Search
Search
Partners
Lawson is the research institute of London Health Sciences Centre and St. Joseph's Health Care London. Our scientists work across the city at multiple hospital sites, and we are proud to be an integral part of both academic hospitals and the excellent, patient-centred care they provide. In addition to the hospitals, we work in close partnership Western University and a variety of other collaborators in London, Ontario, across Canada, and around the world.
Lawson works with over 200 business and industry partners in more than 25 countries.
Partnership with Siemens Healthineers will create a centre of excellence in advanced diagnostic imaging and therapeutics
Continuing to build on the established excellence in medical imaging, London’s academic teaching hospitals, London Health Sciences Centre (LHSC), and St. Joseph’s Health Care London, and Western University’s Schulich School of Medicine & Dentistry announced a partnership with Siemens Healthineers in magnetic resonance imaging (MRI), interventional angiography, cardiology and cardiac surgery that will create a centre of excellence in advanced diagnostic imaging and therapeutics in southwestern Ontario.
This new partnership includes the creation of an education, training and scientific research support fund in the area of advanced diagnostic imaging and therapeutics. Siemens will provide in excess of $1 million in support funding for research, advanced clinical applications, teaching and outcomes analysis.
“This partnership represents another important building block in the incredible foundation of imaging excellence that we have in London,” says Dr. Narinder Paul, Chair/Chief of the Department of Medical Imaging at LHSC, St. Joseph’s, and Schulich Medicine & Dentistry.
“Not only will we become leaders in state-of-the-art imaging and intervention through the centre of excellence, but thanks to the research contribution from Siemens Healthineers, we will also have dedicated funds for critical research in cardiovascular and neurological diseases that will translate to improved services and outcomes for patients in London and the region.”
The research fund will support collaborations between research teams in diagnostic and interventional radiology, cardiology, and cardiac surgery, with imaging scientists at Lawson Health Research Institute, the research institute of LHSC and St. Joseph’s, and Schulich Medicine & Dentistry’s Robarts Research Institute, as well as research teams from across Western. These teams will partner with scientists from Siemens Healthineers to focus on improving both the patient experience and the outcomes in important cardiovascular and neurological diseases. The research funds will be leveraged against provincial and federal research grants to increase the funds available to the research teams.
“Collectively, Western and our partner institutions in London are becoming a global powerhouse, recognized for our expertise and facilities in imaging that drives discovery and innovation across a broad range of disciplines,” says Alan Shepard, President & Vice-Chancellor of Western University. “This partnership with Siemens Healthineers builds on our strengths, increases capacity to enhance patient care, and expands opportunities to integrate education, training and research for the benefit of learners and faculty. It’s a huge win for London and southwestern Ontario.”
“Imaging scientists and clinicians, working on campus and within hospital walls, have positioned London as a leader in non-invasive biomedical imaging, conducting groundbreaking research that impacts health care here and around the world,” adds Dr. David Hill, Lawson Scientific Director and Integrated Vice President, Research for London’s hospitals.
“With strong industry partnerships and working seamlessly with our hospitals and academic partners, we can build on this success. The advancements made here can be quickly translated into care within the very units where the testing is being done, which ultimately improves care for the patients and families that we serve.”
The centre of excellence will provide hands-on training in MRI, diagnostic, and interventional catheter procedures through development of advanced simulation and phantom models. Medical learners and radiologists, cardiologists, cardiac surgeons, neurologists, neurosurgeons, and technologists in London and from across Canada will be able to access this centre to improve their diagnostic and therapeutic skills, which will in-turn improve patient access to skilled clinicians.
As well, LHSC and St. Joseph’s are acquiring six clinical MRIs and six angiogram suites to be used for patient care, which will include the introduction of the first 3T MRI in the region. University Hospital will acquire a 3T/1.5T pair of MRIs, and two biplane angiogram suites. Victoria Hospital will acquire a 3T/1.5T pair of MRIs, a biplane and two single plane angiogram suites. St. Joseph’s will acquire a 3T/1.5T pair of MRIs, and a single plane angiogram suite.
“Investments in capital equipment, such as these new MRI machines and angiogram suites, are incredibly important as they will immediately translate into safer, higher quality care for the patients we serve – in this case it’s by offering the highest resolution images available, in less time, and with improved comfort for patients,” says Dr. Paul Woods, President and CEO, London Health Sciences Centre.
“London has an illustrious history of innovation that has been groundbreaking in shaping the scope and possibilities of medical imaging within the health-care system,” says Dr. Gillian Kernaghan, President and CEO, St. Joseph’s Health Care London. “This exciting partnership ensures our ongoing leadership and expertise in the introduction of leading-edge medical imaging technologies and is a critical step toward new approaches in imaging research and patient care.”
MRI is used to provide critical diagnostic information about the physical structure and the biological processes of the body. MRI scanners differ from other imaging technologies as they use strong magnetic fields, magnetic field gradients, and radio waves, instead of X-rays, to generate images of the organs in the body. MRI is widely used in hospitals to facilitate medical diagnosis and/or the staging of disease without exposing patients to radiation.
Perceptions of confidentiality for Canadian Veterans discussing moral injuries
A new study from Lawson Health Research Institute will be the first to explore Canadian Veterans’ beliefs about confidentiality in mental health care and whether those beliefs act as a barrier to seeking treatment for a type of trauma known as moral injury.
Moral injury describes psychological distress following events where a person performs, witnesses or fails to prevent acts that conflict with deeply held moral standards. Evidence suggests that moral injuries are on the rise among deployed members of the Canadian Armed Forces (CAF), and that those exposed to such events are at a higher risk of developing post-traumatic stress disorder (PTSD) and depression.
Through the study, researchers aim to understand barriers that might prevent military personnel from disclosing details of moral injury.
“A commonly reported barrier when seeking mental health treatment is a perceived lack of confidentiality,” explains Dr. Anthony Nazarov, Post-Doctoral Associate at Lawson. “Since some events that induce moral injuries are ethically ambiguous, it’s possible that military personnel may withhold details of their trauma or even avoid seeking help due to worries about confidentiality.”
The two-year study will engage 200 Canadian Armed Forces Veterans to investigate their perceptions around the confidentiality of disclosing moral injuries in the mental health care and research settings. This will be accomplished not only by interviewing Veterans receiving care at St. Joseph’s Health Care London’s Operational Stress Injury Clinic, but also through online surveys made available to military personnel and Veterans across Canada. The research team will also interview mental health professionals to understand their perspectives on this topic.
“Many Veterans seek help for mental health, and that’s great to see. We’ve come a long way in reducing stigma and barriers, but there’s more work to be done,” says Dr. Don Richardson, Lawson Associate Scientist, Director of the MacDonald/Franklin OSI Research Centre and Physician Lead at St. Joseph’s OSI Clinic. “It’s our duty as mental health researchers and clinicians to ensure that everyone who needs help seeks it. If Veterans do not feel comfortable disclosing certain details because of perceived mistrust related to privacy, we need to know why that is and what we can do to address this issue.“
“Through appropriate messages, it may be possible to dispel any false beliefs, increase trust in mental health professionals and, in turn, increase the number of veterans who choose to seek help,” notes Dr. Nazarov.
The study is being funded by Veterans Affairs Canada and St. Joseph’s Health Care Foundation’s Robert S. & Mary Gay, Donald, James, and Helen (Taylor) Gay Endowed Research Fellowship in Veterans Care.
Above: Drs. Don Richardson and Anthony Nazarov
Perceptions of confidentiality for Canadian Veterans discussing moral injuries
LONDON, ON – A new study from Lawson Health Research Institute will be the first to explore Canadian Veterans’ beliefs about confidentiality in mental health care and whether those beliefs act as a barrier to seeking treatment for a type of trauma known as moral injury.
Moral injury describes psychological distress following events where a person performs, witnesses or fails to prevent acts that conflict with deeply held moral standards. Evidence suggests that moral injuries are on the rise among deployed members of the Canadian Armed Forces (CAF), and that those exposed to such events are at a higher risk of developing post-traumatic stress disorder (PTSD) and depression.
Through the study, researchers aim to understand barriers that might prevent military personnel from disclosing details of moral injury.
“A commonly reported barrier when seeking mental health treatment is a perceived lack of confidentiality,” explains Dr. Anthony Nazarov, Post-Doctoral Associate at Lawson. “Since some events that induce moral injuries are ethically ambiguous, it’s possible that military personnel may withhold details of their trauma or even avoid seeking help due to worries about confidentiality.”
The two-year study will engage Canadian Armed Forces Veterans to investigate their perceptions around the confidentiality of disclosing moral injuries in the mental health care and research settings. This will be accomplished not only by interviewing Veterans receiving care at St. Joseph’s Health Care London’s Operational Stress Injury Clinic, but also through online surveys made available to military personnel and Veterans across Canada. The research team will also interview mental health professionals to understand their perspectives on this topic.
“Many Veterans seek help for mental health, and that’s great to see. We’ve come a long way in reducing stigma and barriers, but there’s more work to be done,” says Dr. Don Richardson, Lawson Associate Scientist, Director of the MacDonald/Franklin OSI Research Centre and Physician Lead at St. Joseph’s OSI Clinic. “It’s our duty as mental health researchers and clinicians to ensure that everyone who needs help seeks it. If Veterans do not feel comfortable disclosing certain details because of perceived mistrust related to privacy, we need to know why that is and what we can do to address this issue.“
“Through appropriate messages, it may be possible to dispel any false beliefs, increase trust in mental health professionals and, in turn, increase the number of veterans who choose to seek help,” notes Dr. Nazarov.
The study is being funded by Veterans Affairs Canada and St. Joseph’s Health Care Foundation’s Robert S. & Mary Gay, Donald, James, and Helen (Taylor) Gay Endowed Research Fellowship in Veterans Care.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Poop in a pill helping advance cancer care
Lawson Research Institute scientists have perfected the delivery of fecal transplants via patient-friendly capsules now central in ground-breaking cancer treatment studies.
It’s one of the most exciting areas of research in cancer care.
Making waves in scientific and health care circles worldwide, it holds the potent potential to “jazz up” cells that attack cancer and boost the body’s response to treatment.
So what is this powerful ally? It’s poop in a pill – home-grown right here at St. Joseph’s Health Care London and Lawson Research Institute.
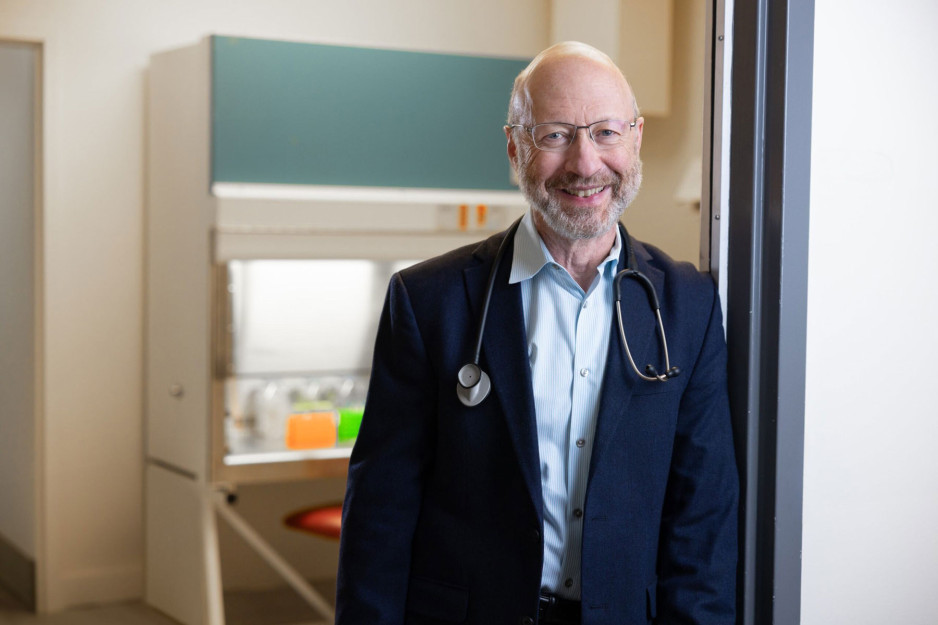
In fact, Lawson scientists Dr. Michael Silverman, Seema Nair Parvathy, PhD and their team are considered poop pill pioneers, having perfected the delivery of fecal transplantation by way of patient-friendly capsules that can be easily swallowed. These capsules contain healthy gut microbes that have become pivotal in many landmark cancer treatment studies.
Triggering an immune response
Understanding the role of poop in cancer treatment requires grasping the wonders of the human microbiome and its key role in influencing health and well-being.
The human microbiome consists of trillions of microorganisms that live inside and outside of the body, including bacteria, viruses and yeasts. While some bacteria are associated with disease, others are vital to the human immune system – the body’s main protective and disease-fighting tool – and many other aspects of health. Over the past decade, microbiome research has led to a revolution in medicine as scientists unravel just how an imbalance of these microorganisms interferes with many aspects of good health.
"(Fecal microbial transplants) allows us to harness the immune system to mount a stronger defence." Dr. Michael Silverman
The goal of fecal microbiota transplants (FMT) is to transfer healthy gut microbes from donors into patients with cancer and other diseases so that healthy bacteria will colonize in the patient’s gut and improve the microbiome, explains Silverman, Medical Director of St. Joseph’s Infectious Diseases Care Program and citywide Chief of Infectious Diseases for London’s hospitals.
To do so, stools are collected from carefully screened healthy donors, prepared in a lab into capsule format, and introduced into a patient’s gastrointestinal tract.
“What is so exciting when it comes to cancer treatment is the evidence we now have showing how a healthy microbiome activates the immune response to tumours to make the treatment more effective,” Silverman adds. “It allows us to harness the immune system to mount a stronger defense.”
St. Joseph’s capsules are central to several significant studies currently underway aimed at improving treatment for lung, kidney, breast, renal, pancreatic and other cancers.
Among the most notable is the London team’s lead role in a ground-breaking national study – one of the world’s largest randomized controlled clinical trials using FMT to improve the effectiveness of the standard of care for advanced melanoma, a type of skin cancer.
Improving melanoma survival rates
About 11,300 Canadians will be diagnosed with melanoma in 2024 and, even with standard treatment, about half that number will experience disease progression and die.
The 16-site Canadian trial builds off the work of Silverman, Parvathy and their team, in partnership with Saman Maleki, PhD, and Dr. John Lenehan at London Health Sciences Centre. Together, they were the first to demonstrate the safety and therapeutic potential of using the capsules produced at St Joseph’s to influence a patient’s gut microbiota to enhance immunotherapy and increase the odds of surviving advanced melanoma.
“London is seen as having the most expertise in use of FMT in cancer care in the world and is a driving force in moving this forward,” says Silverman. “Immunotherapy is rapidly expanding the number of treatable cancers and our FMT therapy is helping to accelerate this progress.”
Preventing infertility in men who undergo lymph node removal surgery for testicular cancer
When patients with testicular cancer undergo lymph node removal surgery there is a risk that their fertility will be affected if proper nerve sparing techniques are not used. Up to 75 per cent of men will not be able to father children if they receive the surgery without these techniques.
Lawson’s Internal Research Fund (IRF) has awarded a grant to Dr. Nicholas Power, a researcher at Lawson and urologic oncologist at London Health Sciences Centre (LHSC), who is leading a study to identify the nerves involved in fertility that are affected in lymph node removal surgery for testicular cancer.
“Sometimes patients go through a lot to be cured of testicular cancer only to be left dealing with long-term survivorship issues such as fertility. We hope to gain new insights into how fertility can be preserved after these men receive lymph node removal surgery,” says Dr. Power, who is also an assistant professor at Western University’s Schulich School of Medicine & Dentistry.
In collaboration with Schulich assistant professors Dr. Marjorie Johnson and Dr. Brian Allman, and PhD candidate Tyler Beveridge, Dr. Power published initial results in The Journal of Urology announcing their discovery of a brand new anatomic structure, the pre-hypogastric ganglion, which needs to be spared in surgery to maintain fertility. They were also able to describe the first roadmap of retroperitoneal neuroanatomy – the anatomy of nerves in the space where surgeons locate lymph nodes most commonly affected by testicular cancer that has spread.
“There has never been a definitive anatomic study of the nerves of the retroperitoneum so it was our goal to provide the first comprehensive study of the nerves as they relate directly to patients who have testicular cancer,” explains Dr. Power. “After we published the initial results we were approached by textbook authors to use our data in upcoming editions of anatomy and surgical atlases. This will help to provide insight into nerve sparing techniques for surgeons who have not been trained at high-volume centers and ultimately improve the quality of care in testicular cancer patients overall.”
Already Dr. Power has found that using this knowledge when he performs lymph node removal surgery for testicular cancer has led to a 95 per cent success rate of preserving fertility.
The IRF will go towards their research to further investigate the actual function and physiology of the retroperitoneal neuroanatomy using a pig model.
“Lawson’s IRF provides incredible support for a field of study such as ours that is not yet at the stage of applying for a large grant. Receiving the funding gives us the independence to test out novel yet important hypotheses that will then lead us to further grants,” says Dr. Power.

Above: Dr. Nicholas Power
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph's Health Care Foundation).
Probiotics could improve survival rates in honey bees exposed to pesticide
In a new study from Lawson Health Research Institute (Lawson) and Western University, researchers have shown that probiotics can potentially protect honey bees from the toxic effects of pesticides.
Honey bees are critical to agriculture as they pollinate approximately 35 per cent of the global food crop, contributing an estimated $4.39 billion per year to the Canadian economy. Pesticides are currently used to maximize crop yields, but the most common pesticides, neonicotinoid insecticides, are a major factor in colony collapse disorder which is killing honey bee populations.
“The demise of honey bees would be disastrous for humankind. A current dilemma in agriculture is how to prevent bee decline while mitigating crop losses,” says Dr. Gregor Reid, Director for the Canadian Centre for Human Microbiome and Probiotic Research at Lawson, and Professor at Western’s Schulich School of Medicine & Dentistry. “We wanted to see whether probiotics could counter the toxic effects of pesticides and improve honey bee survival.”
The study was performed by trainees Brendan Daisley and Mark Trinder in Dr. Reid’s lab at St. Joseph’s Hospital in London, Ontario. The researchers utilized fruit flies as a well-known model for studying pesticide toxicity in honey bees. Both insects are affected similarly by neonicotinoids, have very similar immune systems, and share many common microbes present in their microbiota – the collection of microorganisms found in each insect.
The researchers found that fruit flies exposed to one of the world’s most commonly used pesticides, imidacloprid (IMI), experienced changes to their microbiota and were more susceptible to infections. The flies were exposed to a comparable amount of pesticide as honey bees in the field.
By administering a specific strain of probiotic lactobacilli, survival among fruit flies exposed to the pesticide improved significantly. The mechanism involved stimulating the immune system through a pathway that insects use to adapt to infection, heat and other stresses.
“Our study showed that probiotic lactobacilli can improve immunity and potentially help honey bees to live longer after exposure to pesticides,” says Daisley, an MSc candidate. He notes that probiotic lactobacilli could be easily administered through pollen patties, which are used by beekeepers to provide nutritional support and anti-pesticide effects to honey bees.

Above: Brendan Daisley, an MSc candidate at Western's Schulich School of Medicine & Dentistry, working in Dr. Gregor Reid's lab at St. Joseph's Hospital
Over the winter months, honey bee mortality has been steadily increasing with ranges of 38 to 58 per cent in recent years, two to three times higher than the sustainable level. In Ontario alone, 340 bee keepers reported an abnormally high number of bee deaths, with over 70 per cent of dead bees testing positive for neonicotinoid residues (Government of Ontario).
“While cessation of pesticide use would be ideal, farmers currently have little alternative to obtain the yields that keep their businesses viable,” says Dr. Reid. “Until we can cease using pesticides, we need to find ways to protect humans and wildlife against their side effects. Probiotics may prove as an effective protective intervention against colony collapse disorder.”
The researchers hope to further study the mechanisms involved in this process and perform field tests on honey bee populations in Ontario.
The study, “Neonicotinoid-induced pathogen susceptibility is mitigated by Lactobacillus plantarum immune stimulation in a Drosophila melanogaster model”, is published in Nature’s Scientific Reports. The research was funded by the Natural Sciences and Engineering Research Council of Canada (NSERC).

Above: Dr. Gregor Reid, Director for the Canadian Centre for Human Microbiome and Probiotic Research at Lawson, and Professor at Western’s Schulich School of Medicine & Dentistry