Search
Search
Dr. Raymond Kao awarded John McCrae Memorial Medal by Canadian Medical Association
Captain (Navy) Dr. Raymond Kao, a Lawson associate scientist, has been awarded the 2017 John McCrae Memorial Medal by the Canadian Medical Association (CMA).
Dr. Kao has served in various military units as a Medical Officer since 1991 and has been a member of the Canadian Armed Forces since 1977. He has served in Africa and the Middle East. In 2013, Dr. Kao was named Canada’s first Chair in Military Critical Care Research. A major focus of his research has been on improving military trauma care and developing treatments that can be brought to the battle field.
The John McCrae Memorial Medal from the CMA recognizes clinical health services personnel of the Canadian Forces who perform exemplary service and demonstrate compassion, self-sacrifice or innovation beyond the call of duty to benefit the health or welfare of fellow military personnel or civilian populations.
“Receiving this honour is very humbling because one does not achieve anything without the help of others. My work would not be possible without the support of and collaboration with other researchers. This award represents the efforts of all the military physicians and surgeons, nurses, medical technicians, allied health care providers and physicians’ assistants on my deployments who have worked to provide excellent care,” says Dr. Kao, who is also the senior critical care advisor to the Surgeon General, a critical care physician at London Health Sciences Centre (LHSC), and an Associate Professor in the Department of Medicine at Western University’s Schulich School of Medicine & Dentistry.
In 2014, Dr. Kao was part of a military medical team sent to Sierra Leone to help combat the Ebola epidemic. He provided care to affected health care workers and studied prognostic factors to help improve care in future epidemics.
He is currently studying the use of C-Peptide to improve organ dysfunction after traumatic hemorrhagic shock caused by blunt or penetrating trauma. Hemorrhagic shock is treated with fluid resuscitation, or fluid replacement, which can also put stress on the organs. His recent studies have shown that C-Peptide, an insulin connecting protein, has the potential to reduce gut injury and lung inflammation from hemorrhagic shock and fluid resuscitation.
Dr. Kao is also widely recognized for his research on erythropoietin, a hormone produced by the kidneys that stimulates the production of red blood cells and, in turn, haemoglobin. He found that when combined with saline, erythropoietin can improve blood flow and tissue oxygen usage after an injury. Erythropoietin can easily be administered through a syringe and can be used to help stabilize wounded soldiers in the battlefield.
Dr. Vladimir Hachinski receives Canadian Medical Association’s highest honour
World-renowned brain researcher, Dr. Vladimir Hachinski, is named as this year’s recipient of the Canadian Medical Association’s (CMA) F.N.G. Starr Award for his contributions in stroke research and patient care. This prestigious award is the highest available to CMA members and is intended to recognize outstanding and inspiring lifetime achievement.
Dr. Hachinski, Lawson Scientist and Neurologist at London Health Sciences Centre is the co-founder of the world’s first successful stroke unit. Two earlier centres in the United States were deemed unsuccessful and eventually closed. Dr. Hachinski and his colleague, Dr. John W. Norris, applied their knowledge and fresh perspectives, and opened a stroke centre at Sunnybrook Hospital, Toronto, in 1975.
“We had a tremendous team of volunteer nurses, physiotherapists and other professionals who were very keen to have an impact,” explains Dr. Hachinski. “We implemented the A, B, C, protocol which focused on Accurate diagnosis, Balance and homeostasis in the patient’s physiology, and avoiding Complication. Dr. Josephine Somerville pioneered early rehabilitation in the stroke unit.”
At the time, stroke was still commonly misunderstood in medicine, until Dr. Hachinski coined the term “brain attack” in 1993, describing the similarities in urgency of strokes and heart attacks.
Realizing the success of their protocols on stroke patients, Dr. Hachinski and his colleagues also noticed improved outcomes for dementia rates in the stroke patients they saw. There is still no treatment for dementia, however they were confident they could delay onset through similar stroke prevention and treatment protocols.
After several studies on both animal models and humans, Dr. David Cechetto from Western University and Dr. Hachinski discovered that the region of the brain, known as the insula, is involved in regulating the parasympathetic and sympathetic nervous systems - evidence that there is an important connection in how the brain impacts the heart.
Today there are several stroke centres operating in Ontario. “We were able to prove that our model was successful at improving the lives of stroke patients, so the government facilitated the opening of these centres across the province. We can now say that we have improved outcomes not just for individuals, but at a population level, where public health policy has its true impact,” says Dr. Hachinski.
Currently Dr. Hachinski and his team are seeking funding for a nation-wide study to examine stroke and dementia outcomes across the country, including how several environmental factors play a role in the development of stroke and dementia with the aim of preventing both. “Since this research is multi-disciplinary, it is challenging to find a funding agency as most of them tend to invest in very specific fields of research,” he explains. “We are hopeful that someone will recognize the importance of this research, and we will be able to move forward with our study.”
“I am extremely appreciative and proud to be recognized with the F.N.G. Starr Award, however I am just the face of this honour. Behind me stands an amazing team. I feel that my greatest strength is to recognize and work with talent.”
Embracing health research this holiday season
Community members, patients and families, and those working in the health field attended a special open house on November 28 by research groups at Lawson Health Research Institute. Together, they celebrated the holiday spirit and the gift of hope that is made possible through hospital-based research.
A part of St. Joseph’s Health Care London, Parkwood Institute represents the next era in care, recovery and rehabilitation. Across the site, clinical and research teams in different disciplines and specialties collaborate not only with each other but also with patients and families.
“Many people in the community know the high-quality and compassionate care that is supported by the various clinical teams at Parkwood Institute, but aren’t aware of the research happening at this site,” says Dr. Cheryl Forchuk, Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery, and Assistant Scientific Director at Lawson.
“Lawson researchers at Parkwood are tackling important challenges with highly innovative and meaningful solutions that help improve care and quality of life.”
For the past three years, the open house gives guests a more in-depth understanding of hospital-based research and its impact. Dr. Forchuk notes that it is a great chance to talk to the researchers and their teams, and to learn about research in a really fun and interactive way. Guests may also learn about opportunities to participate in studies, as the research teams rely on people in the community getting involved.
There were 12 interactive program displays from Parkwood Institute Research, a Lawson program, in the areas of cognitive vitality and brain health, mobility and activity and mental health:
- Cognitive Clinical Trials Group (CCTG)
- Collaboration of Rehabilitation Research Evidence (CORRE)
- Gait and Brain Lab
- Geriatric Mood Disorders Lab
- MacDonald Franklin OSI Research Centre (Occupational Stress Injury)
- Mental Health Nursing Research Alliance (MHNRA)
- Mental Health INcubator for Disruptive Solutions (MINDS) of London
- Neuropsychiatry and Therapeutic Brain Stimulation Research Group
- Occupational Therapy and Spiritual Care Research Lab
- R2P (Research to Practice)
- Rehabilitation Mental Health
- Wound Care
The open house had a festive theme and many of the exhibits involved a problem solving or interactive elements to encourage learning and foster teamwork.
Karen Vecchio, federal Member of Parliament for Elgin-Middlesex-London, was among the over 200 people in attendance.

At the open house, from left: Dr. Cheryl Forchuk, MP Karen Vecchio and Roy Butler, St. Joseph's Vice President.
“London is a great community to conduct research,” explains Dr. Forchuk. “We are a mid-size city surrounded by rural areas, in many ways reflecting Canada as a whole. A lot of our projects cover the country with multiple sites and results found here by our leading experts are being implemented in health centres and national strategies in this country and around the world.”
Examining how the pandemic affects Southwestern Ontario's frontline hospital workers
LONDON, ON - A team from Lawson Health Research Institute will examine the unique personal and professional impacts of the COVID-19 pandemic on frontline hospital workers in Southwestern Ontario. The region’s frontline hospital workers are invited to participate in an online survey to share their experiences during the public health emergency. The goal is to understand impacts unique to our region in order to develop strategies that address the needs of hospital workers.
“It’s crucial to understand the impact of this pandemic on frontline hospital workers who often face difficult decisions, including risking personal safety to care for patients and the community,” explains Dr. Kimia Honarmand, Lawson Adjunct Scientist and Critical Care Physician at London Health Sciences Centre (LHSC). “Experiences are likely to vary across the province and country based on local circumstances. It’s important we hear the unique perspectives of those in our region.”
The team will recruit health care professionals from hospitals across Southwestern Ontario. Participants will be asked to complete one short survey with questions about their perceptions, causes of stress and coping strategies during the pandemic. The team hopes results can be used to identify strategies that address informational, training and support needs.
In addition to worries about personal safety, the team notes that frontline workers are faced with concerns about rapidly evolving information, patient surges and depletion of resources like ventilators and personal protective equipment (PPE). They suspect social media may play a role in compounding these fears.
“Compared with past outbreaks like SARS, today’s digital age provides a wealth of on-demand information and the majority is unverified,” says Dr. Honarmand. “While social media can be a place of solidarity and connection, it can also contribute to the spread of misinformation and fear.”
The researchers also suspect that public health measures like physical distancing, while crucial to controlling the spread of disease, may contribute to a loss of social support systems.
“Taken together, these challenges can lead to stress, anxiety and burnout,” says Carol Young-Ritchie, Executive Vice President, Chief Nursing Officer and Pandemic Incident Management Team Co-Lead at LHSC. “Hearing directly from those on the frontline can help guide hospital administrators and professional organizations in better supporting our people, both during the current pandemic and in future public health emergencies.”
Frontline hospital workers in Southwestern Ontario can learn more and access the survey at https://redcap.lawsonresearch.ca/surveys/?s=E9KKL3CXYE.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Expanded No Fixed Address strategy houses half of those in danger of homelessness
At a community symposium on health care and homelessness attended by over 250 Londoners, a research team from Lawson Health Research Institute announced the results of a nine-month, federally funded project tackling the issue of homelessness from within hospital walls.
The No Fixed Address (NFA) strategy reaches and supports patients during the crucial transitional period when they are being discharged from the hospital and re-integrated into the community. The approach was initially tested with strong success for mental health patients across the city and the second ‘version’ of the project was extended to medical units at London Health Sciences Centre’s University Hospital and Victoria Hospital.

“Many of our patients with lived experience of homelessness were saying that their journey started with a hospital discharge,” explains Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and NFA project lead. “They were often experiencing major transitions in their lives and then experienced a hospital stay. Normally a relatively short visit, they aren’t able to gather the information and make a plan to be able to leave the hospital with somewhere to stay.”
Through partnerships between service providers and non-profit organizations, the NFA strategy helps prevent homelessness by providing timely and accessible supports to patients who would otherwise be discharged into homelessness. Staff from the Canadian Mental Health Association Middlesex, Salvation Army’s Housing Stability Bank, and Ontario Works in the City of London provided direct, on-site patient access to housing and income support databases
“Lawson’s No Fixed Address research project is the first evaluation anywhere of a strategy that aims to reduce the number of hospital patients being discharged into homelessness,” says Dr. Forchuk.
Over nine months, 74 people experiencing medical health issues accessed the NFA program. Of those, 54 per cent were also experiencing mental health challenges.
All of the study participants were in imminent danger of homelessness. Through the supports provided as part of this research study, half were able to arrange housing before being discharged.
“We were able to help a lot of people, with 50 per cent successfully securing housing,” shares Dr. Forchuk. “With the results and feedback we received, we learned a lot about how we can make the program even better.”
They found that there is a need for the supports to be extended as a transitional program in the community post-discharge, as the length of stay in the medical units tended to be short.
The project’s previous phase, involving acute and tertiary psychiatric care in the London region, prevented homelessness in 95 per cent of cases. “Going into the medical units, we found that people have highly complex needs that often involved mental health challenges.
By simply using the same approach that we did for those in psychiatric care, we helped half of the people find housing. To best serve the needs of everyone, we want to follow them after discharge.”
The team sees a solution in having a housing support worker provide transitional, wrap-around services that follow the person. They would continue to meet and work together after the hospital stay, helping to access community programs.
“This role would be embedded in both the health care system and the homeless serving system, supporting individuals who have complex physical and mental health issues as they are also navigating homeless resources.”
This project is funded by the Government of Canada's Homelessness Partnering Strategy’s (HPS) Innovative Solutions to Homelessness funding stream.
Overview and Numbers
Fast facts on homelessness and health care
- Stable housing after discharge is associated with higher quality of life, reduced substance abuse and fewer hospital admissions.
- Homeless clients are four times more likely to be readmitted to hospital within a month compared to low-income matched controls.
- Hospital care for homeless clients costs an average of $2,559 more per client.
- Finding appropriate housing or avoiding a potential eviction takes time – it is important to start as soon as possible during the discharge process.
Implementation of first phases of No Fixed Address
- Access on the unit to a housing advocate and income support staff.
- The initial intervention was accessed by 219 acute psychiatric clients, as well as 32 clients within a specialized tertiary care psychiatric hospital - only 3 became or remained homeless.
- Expanded to be an immediate wrap-around service with offices set up in the hospital mental health units.
- Staff from the Canadian Mental Health Association Middlesex (CMHA), Ontario Works (OW), and Salvation Army’s Housing Stability Bank (HSB) have on-site access to housing and income support databases.
- Clients can access service by drop-in or appointment.
- Services include assistance for finding housing, financial assistance, such as rent/utilities in arrears or first/last months’ rent for a new home, and access to high quality used furnishings, household supplies and a cleaning service.
Expanded second phase of No Fixed Address
- Program ran from July 2018 to March 2019 (9 months).
- 74 people accessed the program.
- Complex situations with both mental health and physical problems: 100% had medical issues and 54% had mental health issues.
- Lengths of stay were very short.
- People could not attend drop-in due to medical issues, so they relied on referral from staff.
- Although they were all in imminent danger of homelessness, 38 people (50%) were housed as a result of this program.
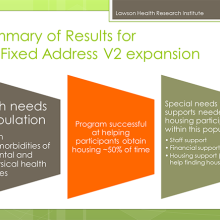
What were the main housing needs?
- Help finding a place to live
- Money for deposit
- Financial support
- Transportation support
- Help getting benefits
Recommendations and learnings for future models
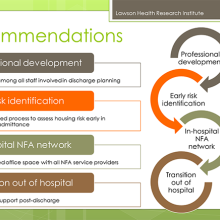
- Housing support worker needs to be a transitional support since work will be needed after discharge.
- Social work not the only key players (patient care facilitators, nursing staff, etc.).
- The transitional housing support role needs to be well embedded in the homeless serving system, as well as health care.
- People have physical and mental health issues and are also going to be navigating homeless resources.
- Despite the low success rate, many people were housed who would have otherwise been discharged to homelessness.
- We learned a lot about what was needed in an area where there was a knowledge vacuum.
- Future plans involve implementation with improvements to the model.
Expanding transitional support for young adults with diabetes
In 2012, researchers from across Ontario, led by a team at Lawson Health Research Institute, started the first multicenter randomized controlled trial to evaluate implementation of a transition coordinator for young adults with type 1 diabetes as they transferred from paediatric to adult care.
“There is a huge difference between the kind of care that they receive as children compared to adults, and that is consistent across Canada and most other countries,” explains Dr. Cheril Clarson, associate scientist at Children’s Health Research Institute, a program of Lawson, and a paediatric endocrinologist at Children’s Hospital, London Health Sciences Centre.
With children, patient visits involve a variety of specialists from different areas, such as the physician, nurse educator, dietitian and social worker. “The naturally build up a long-term relationship with the team, as some children might start the program when they are 2 or 3 years old as an example.” Dr. Clarson adds that the child’s caregivers are an integral part of the process and the care team also gets to know them very well.
Moving into the adult program means that the patient now has more responsibility and autonomy over their own care. They have to remember to go to appointments, fill prescriptions and maintain their daily diabetes care.
“During the emerging adulthood period, your attention is taken up by many other things – leaving home, starting post-secondary education, figuring out your identity and independence,” says Dr. Tamara Spaic, Lawson associate scientist and adult endocrinologist at St. Joseph’s Health Care London. “And on top of that they need to manage their diabetes every day. They are in a completely new system with a new care team – it’s a major transition. For many, they stop coming to appointments regularly and they don’t keep up with all of their own care.”
As young adults struggle to find their footing in a new system, there are significant short and long-term consequences when it comes to their health. Some will experience acute complications like high sugars leading to diabetic ketoacidosis and hospital admission or severe low blood sugars where they can lose consciousness and have a seizure.
“Different studies show between 30 to 60 per cent increased risk of complications like retinopathy, myocardial infraction, stroke and kidney disease in those who do not follow their care plan,” notes Dr. Spaic. “We see a bump in this young adult period where levels spike and their diabetes isn’t being controlled – this has impacts for both the individual and the system.”
The study enrolled 205 young adults with type 1 diabetes between the ages of 17 and 20. Patients were recruited from three paediatric centres and their care was transitioned to three adult centres. The multi-centre partnership included Children’s Hospital; St. Joseph’s; Children’s Hospital of Eastern Ontario; The Ottawa Hospital; and, Trillium Health Partners in Mississauga.
Participants were randomly assigned to two groups, with 104 patients in the structured transition program and 101 patients receiving standard care. Patients were seen in the paediatric care setting for six months and then transferred to adult care, where they continued with either the transition program or standard care for one year.
The core component of the program was a transition coordinator, a nurse who is a certified diabetes educator. The coordinator followed the young adults throughout the transition, interacting with the paediatric health care team to establish a base of support as they moved into adult care. They attended visits, established appropriate contacts for the patient, provided support for diabetic care, problem solved and helped navigate the system. In addition to face-to-face meetings, they were available via text messages, emails and phones calls.
“We had a high recruitment rate for the population and type of study, and a high number of participants followed the full program,” says Dr. Clarson. “Our results at the end of the intervention showed that the program worked very well. By providing additional support through a transitional coordinator, the results showed better outcomes all around.”
Compared to the baseline, study participants attended more care visits, were more satisfied with their care, suffered much less distress associated with diabetes, had better management on a daily basis and reported less emotional burden of diabetes.
The team then took it a step further and spent another year following the participants to see if they were able to sustain the behaviour and positive outcomes. They did not find a difference between the control and intervention groups.
“Unfortunately, we found no difference in the number of visits they attended, their satisfaction with care and management of their diabetes,” explains Dr. Spaic. “When they didn’t have the intervention, they essentially went back to baseline. Out hope is to see the program extended.”
Dr. Clarson adds that they developed the program so that it can be integrated in different ways, and also in difference areas of health care beyond diabetes. For example, they found that the preferred method of communication with the coordinator was text. This is an easy way to provide the fundamental support of a coordinator for longer, and it is cost-effective.
“Our patients really loved the intervention. By the end of the study, they felt more comfortable being able to navigate the adult health care system. They felt empowered and responded well. They wanted to continue the program.” The next step for the researchers is to evaluate support through a virtual transition coordinator.
“Closing the Gap: Results of the Multicenter Canadian Randomized Controlled Trial of Structured Transition in Young Adults With Type 1 Diabetes” was recently published in the journal Diabetes Care by the American Diabetes Association.
Learn more about the study and read about Nicole Pelcz, study participant, who found out at 13 years old that she had type 1 diabetes.
In the media:
Diabetic teens fall back to old habits after transition care, study says – London Free Press