patients originally anticipated. For example, there was often an element of trial and error by using different treatment methods or different medications. Patients found treatment was not straight forward and it took more time than anticipated to see changes in their mental health.
“Ultimately, youth found that treatment at FEMAP was much more complex than they anticipated. However, they experienced a positive change in mindset with a strengthening of personal agency,” said Dr. Armstrong. “Their treatment fears were relieved and they valued their active role in their own care.”
The team hopes this study will be a first step in identifying myths and better preparing youth for the work involved in effective psychiatric care.
“Belief in a positive outcome often leads to better outcomes,” said Dr. Elizabeth Osuch, a clinician-scientist at Lawson, associate professor at Schulich Medicine & Dentistry and medical director at FEMAP. “Young adults are often reluctant to seek mental health care. Expectations can influence whether youth seek help to begin with. These results could help inform educational outreach about psychiatric care, helping to better align expectations with reality. But just as important, this study helps identify what youth value in the treatment provided at FEMAP and what principals would be beneficial to guide health care delivery models for emerging adults.”
The study, “Expectations vs. Reality: The Expectations and Experiences of Psychiatric Treatment Reported by Young Adults at a Mood and Anxiety Outpatient Mental Health Program,” is published in Early Intervention in Psychiatry.
Youth report improved wellbeing as result of tailored mental health services, study finds
In a new study from Lawson Health Research Institute and Western University, researchers partnered with youth receiving care at the First Episode Mood and Anxiety Program (FEMAP) at London Health Sciences Centre (LHSC) to better understand personal perspectives on care and treatment outcomes. The study found that patients experienced lasting improvements in managing their symptoms and improvements in academics, work performance and relationships, and they reported that these benefits involved being empowered by feelings of self-acceptance.
The study included 22 patients from FEMAP, a novel outpatient mental health program at LHSC that provides treatment to ‘emerging adults,’ ages 16 to 25, with emotional concerns that fall into the categories of mood and anxiety symptoms. Treatment at FEMAP takes a patient-centred approach and the research involved looking at what is meaningful and valuable to patients during their care journey.
“The transition from adolescence to adulthood is challenging. FEMAP employs an innovative model of care tailored to the needs of this complex population,” said Dr. Elizabeth Osuch, a clinician-scientist at Lawson, associate professor at Western University’s Schulich School of Medicine & Dentistry and medical director at FEMAP. “By engaging patients in a reflection of their experience, we can learn how effective the program is from the patient perspective.”
Participants shared their experiences through open-ended interviews with Dr. Osuch’s research team. Interview transcripts were collected and analyzed to determine common themes around treatment and outcomes. These themes were then presented back to the research participants for validation.
The study found that treatment led to development of coping strategies to better manage symptoms. Research participants credited these strategies for better functioning in academics, careers and personal relationships. Challenges in these areas are common among emerging adults and are often stressors that lead to youth seeking mental health care.
Participants characterized their treatment at FEMAP as an important investment in their mental health and wellbeing, and credited a collaborative partnership with their care provider for keeping them engaged in treatment. They appreciated the ease of accessing treatment at FEMAP where they could receive care from a psychiatrist, social worker, addictions counsellor, family counsellor and a psychologist, depending on their needs.
The research found that the complexities of treatment were initially frustrating to patients as they were seeking an “easy fix” to their mental health concerns, but they ultimately appreciated that mental health recovery is a journey. They valued that care providers partnered with them to set long-term treatment goals, choose the best treatment options and provide support both during and between appointments.
“Patients may prefer FEMAP over other mental health services because the care is tailored to emerging adults,” said Justin Arcaro, first author on the study and a former MSc candidate at Schulich Medicine & Dentistry and research associate at FEMAP. “There’s an important balance between recognizing emerging adults’ personal autonomy and their need for comprehensive support.”
Study results demonstrated that through treatment at FEMAP, patients realized they are not alone in their mental health journey which led to improved self-acceptance and self-compassion. Participants reported feeling empowered to create meaningful changes in their lives.
Participants also discussed the decision to seek mental health care in the first place. Many struggled with the decision of whether or not treatment was needed. “This shows a need for targeted campaigns to help emerging adults distinguish between normative feelings and those that indicate a need for help,” said Dr. Osuch.
This study also aligns with other research projects at FEMAP that suggest a need for targeted education campaigns about mental health care as a process with solutions that are not necessarily quick or easy. The research team highlights the importance of these findings in informing future funding decisions and policy around mental health care for emerging adults. The findings emphasize the need for quick engagement with a trusted care provider and an integrated treatment team that can partner with patients to support them while enhancing independent growth and self-acceptance.
The study, “Emerging adults’ evaluation of their treatment in an outpatient mood and anxiety disorders program,” is published in Emerging Adulthood.

Above: Dr. Elizabeth Osuch and Justin Arcaro