Search
Search
Growing Tissues in the Lab
When challenged by surgeons to find better treatments for difficult-to-manage connective tissue diseases, Dr. David O’Gorman gladly accepted.
Dr. O’Gorman is a Molecular Biologist and Lawson Scientist based at St. Joseph’s Hospital, a part of St. Joseph’s Health Care London. His research focuses on understanding normal and abnormal connective tissue repair. He collaborates with researchers and clinicians working in many different disciplines, including those specializing in reconstructive surgery, orthopedics and urology.
Surgical reconstructions can be hampered by a lack of graft tissue, or graft tissue of insufficient quality, making it difficult to achieve optimal outcomes for the patients.
An example is a condition called urethral stricture disease (urethral scarring). This condition occurs in males and typically causes symptoms such as frequent and urgent urination, and slow urinary stream. In extreme cases, it can cause urinary tract infections, permanent bladder dysfunction and renal failure. Recurrence rates after minimally invasive treatments are high, and so many urologists recommend open surgical approaches.
Surgeons can use the patient’s own tissues to reconstruct the urethra after stricture removal. This tissue is normally sourced from the buccal cavity in the mouth but taking large tissue grafts can result in complications. In cases where buccal grafts have been used for previous reconstructions, there may not be enough intact tissue left.
Dr. O’Gorman sees a solution in growing sheets of human buccal tissues in the lab.
“We are currently using buccal graft trimmings as a source of cells, culturing them in a 3D environment and expanding them to create tissues of suitable size, density and elasticity.”
The patient’s own cells are used to generate a tissue graft for urethral reconstruction. While several research groups have developed this approach in the past, few have attempted to translate their models for clinical use.
“Our immediate goal is to provide proof of principle – that we can consistently generate grafts of suitable size and functional characteristics,” explains Dr. O’Gorman, “In the future, we could be providing bioengineered graft tissues for reconstructive surgeries here in London.”
Bioengineered human tissues can also be used as ‘mimetics’ – replications of human tissues – to study diseases, especially those difficult to model using routine laboratory methods.
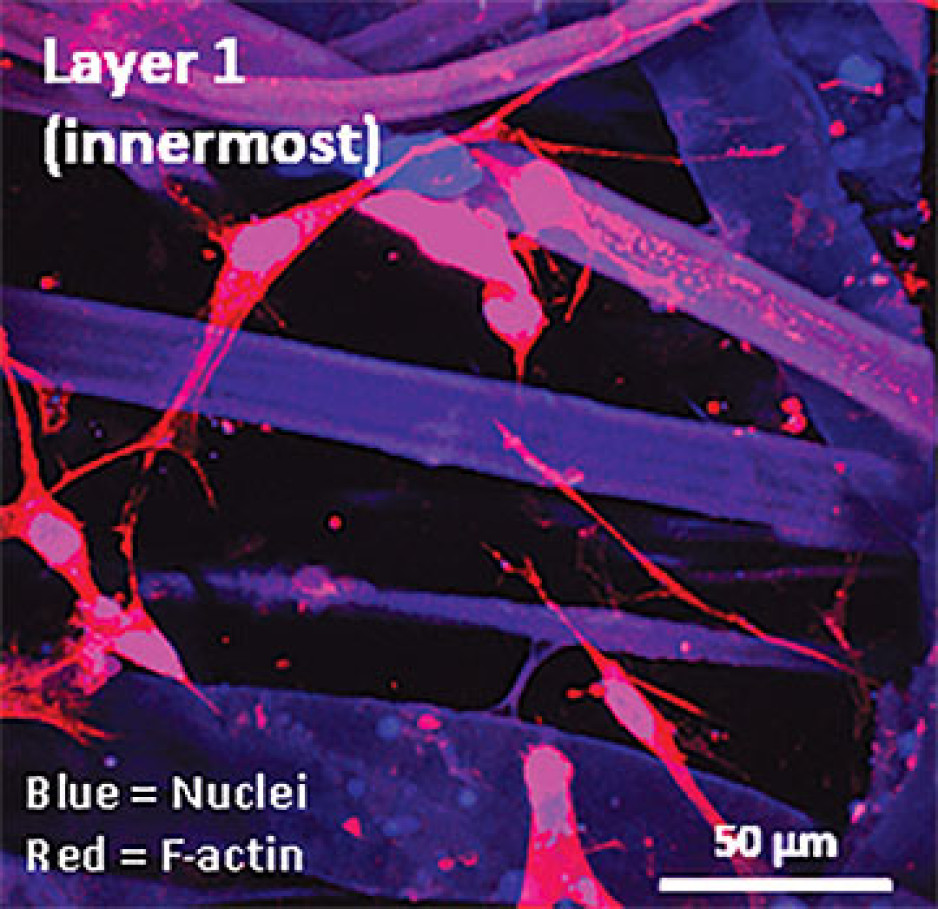
Instead of a using a growth media or sterile plastic dishes, 3D cell culture is achieved by embedding cells in a matrix of proteins and other molecules normally found in those tissues. In this environment, gene expression and growth is more similar to cells of connective tissues in the body being replicated.
Dupuytren’s disease (or Dupuytren’s Contracture) affects the palmar fascia in the hand, a connective tissue beneath the skin that extends from the base of the palm into the fingers. This disease can be understood as a type of excessive scarring, where normal tissue repair processes have gone awry and dense scar tissue forms, typically causing permanent palm or finger flexion that restricts hand function.
This condition is surprisingly common and may affect more than one million people in Canada. While there are surgical treatment options available, none consistently prevent this disease from recurring in at least a third of patients.
“Due to its high recurrence rate after treatment, Dupuytren’s disease is currently considered incurable. Our challenge is to understand it well enough to develop truly effective treatments,” says Dr. O’Gorman.
Human hands have unique characteristics not found in other species, making animal models impractical. Instead, Dr. O’Gorman’s team extracts cells from the diseased palmar fascia of patients undergoing hand surgeries and bioengineers them into palmar fascia ‘contractures’ in the lab.
“Since the cells from a single palmar fascia sample can be used to grow dozens of little contractures, we can test many different treatments simultaneously to see what works best for each patient.”
This approach may also allow them to determine if Dupuytren’s disease is truly one disease, or a group of similar diseases that cause palm and finger contractures.
“Often, Dupuytren’s disease is clearly heritable, but some individuals have no family history of it and develop apparently sporadic disease,” notes Dr. O’Gorman. “We want to determine if these are truly the same disease at the molecular level.”
Another major cause of abnormal connective tissue repair is infection, and tissue mimetics can play a role here, too. While rare, infections of artificial joint replacements are particularly devastating for patients, as they typically require readmission to hospital to remove the infected joint, weeks of antibiotic-based treatment, and an additional surgery to replace the artificial joint.
In addition to the associated pain and suffering, these procedures are technically challenging and costly to our health care system.
Artificial shoulder joint infections are most frequently caused by the microorganism Cutibacterium acnes (C. acnes). C. acnes infections disrupt normal tissue repair processes after surgery, cause shoulder tissues to die and promote loosening of the artificial joint. These infections are difficult to diagnose, and there is a lack of reproducible
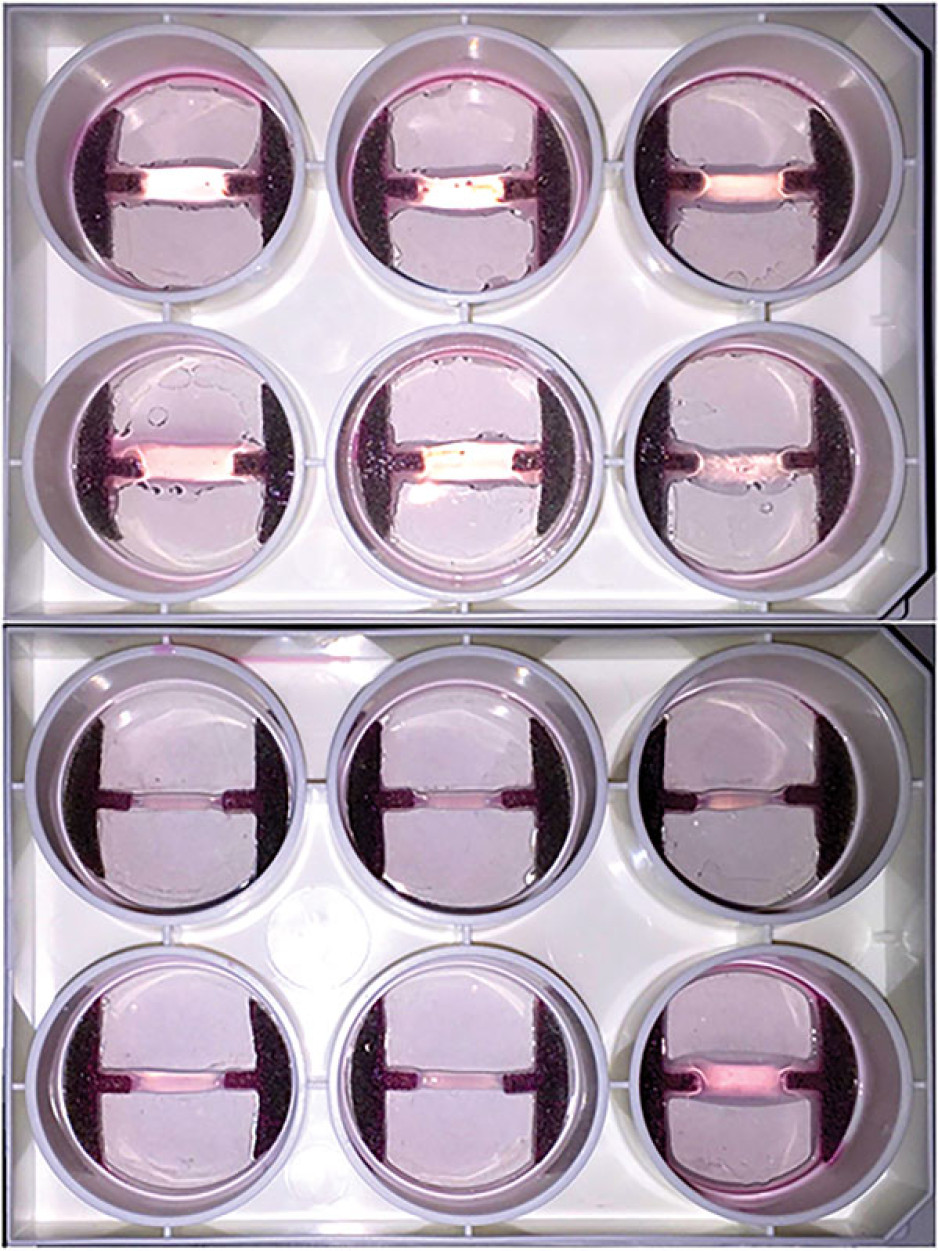
models in which to study them. Dr O’Gorman’s team has set out to create the first human Shoulder-Joint Implant Mimetic (S-JIM) of C. acnes infection.
“While S-JIMs are more complex, they are 3D in vitro cell culture systems designed to mimic human tissues, like those that we use for studying Dupuytren’s disease.”
S-JIMs include layers of artificial human tissue, wrapped around cores of titanium alloy or cobalt chrome, the metals used to create artificial joints. They are co-cultured with C. acnes under low oxygen conditions similar to those that normally occur around artificial shoulder joints.
“We are bioengineering simple 3D cell cultures to more closely mimic the complexity of human tissues, with blood supply, nerves and interactions with other cells.” – Dr. David O’Gorman
Studying the connective tissue layers close to the infection allows researchers to investigate processes that promote infection, such as the formation of a biofilm that harbours and protects the bacteria from the body’s immune system. They are also able to test whether novel treatments can disrupt biofilm formation and increase the effectiveness of antibiotics.
Dr. O’Gorman predicts that in the future, medical researchers will routinely use bioengineered 3D human tissue and organ mimetics to accelerate our understanding of disease.
“The technology is in its infancy, but the potential for using bioengineered human tissues for surgical reconstructions or as disease models is huge. At Lawson, we’re ready to take on health care challenges and build on innovative approaches to improve the quality of life for patients.”
ONLINE EXCLUSIVE: What is 3D cell culture?
Medical researchers have grown human cells in culture media on or in sterile plastic dishes, such as Petri dishes, for more than 50 years.
Some cells, such as blood cells, can survive and grow in suspension, while others like smooth muscle cells need¬ to adhere to a surface to survive and grow. These are often called “2D cell cultures” because the cells grow horizontally across the bottom of the dish.
Some cells derived from connective tissues, such as fibroblasts, are not only adherent, but also very sensitive to the stiffness of their environment (“biomechanically sensitive” cells). Plastic dishes are at least 10,000 times stiffer than most connective tissues, and when biomechanically sensitive cells detect stiff surfaces, they can change the expression of their genes and behave abnormally.
The most common proteins in these tissues - and in the entire human body - are collagens, and one routine 3D cell culture approach is to embed fibroblasts in a collagen gel (gelatin). Fibroblasts in this environment can grow in any direction they choose, and their gene expression is more similar to cells in connective tissues.
These simple 3D cell cultures represent tissue engineering in its most basic form.
“Our challenge is to bioengineer simple 3D cell cultures in the lab to more closely mimic the complexity of human tissues, which have blood supply, nerves and interactions with other cells and tissues that modify their function and ability to heal after injury,” explains Dr. O’Gorman.
Dr. David O’Gorman is a Lawson Scientist and Co-director, Cell and Molecular Biology Laboratory at The Roth | McFarlane Hand and Upper Limb Centre in London, Ontario. He is also an Assistant Professor at Western University.
Health research in London receives millions in funding from federal government
Lawson Health Research Institute was awarded over $1.2 million in the Canadian Institutes of Health Research’s Fall 2019 Project Grant competition, for three projects including one Priority Announcement.
“This is a great accomplishment for the successful researchers at Lawson and those working across the city,” says Dr. David Hill, Lawson Scientific Director. “At Lawson, our scientists target rapid response research that can be quickly incorporated into improved care for patients and families. Our research happens within hospital walls, where care is delivered, with innovations that improve lives every day.”
Western University received more than $11.9 million in research funding through the project grant competition for 17 projects. A special congratulation to Lawson researchers Drs. Samuel Asfaha, Thomas Appleton, Neil Duggal, David Spence and Zhu-Xu Zhang, as well as Dr. Subrata Chakrabarti, recipient of the CIHR Priority Announcement for “Novel mechanisms in diabetic cardiomyopathy.”
Selective Brain Hypothermia via Intranasal Cooling to Limit Brain Injury Post Cardiac Arrest
Dr. Ting-Yim Lee
There are 40,000 cardiac arrests per year in Canada. Within the body, it triggers a complex cascade of dysfunction resulting in cell death, even after successful cardiopulmonary resuscitation, with only three to seven per cent of survivors returning to normal function.
To reduce the high incidence of brain damage and the burden on families, the American Heart Association has recommended hypothermia for neuroprotection in post cardiac arrest care.
However, current clinical hyperthermia cools the whole body instead of just the brain. Simple, effective and non-invasive methods to selectively cool the brain that can be readily used in and out of hospitals are not available.

“The grant is allowing us to collect validative data on the protective effect of brain cooling in limiting brain injury from cardiac arrest,” explains Dr. Lee. “The device is very convenient to use. It is compact and can be set up right by the bedside of patients in intensive care units.”
Dr. Lee sees the device as having the potential to be used widely to limit brain injury following stroke, head trauma and sepsis.
“This kind of investment in hospital-based research allows us to identify important clinical problems and find ways to solve them, working closely with research patients along the way.”
Multi-centre diagnostic performance of dynamic CT perfusion for functional assessment of multi-vessel coronary artery disease with dense coronary calcification
Dr. Aaron So
Coronary artery disease (CAD) occurs when plaque forms in one or more coronary arteries of the heart. It is one of the leading causes of mortality and morbidity in the world.
Patients with CAD can go to a cardiac catheterization laboratory where the narrowed coronary artery can be reopened using a catheter-based technique. However, this approach is invasive for the patient and costly for the system. Studies have shown that for various reasons not all patients benefit from this treatment.

With the funding, they are testing the technique at several hospitals and national cardiovascular centres in Canada, China, Germany and Japan. With larger clinical studies in the future, they could determine the optimal diagnostic strategy for patient triage and reduce unnecessary procedures.
“Health research has been and will continue to be very important, with the commitment of patients and clinicians playing a crucial role in the success of medical research and advancement,” says Dr. So. “It’s important for the Canadian government to continue to support research in academic hospitals.”
He adds that the success of the CIHR grant application shows that Canadian researchers can be leaders in health research that benefits people around the world.
Filling Knowledge Gaps for the Success of Ontario Renal Plan 3
Dr. Matthew Weir
The Ontario Renal Network (ORN) is the agency responsible for distribution of funding for kidney care in Ontario. They have released three policy statements outlining strategic objectives for kidney care, with the most recent being the recently released Ontario Renal Plan 3 (ORP3).
“Within the strategic objective, gaps in our understanding of kidney disease have been identified as barriers to successful implementation,” explains Dr. Weir. “We have proposed a suite of 32 related retrospective cohort analyses designed using integrated knowledge translation to address those gaps.”
The Priority funding will help get the first projects underway and build momentum. “The ORP3 had extensive consultation with patients, families and other stakeholders. By supporting its successful implementation, our findings will have a direct and immediate effect on patients in areas that are a priority to them.”

Hospital-based research in London ranked in the top 10 for Canada
Lawson Health Research Institute is ranked eighth in the country according to the 2018 edition of “Canada’s Top 40 Research Hospitals List” by Re$earch Infosource. This strong position has been maintained by Lawson for the past five years and also keeps the institute within the top five institutions in Ontario.
The research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London (St. Joseph’s), Lawson has also maintained the top ranking for research intensity among the large tier institutions, with $616,300 of research spending per researcher.
“As a hospital-based research institute, our innovation happens where care is delivered,” says Dr. David Hill, Lawson Scientific Director. “Every day, teams of researchers are working directly with clinicians and patients to improve treatments, or create entirely new ones. They find innovative methods of delivering services that drive efficiency and reduce costs.”
The top 40 list analyzes hospital-based research institutes from across the country on several metrics, including total research income from the previous fiscal year. The ranking looks at funds received from all sources, including both internal and external, to support research at the organization. According to the report, Lawson received $123,255 million in research income in 2017, which was a 0.8 per cent drop from the previous fiscal year.
Dr. David Hill advocates for increased scientific funding nationally. “We held our position despite the modest decrease in funding. Canada as a whole requires significant investment in scientific discovery to increase the well-being of Canadians and build a robust economy.”
This year, a special spotlight on intellectual property (IP) is showcasing the top Canadian organizations – universities, corporations, hospitals and government departments/agencies – patenting at the US Patent and Trademark Office.
Lawson, as the research institute of LHSC and St. Joseph’s, is featured in the top 10 list for Hospital Patent Leaders as measured by ownership of patents granted between 2013-2017. Lawson has ranked in the sixth spot with 13 patents owned.
Commercialization opportunities are managed through WORLDiscoveries®, the business development arm of London’s extensive research network. Born out of a partnership between Lawson, Robarts Research Institute and Western University, WORLDiscoveries® draws upon a mix of industry connections, sector-specific market knowledge, and business development expertise to help researchers and local inventors commercialize their discoveries through licensing and new company spin-offs.
“We support technology development and licensing agreements by taking local knowledge and discoveries to industry partners worldwide,” explains Dr. Hill. “Research-intensive hospitals are improving health care, creating jobs and contributing to the country’s growing knowledge economy.”
Featured Innovations
A Stroke of Genius

Based at St. Joseph’s Hospital in London, Dr. Ting-Yim Lee specializes in computed tomography (CT) imaging, a type of x-ray technology that captures images of slices of the body. As a young scientist, he dreamed of using CT imaging to measure how blood flows in the human body. The idea was to develop software that could be installed on existing CT scanners to make quick, easy work of a very complex algorithm. If a patient came to the emergency room suffering from a stroke, it would allow the doctor to quickly analyze and address the damage.
Thanks to decades of public and private sector support, Dr. Lee’s idea has evolved from concept to prototype to clinically-approved product. Through a licensing deal with GE Healthcare, his software is now installed on 70 per cent of the company’s new CT scanners on the market. It’s currently in use in more than 8,000 hospital imaging departments around the world.
Stroke is a situation where every minute of delay in treatment has grave consequences on the recovery of the patient, and this software allows physicians to quickly decide on the best treatment for the patient. Dr. Lee is extending his technology to measure blood flow in whole organs, including predicting and monitoring how cancer and heart attacks respond to treatment. The royalties from the licenses enabled Lawson to install Canada’s first PET/CT scanner to complement CT Perfusion with metabolic information from PET scanning.
Novel discovery in the field of Parkinson’s Disease

In addition to a busy neurosurgery practice, Dr. Matthew Hebb maintains a highly productive research program. Dr. Hebb is creating tools to advance Parkinson’s Disease research and therapeutics across the globe. Parkinson’s Disease is characterized by progressive neurological impairment caused by the death of cells in the nervous system. Dr. Hebb’s team provided a novel description of brain-derived progenitor cells (BDPCs) that could protect and stimulate re-growth of disease-affected neurons. This discovery may offer critical insight into the disease process and provide a new personalized source of brain-derived cells for delivering therapy back into the same individual.
By using a patient’s own BDPCs, Dr. Hebb hopes to slow or halt disease progression and stimulate regeneration of damaged brain circuitry. BDPCs may further advance drug, genetic and functional screening across broad patient populations. This work also resulted in a patent and partnership with STEMCELL Technologies to develop innovative research tools for Parkinson’s Disease and other incurable neurological diseases.
Computer assisted surgical techniques and technologies

Dr. Christopher Schlachta is Medical Director of CSTAR, the Canadian Surgical Technologies & Advanced Robotics, at LHSC. His current research interests are focused on development of computer-assisted surgical techniques and technologies to enhance care and training. Along with his team, he has demonstrated how computer-assisted technologies in the operating room can enhance communication among surgeons and trainees to produce better outcomes for patients. He is currently partnering with industry to commercialize operating room technology developed with engineers at CSTAR.
His Wireless Hands-free Surgical Pointer system incorporates infrared and inertial tracking technologies to address the need for hands-free pointing during minimally invasive surgery. The combination of these technologies allows for optimal movement of the pointer and excellent accuracy while the user is located at a realistic distance from the surgical monitor.
Smart tech, smart treatment for movement disorders

Dr. Mandar Jog operates the London Movement Disorders Centre and has driven the development of TremorTek, a wearable sensor technology that has already successfully treated hundreds of research patients who suffer from tremors in their arms and hands. These tremors, typically caused by Parkinson’s disease or essential tremor, are a common movement disorder symptom yet there is no effective treatment. Neurotoxin therapy has been identified as a possible treatment for tremors; however, an injection in the wrong place or at the wrong dose can cause negative side effects. Everyone experiences tremors in different ways – the location and strength of the movements, and how often they occur varies widely.
Using commercially available sensor technology, Dr. Jog and his team were able to isolate independent muscle movements. They created a system that matched the muscle activity pinpointed by the sensors with the correct amount of toxin to administer. This kinematic technology can be applied to the pre-treatment assessment of patients and the information generated can guide the placement of botulinum toxin. The technology has been taken by a spinoff company MDDT Inc. that has been working with numerous stakeholders interested in its applications.
Institute Team
Administration
Research Administration: responsible for the Lawson Approval process, delivery of Lawson’s Quality Assurance and Education program for clinical research, contract negotiation and approval for research, including industry-sponsored and investigator-initiated contracts, and fee-for-service support through Lawson Clinical Research Services.
Finance: responsible for the ongoing management of all research grants and contracts awarded to Lawson researchers; works closely with researchers, administrative staff, and funding sponsors to ensure adherence to funding guidelines and policies; manages the post-award functions for all research grants and contracts at the institute, including financial reporting, financial analysis and forecasting, cash flow and expenditure monitoring, compliance oversight, audit facilitation, and communicating with funding sponsors.
Research Human Resources: responsible for providing human resource services for Lawson researchers and staff, including acting as liaison between hospital Human Resources (HR) departments and Western faculties; the health and safety component facilitates standardizing safety processes and ensuring relevant legislation and safety standards are being met.
Research Operations & Technical Services: responsible for organizing the operations of Lawson’s vivarium/animal care facilities and services, as well as coordinating laboratory space, renovations, equipment and maintenance aspects of Lawson.
Research Informatics: responsible for supporting clinical researchers who have software development and database requirements by providing robust infrastructure to support their research activities, on a safe, secure IT platform to ensure patient confidentiality for clinical activities; and providing assistance with application development, data collection, data extraction, archiving, collaboration, analysis and reporting.
Strategic Planning and Development
Communications & External Relations: responsible for building and managing the Lawson brand and reputation, including public relations, media relations, marketing, special events, web presence and social media, advocacy, strategic planning and issues management.
Grant Development: responsible for facilitating the full spectrum of research grant submissions, including grant coordination for large government grant applications; development of grantsmanship; dissemination of new information pertaining to research and training grants opportunities; and, institution submissions and sign-off processes for CIHR, CFI, ORF, etc.
Business Development: responsible for providing services to Lawson investigators to facilitate the transfer of medical research from the laboratory to commercial use, including assisting with patenting new discoveries and finding commercial partners for collaborative research and licensing. Expertise is offered in the areas of intellectual property protection, marketing, licensing agreements and formation of start-up companies. Commercialization opportunities at Lawson are managed through WORLDiscoveries®, the business development arm of London’s extensive research network and the bridge between local invention and global industry.
Research Infrastructure: responsible for the development and implementation of a research master plan for all Lawson sites, including identifying potential research space solutions to meet the evolving needs of researchers, and working with the Facilities Planning departments at both hospitals to operationalize research space plans.
International Women's Day 2020
International Women’s Day, taking place on March 8, 2020, is a day to celebrate the various achievements of women around the world and is a call to action for gender parity. This year’s theme is “Each for Equal” to emphasize that each individual has a significant part in working towards a gender equal world.
This year, Lawson is highlighting the different paths for women who are working towards a career in the health sciences. Below are the perspectives from students, physicians and researchers on their contributions to science and medicine.

High school student, Nimrit Aulakh, is completing her co-op placement with Lawson Scientist, Dr. Cheryl Forchuk. Her research focuses on improving mental health care for youth.
“Science has always been of interest to me and has now become significant within my academic endeavours. Part of my desire to become involved in the sciences stemmed from my older sister, who exposed me initially to the research side of science. It is with the help of rationale and logic in science that I can enrich my academic experience. Specifically, I have been working as a co-op student alongside the Mental Health Nursing Research Alliance and learning what it means to be a researcher. During my time, I conducted preliminary analyses on one of their studies, which focuses on improving mental health care for youth through virtual models of care. I will be presenting my findings at the Thames Valley Science and Engineering Fair later this month and if successful, will advance to the Canada Wide Science Fair. This experience has shown me a new side of science, one that I hope that I can continue to be a part of. I realized that through science and research, I can contribute to advancing society. To continue my journey through post-secondary education, I have applied to get my Bachelor’s in Health Sciences. Both within and beyond my four years of undergraduate studies, I hope to continue my contributions in serving the public through scientific research, as well as create an image for girls with the same interests as me, everywhere.”

Romaisa Pervez is a Research Assistant working with Lawson Scientist, Dr. Arlene MacDougall. She recently completed her Master of Science in Epidemiology and Biostatistics at Western University.
“I’m the student lead on a project that’s titled “Building a Sustainable Model and Evaluation for Psychological Rehabilitation in Kenya: An Implementation Study.” I’m working with the CREATE (Community Recovery Achieved Through Entrepreneurism) Kenya team to conduct a study to improve how we deliver, evaluate, and train persons with lived experience or community members to facilitate the Psychosocial Rehabilitation (PSR) Toolkit so it can be locally sustained in Kenya. I’ve travelled to Kenya twice during my Master’s to build relationships with stakeholders and conduct focus groups/interviews. My passion lies in understanding how we can implement upstream initiatives for mental health that are both sustainable and effective. Furthermore, I want to explore how we can find leverage points within the current mental health system in low to middle income countries and create innovative solutions. In the near future, I want to pursue medicine and further my knowledge and build stronger skills in this field.”

Dr. Kelly Anderson is an Associate Scientist at Children’s Health Research Institute, a program of Lawson. She is also Assistant Professor in the Department of Epidemiology & Biostatistics at the Schulich School of Medicine & Dentistry, Western University.
“I lead a research program in public mental health research, with a primary focus on young people experiencing a first onset of psychotic disorder. Together with my team, we are investigating the distribution and risk factors for psychotic disorders, prevention in early psychosis, and access to care and utilization of services in first-episode psychosis. My research program is centered around mentorship and training of students from all levels, and I work with trainees to foster high-level skills in the design and analysis of epidemiologic studies using large complex datasets. I am committed to fostering a culture of equity, diversity, and inclusion within my research team, and I advocate strongly for gender and early career representation for awards, scientific symposia, and other career opportunities. As a female scientist, I regularly mentor young women, both formally and informally, and due to the focus of my research, I also regularly work with trainees with lived experience of mental disorders. The diverse experiences and perspectives of these students both inspire and inform our work together.”

Dr. Michelle Barton-Forbes is an Associate Scientist at Lawson and a Physician at London Health Sciences Centre (LHSC) specializing in paediatric infectious diseases. She is also an Assistant Professor at the Schulich School of Medicine & Dentistry, Western University.
“My research program is focused on the clinical epidemiology of infectious diseases in children, particularly in vulnerable paediatric populations such as neonates and young infants. A secondary area of interest is in bacterial resistance and antimicrobial stewardship. Through engagement in multicentre research and contribution to national guideline development, I am able to make a difference in the management and prevention of common childhood infections nationally. The combination of intense passion for my subspecialty, inquisitive curiosity and a drive to better understand common childhood illnesses is infectious to my students. I motivate my students to excellence by inspiring them to believe in themselves and their ability to make a difference. My students are encouraged and challenged to find answers to unanswered questions and unexplained trends through research. As a proud Canadian and an immigrant from a nation that prides itself in its diversity, I believe that diversity is our strength. The Jamaican national motto “out of many one people” has framed my worldview and has influenced my practice.”

Dr. Eileen Crowley is a Scientist at Lawson and a Pediatric Gastroenterologist at LHSC. She is also an Assistant Professor at the Schulich School of Medicine & Dentistry, Western University.
“My research interests include pediatric inflammatory bowel disease (IBD), the genetics of IBD, big datasets, therapeutic drug monitoring clinical trial endpoints and precision medicine. My work has served to be better delineate the genetic phenotype of children with IBD as well as optimizing response to therapy in this age group. I engage students and motivate them to work with enthusiasm! My aim is to create learning opportunities that are active, collaborative and promote learning relationships. Once I have identified a student’s goal, it is easier to share and attain that goal. Within the research setting, I aim to maintain an environment where every student feels accepted, valued and safe. Sharing of ideas creates opportunities whilst also fostering a sense of personal belonging and achievement.”
To learn more about International Women’s Day, visit https://www.internationalwomensday.com/.
Investing in life-changing research
Through donor support, endowed research chairs are exploring and answering some of the most profound and complex research questions of our time.
Among cherished family photos and special mementos in the office of Jeremy Burton, PhD, is a slightly faded photo of a young woman. Burton points out the framed photo as he enthusiastically talks about his work. It’s a young Miriam Burnett, after whom the Miriam Burnett Chair in Urological Sciences is named. It’s also the first endowed research chair position Burton held at St. Joseph’s Health Care London (St. Joseph’s).
As the research chair for seven years, Burton speaks fondly about the relationship he has with the Burnett family and the crucial role their support has played in advancing his research.
“Thanks to their funding, we became one of the world leaders in urological microbiome research,” he says.
Endowed research chairs at St. Joseph’s receive consistent and sustainable funding so that research leaders and their teams can answer the most profound and complex health questions of our time.
For decades, donors have been inspired by the clinical research taking place at St. Joseph’s and have heavily invested in endowed research chairs. Today, St. Joseph’s Health Care Foundation manages seven endowed chairs focused on several areas, including molecular imaging, fetal and newborn growth and diabetes. Working in partnership with Western University, and with donor support, the foundation recently established four new endowed chairs in mobility, medical biophysics, medical imaging and ophthalmology.
“Medical research in Canada is chronically underfunded, and there is almost no sustainable funding for hospital-based research positions,” says Michelle Campbell, President & CEO, St. Joseph’s Health Care Foundation. “Private philanthropy has filled that gap for years. When a donor gives to an endowed research chair, they are building capacity in the present day and creating future value and opportunity. An endowed gift has a multiplier effect.”
Burton, now the endowed Research Chair in Human Microbiome and Probiotics, has many reasons to be grateful for this support. Not only does the endowed fund pay for Burton’s research salary, it also partially supports the salaries of a lab manager and technical team – all vital for a sophisticated lab to be successful.
The funding also provides the gift of time – a diminishing commodity for any busy research team.
“Scientists need more time to think,” says Burton, a Lawson Research Institute (Lawson) scientist. “We are incrementally being stretched in multiple directions, and the funding gives us the time to do what we are meant to do – find answers to important clinical questions and find solutions to medical problems.”
Distinguished Lawson scientist and university professor Cheryl Forchuk, PhD, wholeheartedly agrees. She recently completed her final term as The Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation & Recovery, another endowed position. As Chair, Forchuk provided scientific and administrative leadership to a large group of researchers based at St. Joseph’s Parkwood Institute focused on mental health, activity and mobility, and cognitive vitality and brain health.
Many research leaders, she explains, can afford to spend only two days a week on their own research projects. Endowed chair positions change that.
“Imagine travelling across the country to create a national study focused on homelessness, two days a week at a time,” she suggests candidly. “You couldn’t.”
Forchuk is referring to her landmark project to better understand how many people in Canada are homeless and who they are. The goal was to develop more accurate sources of data and recommend appropriate support and services. Her work is already resulting in important changes.
Today, Forchuk is embarking on another cross-country research project to find solutions related to homelessness for Canadian veterans who are women.
Like Forchuk, Burton’s Chair position requires him to provide operational and research leadership, including developing research networks and partnerships nationally and internationally to advance studies that will revolutionize care.
“As the Chair, I think it is important that I have wide-ranging projects that benefit people in our own community and beyond,” says Burton, who is optimistic about the outcomes of several of his team’s studies.
He recently partnered with London’s First Episode Mood and Anxiety Program to study the impact of fermented foods on the microbiome of young people taking medications for mental health conditions.
One of the side effects of these medications is weight gain, which deters some patients from taking it. By providing patients with slow-release apple cider capsules, which have similar properties to fermented foods and positively affect the microbiome, they have seen an overall improvement in participants’ mental health and cholesterol after just a few months.
Reflecting on his team’s research achievements to date and the potential of what’s to come, Burton emphasizes how vital endowed chairs are to the sustainability of research and the hope to translate newly discovered knowledge into medical practice.
“Research funding from other sources comes and goes,” he says, “but endowed chair positions that are focused on improving human health provide continuity, build research and create change benefiting all of us.”
iSee Vision Screening Program - Screening Session and Special Gift Announcement
Join the St. Joseph's Health Care Foundation and the Brandon Prust Foundation for a special gift announcement at the Stoney Creek YMCA on Monday, July 18 at 9:30 AM. This is also an opportunity to screen your children (aged 18 months to 4 years) for early signs of vision impairment through the iSee Vision Screening Program. Learn about the iSee Program by visiting the St. Joseph's Health Care London website.