Search
Search
Heather MacKenzie
Heather MacKenzie, MD; MSc
Assistant Professor, Schulich School of Medicine and Dentistry
Acquired and Traumatic Brain Injury
Dr. Heather MacKenzie is a physiatrist at Parkwood Institute and an Assistant Professor in the Department of Physical Medicine and Rehabilitation in the Schulich School of Medicine and Dentistry at Western University. She completed her residency training in Physical Medicine and Rehabilitation at Western University and subsequently earned a Master’s of Science degree in Epidemiology at the Harvard T. H. Chan School of Public Health.
Her research program focuses on predicting outcomes after concussion/mild traumatic brain injury (mTBI). Although concussions/mTBIs are common and the majority of symptoms resolve within three months, a significant proportion of individuals remain symptomatic beyond one year. These persistent symptoms result in mobility challenges and reduced participation in instrumental activities of daily living as well as vocational and leisure activities. Dr. MacKenzie’s current research focuses on identifying patients that are at high-risk for developing persistent symptoms from concussion/mTBI so that interventions can be prioritized and rehabilitation services can be quickly mobilized. Early intervention for those expected to have a prolonged recovery has the potential to alter their trajectory and optimize their potential for a positive outcome and may also reduce the occurrence of persistent symptoms and decrease secondary disability related to their injury.

Helping patients get high quality cancer care
Dr. David Palma, Radiation Oncologist at London Health Sciences Centre (LHSC) and Scientist at Lawson Health Research Institute, is a strong advocate for cancer patients getting the high-quality care they deserve.
His new book, Taking Charge of Cancer: What You Need to Know to Get the Best Treatment, is the first “how-to” manual that shows patients how to obtain and understand their medical records, double-check their doctors’ recommendations and ensure they are getting top-notch radiation, surgery or chemotherapy.
All royalties are being donated to London Health Sciences Foundation's Cancer Care Campaign, which will help to support cancer research at Lawson.
History
Each hospital’s research mission has a rich history. At both hospital organizations, leaders recognized opportunities to leverage in-house experts to conduct research and improve care. However, they also recognized the challenge in supporting these activities without dedicated space and resources.
Through great foresight, our hospitals founded the official research institutes that serve as Lawson's foundation:
- 1983: Supported by Sister Mary Doyle, former Executive Director of St. Joseph's, the Sisters of St. Joseph's establish the hospital's official research institute. LHSC and Upjohn jointly open the Victoria Upjohn Clinical Research Unit at South Street Hospital (formerly Victoria Hospital), focusing on Phase I-III clinical trials.
- 1987: The St. Joseph's research institute is named the Lawson Research Institute (LRI) in honour of London businessman and philanthropist Colonel Tom Lawson and his wife, Miggsie Lawson - close friends of Sister Mary Doyle and major supporters of the research mission.
- 1990: Victoria Hospital takes over the operation of the clinical research unit at South Street, renaming it the Victoria Clinical Trials Centre.
- 1997: The Victoria Clinical Trials Centre is renamed London Health Sciences Centre Research Inc. and becomes a fully incorporated research institute overseeing all hospital-based research within London Health Sciences Centre sites: Victoria Hospital, University Hospital and South Street Hospital.
- 2000: LRI and LHSCRI merge to form a joint venture: Lawson Health Research Institute.
- 2014: Lawson Research Institute (re-)launches as the hospital-based research arm of St. Joseph's with the goal of transforming imagination to innovation to impact; and as LHSCRI is also embedded into LHSC.
Today, partnerships remain strong, allowing researchers to move seamlessly between hospital locations and Western University.
Milestones
Since forming in 2000, Lawson has pioneered breakthroughs across various disciplines of health research and reached several institutional milestones.
- 2019: Lawson led research team is the first in the world to develop a new imaging tool, showed that MRI can be used to measure how the heart uses oxygen.
- 2019: New studies from Lawson and Western University found for the first time that HIV can be transmitted through the sharing of equipment used to prepare drugs before injection and that a simple intervention can destroy the HIV virus, preventing that transmission.
- 2019: In the first genomic analysis of head and neck cancer by smoking status, researchers at Lawson, in collaboration with researchers at the Ontario Institute for Cancer Research and UCLA Cancer Centre, carried out a comprehensive genetic analysis of HPV-negative tumours to better understand the link between smoking and cancer recovery.
- 2019: Lawson scientists develop molecular diagnostic tool to analyze epigenetic patterns, facilitating diagnosis of rare, unknown hereditary disorders. London Health Sciences Centre is the first site in the world to offer this type of testing.
- 2018: Research shows high-dose radiation can improve survival in patients with cancer that has spread to give or less sites. The SABR-COMET study was the first randomized phase II clinical trial of its kind.
- 2018: An international collaborative study between Lawson Health Research Institute, Memorial Sloan Kettering Cancer Center, the Royal Marsden and Epic Sciences is one of the first to demonstrate that a blood test can predict how patients with advanced prostate cancer will respond to specific treatments, leading to improved survival.
- 2018: In collaborative study between Lawson and Stanford University, scientists develop and test a new synthetic surfactant that could lead to improved treatments for lung disease and injury.
- 2018: Scientists use brain MRI to develop first ever method examining young people before they become ill to reliably identify who will develop acute psychosis and who will not.
- 2018: Research team develops clinically-validated, open-source 3D printed stethoscope for areas with limited access to medical supplies.
- 2018: Lawson opens Clinical Research and Chronic Disease Centre (CRCDC) at St. Joseph’s Hospital to tackle chronic disease and improve patient care.
- 2018: Lawson researchers receive $4.4 million to study personalized medicine at LHSC, examining the value of prescribing treatments based on a patient’s genetics.
- 2017: In one of the largest microbiota studies conducted in humans, researchers at Western University, Lawson Health Research Institute and Tianyi Health Science Institute in Zhenjiang, Jiangsu, China have shown a potential link between healthy aging and a healthy gut.
- 2017: Lawson researchers develop transition program to help young adults with type 1 diabetes move from paediatric to adult care.
- 2017: Innovative study brings next-generation genome sequencing to London cancer patients, contributing to province-wide database of genomic and clinical data.
- 2017: Technology developed at Western University and Lawson Health Research Institute can provide a new window into whether or not patients are responding to treatment for advanced ovarian cancer.
- 2017: Dr. Alan Getgood and his team at Western University and Lawson Health Research Institute are the first in Canada to participate in an investigative trial to determine the safety and efficacy of using a patient’s own cartilage cells to repair knee cartilage injuries.
- 2016: Lawson Researchers at Parkwood Institute are the first in Canada to develop clinical practice guidelines for managing neuropathic pain with patients who have experienced a spinal cord injury.
- 2016: Researchers at Lawson are the first in Canada to use a Prostate Specific Membrane Antigen (PSMA) probe in Positron Emissions Tomography (PET) scans to provide improved and highly specific images used for better diagnosis and management of prostate cancer.
- 2015: Lawson scientists, in collaboration with Ceresensa Inc., produce novel PET-transparent MRI head coil, a world first in imaging technology
- 2015: Lawson announces partnership with STEMCELL Technologies for commercialization of tools for Parkinson’s disease research
- 2015: Novare Pharmaceuticals and Lawson announce issuance of a U.S. patent for the composition-of-matter and use of RHAMM-binding peptides with a wide range of potential therapeutic uses. The patent also has claims for the diagnosis and prognosis of cancer, and for prescribing a course of treatment for the diagnosed cancer.
- 2014: Lawson announces licensing agreement with Yabao Pharmaceutical Group in China to develop and test a new life-saving drug to treat sepsis
- 2014: Lawson researchers are part of a Canadian team who have developed a way to produce a key medical isotope, technetium-99m (Tc-99m), using hospital based cyclotrons
- 2013: The Institute for Clinical Evaluative Sciences (ICES) Western opens at Lawson
- 2012: Lawson installs Canada's first PET/MRI at St. Joseph's Hospital
- 2011: Lindros Legacy Research Building officially opens at University Hospital
- 2010: Lawson opens the Cyclotron and PET Radiochemistry facility at St. Joseph's Hospital
- 2009: Lawson receives a record $7 million donation to support the Canadian Research & Development Centre for Probiotics
- 2008: Lawson establishes an experimental anti-thrombolitic clinic to calculate personalized dosage of drugs based on a patient's genetics
- 2007: The first totally endoscopic closed-chest robotic coronary artery bypass surgery on a patient's beating heart is performed at University Hospital
- 2006: Lawson opens the Aging, Rehabilitation & Geriatric Care Research Centre, the first centre of its kind in Canada, at Parkwood Institute
- 2005: Lawson creates the first Ontario Cardiac Rehabilitation Registry
- 2004: Lawson scientists release a three-year study on the effects of the Walkerton water disaster
- 2003: Lawson opens the Victoria Research Laboratories at Victoria Hospital, the first collaboration of its kind in Canada bringing together research from cancer, children's health and vascular biology
- 2002: Lawson installs the first Positron Emission Tomography and Computer Tomography (PET/CT) scanner in Canada at St. Joseph's Hospital
- 2001: St. Joseph's is one of five sites in the world piloting the Diabetes Electronic Management Systems
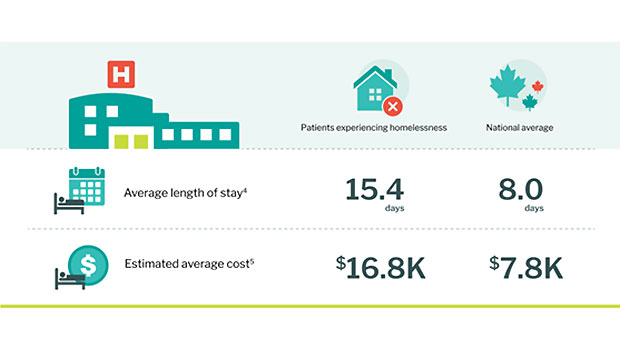
Hospital data shows longer, costlier stays for patients experiencing homelessness
Nearly 30,000 people last year were homeless when admitted to hospital and/or discharged from hospital, a first-of-its-kind Canadian analysis shows. Almost all of these inpatients were admitted following a visit to an emergency department, and the complexity of their illnesses meant they stayed twice as long as the national average.
“What’s most troubling, based on what we know from other research, is that so many were discharged into the community without stable housing,” says study co-author Dr. Cheryl Forchuk, PhD, Assistant Scientific Director at Lawson Health Research Institute. “We need to see housing as a health intervention, and an integral part of a health strategy,” says Dr. Forchuk, a trailblazer in researching health impact and solutions for people experiencing homelessness.
The new analysis – using a database from the Canadian Institute for Health Information (CIHI) – is the first detailed look at Canadian hospitals’ use of Z59.0, a mandatory record-keeping code intended to identify and improve services for patients experiencing homelessness.
Key findings from this study include:
- Nearly 30,000 patients identified as living without housing were hospitalized across Canada last year.
- Average length of stay for people experiencing homelessness was 15.4 days, compared with the national eight-day average.
- About 12 per cent of patients had hospital stays of more than one month.
- Average cost per stay was $16,800, compared with the national average of $7,800.
- Substance use, schizophrenic disorders and cellulitis (a bacterial infection) are the three most common reasons for hospital stays.
- Of these patients, 93 per cent were admitted to hospital after an emergency department visit.

Dr. Forchuk’s contribution to this work was supported through Homelessness Counts, a federally funded Lawson project launched in 2021 to improve understanding of how many people in Canada are experiencing homelessness and who they are.
Dr. Forchuk notes that the longer hospital stays, with more complex care for marginalized populations, can lead to evictions from private apartments or rooming houses.
“In London, we’re in a position to showcase what a community in partnership can do,” Dr. Forchuk notes. “We’ve done a lot of work to prevent discharge into homelessness, including the City of London and other partners prioritizing housing for people who are discharged from hospital.”
The study highlights how housing is intimately connected to health and wellbeing, and the importance of hospitals like London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London (St. Joseph’s) participating in initiatives like the Health & Homelessness Whole of Community Response in London, Ontario.
“As health care providers, we recognize the importance of accurate data for understanding an individual’s care journey across sectors and organizations, especially when addressing homelessness,” says Brad Campbell, Corporate Hospital Administrative Executive, LHSC. “For example, hospital and service utilization data has been essential to understanding emergency department patterns for those living without stable housing in our community, enabling us to improve care for marginalized people through different service delivery models. Through collaborations like our partnership with London Cares, we’ve leveraged data to help individuals in our community access supportive housing and comprehensive 24/7 health and social support services.”
Campbell notes this work aligns to priorities in the Ontario health-care sector by increasing collaboration across sectors and removing barriers to care by enabling inter-agency communication to support increased capacity and access to health-care supports.
“Housing is health care," adds Dr. Forchuk. “Gathering and analyzing this data gives us more tools to find workable solutions to the complex problem of how people experiencing homelessness receive, or don’t receive, the health care they need.
MEDIA CONTACT
Deb (Flaherty) Van Brenk, Communication Consultant
Cell: 226 577-1429 or 519 318-0657
Email: @email
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
London Health Sciences Centre has been at the forefront of medicine in Canada for 145 years and offers the broadest range of specialized clinical services in Ontario. Building on the traditions of its founding hospitals to provide compassionate care in an academic teaching setting, London Health Sciences Centre is home to Children’s Hospital, University Hospital, Victoria Hospital, the Kidney Care Centre, two family medical centres, and two research institutes – Children’s Health Research Institute and Lawson Health Research Institute. As a leader in medical discovery and health research, London Health Sciences Centre has a history of over 70 international and national firsts and attracts top clinicians and researchers from around the world. As a regional referral centre, London Health Sciences Centre cares for the most medically complex patients including critically injured adults and children in southwestern Ontario and beyond. The hospital’s nearly 15,000 staff, physicians, students and volunteers provide care for more than one million patient visits a year. For more information, visit www.lhsc.on.ca.
Renowned for compassionate care, St. Joseph’s Health Care London is a leading academic health care centre in Canada dedicated to helping people live to their fullest by minimizing the effects of injury, disease and disability through excellence in care, teaching and research. Through partnership with Lawson Health Research Institute and our collaborative engagement with other health care and academic partners, St. Joseph’s has become an international leader in the areas of: chronic disease management; medical imaging; specialized mental health care; rehabilitation and specialized geriatrics; and surgery. St. Joseph’s operates through a wide range of hospital, clinic and long-term and community-based settings, including: St. Joseph’s Hospital; Parkwood Institute; Mount Hope Centre for Long Term Care; and the Southwest Centre for Forensic Mental Health Care. www.sjhc.london.on.ca
Hospital data shows longer, costlier stays for patients experiencing homelessness
Nearly 30,000 people last year were homeless when admitted to hospital and/or discharged from hospital, a first-of-its-kind Canadian analysis shows. Almost all of these inpatients were admitted following a visit to an emergency department, and the complexity of their illnesses meant they stayed twice as long as the national average.
“What’s most troubling, based on what we know from other research, is that so many were discharged into the community without stable housing,” says study co-author Dr. Cheryl Forchuk, PhD, Assistant Scientific Director at Lawson Health Research Institute. “We need to see housing as a health intervention, and an integral part of a health strategy,” says Dr. Forchuk, a trailblazer in researching health impact and solutions for people experiencing homelessness.
The new analysis – using a database from the Canadian Institute for Health Information (CIHI) – is the first detailed look at Canadian hospitals’ use of Z59.0, a mandatory record-keeping code intended to identify and improve services for patients experiencing homelessness.
Key findings from this study include:
- Nearly 30,000 patients identified as living without housing were hospitalized across Canada last year.
- Average length of stay for people experiencing homelessness was 15.4 days, compared with the national eight-day average.
- About 12 per cent of patients had hospital stays of more than one month.
- Average cost per stay was $16,800, compared with the national average of $7,800.
- Substance use, schizophrenic disorders and cellulitis (a bacterial infection) are the three most common reasons for hospital stays.
- Of these patients, 93 per cent were admitted to hospital after an emergency department visit.
Dr. Forchuk’s contribution to this work was supported through Homelessness Counts, a federally funded Lawson project launched in 2021 to improve understanding of how many people in Canada are experiencing homelessness and who they are.
Dr. Forchuk notes that the longer hospital stays, with more complex care for marginalized populations, can lead to evictions from private apartments or rooming houses.
“In London, we’re in a position to showcase what a community in partnership can do,” Dr. Forchuk notes. “We’ve done a lot of work to prevent discharge into homelessness, including the City of London and other partners prioritizing housing for people who are discharged from hospital.”
The study highlights how housing is intimately connected to health and wellbeing, and the importance of hospitals like London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London (St. Joseph’s) participating in initiatives like the Health & Homelessness Whole of Community Response in London, Ontario.
“As health care providers, we recognize the importance of accurate data for understanding an individual’s care journey across sectors and organizations, especially when addressing homelessness,” says Brad Campbell, Corporate Hospital Administrative Executive, LHSC. “For example, hospital and service utilization data has been essential to understanding emergency department patterns for those living without stable housing in our community, enabling us to improve care for marginalized people through different service delivery models. Through collaborations like our partnership with London Cares, we’ve leveraged data to help individuals in our community access supportive housing and comprehensive 24/7 health and social support services.”
Campbell notes this work aligns to priorities in the Ontario health-care sector by increasing collaboration across sectors and removing barriers to care by enabling inter-agency communication to support increased capacity and access to health-care supports.
“Housing is health care," adds Dr. Forchuk. “Gathering and analyzing this data gives us more tools to find workable solutions to the complex problem of how people experiencing homelessness receive, or don’t receive, the health care they need.
Media Contact
Deb (Flaherty) Van Brenk, Communication Consultant
Cell: 226 577-1429 or 519 318-0657
Email: @email
Hospital-based research delivers high quality and efficient patient care
On January 10, 2020, the Honourable Jeff Yurek, Minister of Environment, Conservation and Parks and MPP for Elgin-Middlesex-London, joined London Health Sciences Centre (LHSC), Lawson Health Research Institute and the Ontario Hospital Association for a research tour at LHSC’s University Hospital.
This tour was organized to afford the Minister the ability to see first-hand how research-intensive hospitals like those in London are helping to deliver high quality and efficient patient care to people across the province and beyond.
At University Hospital, Drs. Matthew Teeter and Brent Lanting are leading clinical research in hip and knee replacement that is reducing the time patients are in hospital following surgery. They are utilizing wearable technology to better assess how patients are doing, flag issues and predict outcomes, while partnering with industry to develop the next generation of implants.
Dr. Teeter leads one of Canada’s only Implant Retrieval Labs, which stores thousands of failed hip, knee and shoulder implants retrieved from patients. Surgeons and scientists from all over the world send implant specimens to London to be imaged and studied.
As the research institute of LHSC and St. Joseph’s Health Care London, Lawson’s researchers and their teams are helping people live their life to the fullest by minimizing the effects of injury, disease and disability. Research is done within hospital walls and can be directly implemented into patient care.
This includes ground breaking work in minimally invasive and robotic cardiac surgeries let by Dr. Michael Chu and the cardiac surgery team. They have helped patients like Maria Bruno who shared her experience as a patient, and the impact on her own life and that of her family.

“Today, my heart is in perfect condition,” shares Maria. “The ability to perform this procedure is unique in Canada. I’m forever grateful to this hospital and Dr. Chu for being able to repair it. I’m a huge advocate for continued research because there are many, many patients who could benefit.”
As an active clinician researcher, Dr. Chu also investigates augmented reality image guidance in minimally invasive valve surgery, experimental transcatheter technology and complex aortic reconstruction. In 2019, Dr. Chu along with colleagues from University Health Network published a high-impact finding that women are more likely to experience poorer outcomes following aortic surgery.
Dr. Mandar Jog is a world leader in his field, revolutionizing treatment for people with movement disorders including Parkinson’s disease and essential tremor. Last year, his work on spinal cord stimulation was covered by BBC World News.
Patients Real Beaulieu and Guy Alden who have been involved with the team’s clinical trials told the Minister about the dramatic improvements in their quality of life

“With the tremor, I was at the point where I couldn’t write, I couldn’t get a key in the key hole. I couldn’t function normally in life and it was embarrassing for me,” remembers Real. “After the treatment with Dr. Jog, it was a huge turnaround for me and how I could live my life.”
Hospital-based research is critical to supporting health care in Ontario. “Health research is a necessity in order to provide the best care for patients and ensure the health system is sustainable. Researchers, clinicians, staff and trainees working at hospital sites across the city are driving important discoveries that continually improve patient care,” says Dr. David Hill, Lawson Scientific Director and Integrated VP, Research for LHSC and St. Joseph’s Health Care London.
Hospital-based research in London ranked in the top 10 for Canada
Lawson Health Research Institute is ranked eighth in the country according to the 2018 edition of “Canada’s Top 40 Research Hospitals List” by Re$earch Infosource. This strong position has been maintained by Lawson for the past five years and also keeps the institute within the top five institutions in Ontario.
The research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London (St. Joseph’s), Lawson has also maintained the top ranking for research intensity among the large tier institutions, with $616,300 of research spending per researcher.
“As a hospital-based research institute, our innovation happens where care is delivered,” says Dr. David Hill, Lawson Scientific Director. “Every day, teams of researchers are working directly with clinicians and patients to improve treatments, or create entirely new ones. They find innovative methods of delivering services that drive efficiency and reduce costs.”
The top 40 list analyzes hospital-based research institutes from across the country on several metrics, including total research income from the previous fiscal year. The ranking looks at funds received from all sources, including both internal and external, to support research at the organization. According to the report, Lawson received $123,255 million in research income in 2017, which was a 0.8 per cent drop from the previous fiscal year.
Dr. David Hill advocates for increased scientific funding nationally. “We held our position despite the modest decrease in funding. Canada as a whole requires significant investment in scientific discovery to increase the well-being of Canadians and build a robust economy.”
This year, a special spotlight on intellectual property (IP) is showcasing the top Canadian organizations – universities, corporations, hospitals and government departments/agencies – patenting at the US Patent and Trademark Office.
Lawson, as the research institute of LHSC and St. Joseph’s, is featured in the top 10 list for Hospital Patent Leaders as measured by ownership of patents granted between 2013-2017. Lawson has ranked in the sixth spot with 13 patents owned.
Commercialization opportunities are managed through WORLDiscoveries®, the business development arm of London’s extensive research network. Born out of a partnership between Lawson, Robarts Research Institute and Western University, WORLDiscoveries® draws upon a mix of industry connections, sector-specific market knowledge, and business development expertise to help researchers and local inventors commercialize their discoveries through licensing and new company spin-offs.
“We support technology development and licensing agreements by taking local knowledge and discoveries to industry partners worldwide,” explains Dr. Hill. “Research-intensive hospitals are improving health care, creating jobs and contributing to the country’s growing knowledge economy.”
Featured Innovations
A Stroke of Genius

Based at St. Joseph’s Hospital in London, Dr. Ting-Yim Lee specializes in computed tomography (CT) imaging, a type of x-ray technology that captures images of slices of the body. As a young scientist, he dreamed of using CT imaging to measure how blood flows in the human body. The idea was to develop software that could be installed on existing CT scanners to make quick, easy work of a very complex algorithm. If a patient came to the emergency room suffering from a stroke, it would allow the doctor to quickly analyze and address the damage.
Thanks to decades of public and private sector support, Dr. Lee’s idea has evolved from concept to prototype to clinically-approved product. Through a licensing deal with GE Healthcare, his software is now installed on 70 per cent of the company’s new CT scanners on the market. It’s currently in use in more than 8,000 hospital imaging departments around the world.
Stroke is a situation where every minute of delay in treatment has grave consequences on the recovery of the patient, and this software allows physicians to quickly decide on the best treatment for the patient. Dr. Lee is extending his technology to measure blood flow in whole organs, including predicting and monitoring how cancer and heart attacks respond to treatment. The royalties from the licenses enabled Lawson to install Canada’s first PET/CT scanner to complement CT Perfusion with metabolic information from PET scanning.
Novel discovery in the field of Parkinson’s Disease

In addition to a busy neurosurgery practice, Dr. Matthew Hebb maintains a highly productive research program. Dr. Hebb is creating tools to advance Parkinson’s Disease research and therapeutics across the globe. Parkinson’s Disease is characterized by progressive neurological impairment caused by the death of cells in the nervous system. Dr. Hebb’s team provided a novel description of brain-derived progenitor cells (BDPCs) that could protect and stimulate re-growth of disease-affected neurons. This discovery may offer critical insight into the disease process and provide a new personalized source of brain-derived cells for delivering therapy back into the same individual.
By using a patient’s own BDPCs, Dr. Hebb hopes to slow or halt disease progression and stimulate regeneration of damaged brain circuitry. BDPCs may further advance drug, genetic and functional screening across broad patient populations. This work also resulted in a patent and partnership with STEMCELL Technologies to develop innovative research tools for Parkinson’s Disease and other incurable neurological diseases.
Computer assisted surgical techniques and technologies

Dr. Christopher Schlachta is Medical Director of CSTAR, the Canadian Surgical Technologies & Advanced Robotics, at LHSC. His current research interests are focused on development of computer-assisted surgical techniques and technologies to enhance care and training. Along with his team, he has demonstrated how computer-assisted technologies in the operating room can enhance communication among surgeons and trainees to produce better outcomes for patients. He is currently partnering with industry to commercialize operating room technology developed with engineers at CSTAR.
His Wireless Hands-free Surgical Pointer system incorporates infrared and inertial tracking technologies to address the need for hands-free pointing during minimally invasive surgery. The combination of these technologies allows for optimal movement of the pointer and excellent accuracy while the user is located at a realistic distance from the surgical monitor.
Smart tech, smart treatment for movement disorders

Dr. Mandar Jog operates the London Movement Disorders Centre and has driven the development of TremorTek, a wearable sensor technology that has already successfully treated hundreds of research patients who suffer from tremors in their arms and hands. These tremors, typically caused by Parkinson’s disease or essential tremor, are a common movement disorder symptom yet there is no effective treatment. Neurotoxin therapy has been identified as a possible treatment for tremors; however, an injection in the wrong place or at the wrong dose can cause negative side effects. Everyone experiences tremors in different ways – the location and strength of the movements, and how often they occur varies widely.
Using commercially available sensor technology, Dr. Jog and his team were able to isolate independent muscle movements. They created a system that matched the muscle activity pinpointed by the sensors with the correct amount of toxin to administer. This kinematic technology can be applied to the pre-treatment assessment of patients and the information generated can guide the placement of botulinum toxin. The technology has been taken by a spinoff company MDDT Inc. that has been working with numerous stakeholders interested in its applications.
How changes in the brain affect walking while talking in older adults
Dr. Manuel Montero-Odasso’s research demonstrates that gait testing, such as walking while performing a cognitively demanding task like counting backwards (dual-task gait),can be an effective predictor of progression to dementia. In a new study, a team at Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry has discovered changes to the brain that correspond to these findings.
These changes identify a brain mechanism that corresponds with slow dual-task gait among older adults with mild cognitive impairment (MCI), an intermediate stage between the expected cognitive decline of normal aging and the more serious decline of dementia. Through their work Dr. Montero-Odasso and his team have found that a high dual-task gait cost, or a significant slowdown in walking speed when dual-tasking, is associated with a two- to three-fold increased risk of progression to dementia. However, the brain mechanism underlying this association was unclear.
To address this research question, Dr. Montero-Odasso partnered with Robert Bartha, PhD, an imaging scientist at Schulich Medicine & Dentistry and Robarts Research Institute at Western University. The team used magnetic resonance imaging (MRI) to examine the medial temporal areas of the brain, particularly the hippocampus, the parahippocampal gyrus, and the entorhinal cortex, which are regions particularly vulnerable to degeneration in Alzheimer’s disease. Participants were 40 older adults with MCI taking part in Dr. Montero-Odasso’s “Gait and Brain Study” at St. Joseph’s Health Care London’s Parkwood Institute.
The researchers found that participants with higher dual-task gait costs had a smaller grey matter volume in the left entorhinal cortex. Although grey matter volume loss is a common finding in people with Alzheimer’s disease, it is still unclear which areas of the brain are first affected by neurodegeneration. This finding points to the entorhinal cortex as a susceptible brain region in early stages of cognitive decline. This is in line with previous studies reporting that progression to Alzheimer’s disease is associated with volume loss in the entorhinal cortex.
The study therefore suggests that cognitive and motor dysfunction in older adults with MCI share common changes to the brain. This further supports that dual-task gait changes may be a measurable motor marker for neurological degeneration happening in Alzheimer’s disease.
“These novel results show that early brain changes common to pre-dementia states can be manifested by the way patients walk,” says Dr. Montero-Odasso, scientist at Lawson, geriatrician at St. Joseph’s Health Care London, and professor at Schulich Medicine & Dentistry. “This evidence supports walking while performing a cognitively demanding task as an important way to help predict dementia.”
The study, “Entorhinal Cortex Volume Is Associated With Dual-Task Gait Cost Among Older Adults With MCI: Results From the Gait and Brain Study,” is published in The Journals of Gerontology: Series A.