Search
Search
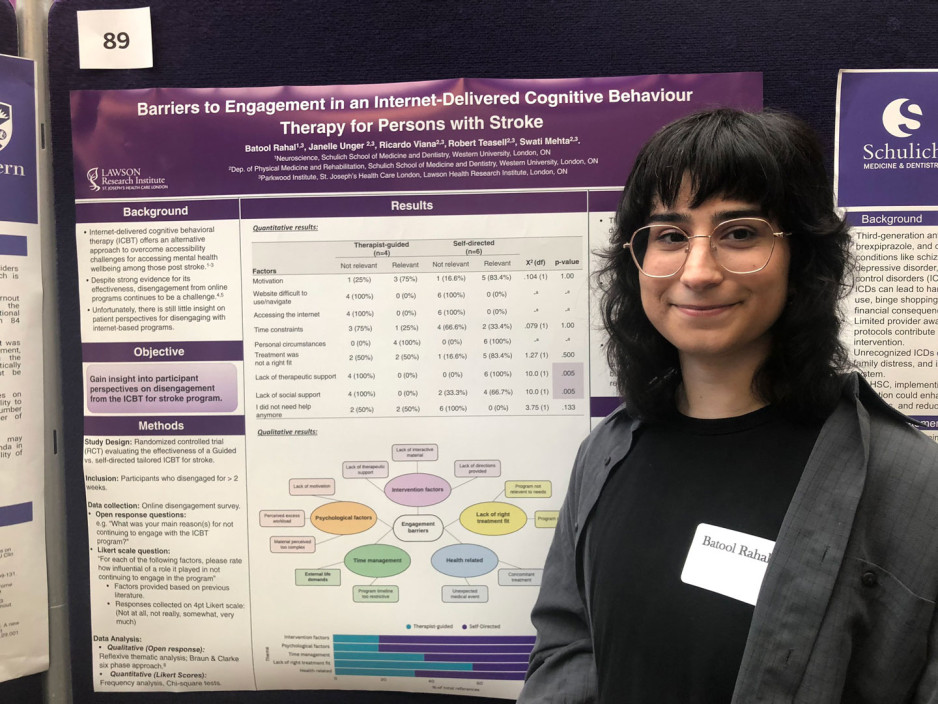
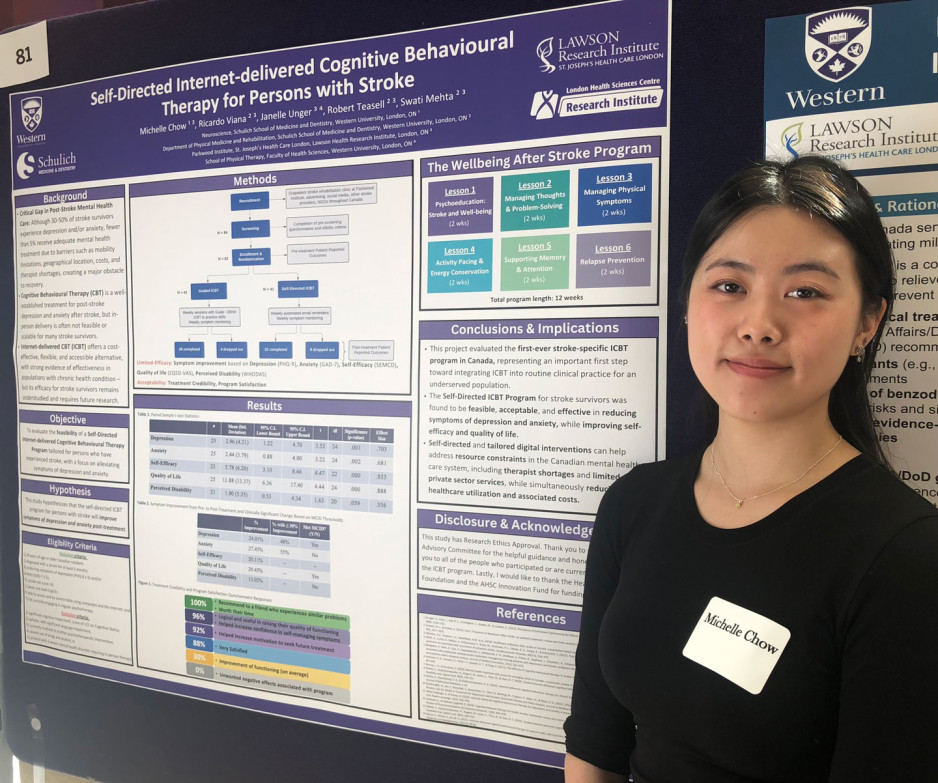
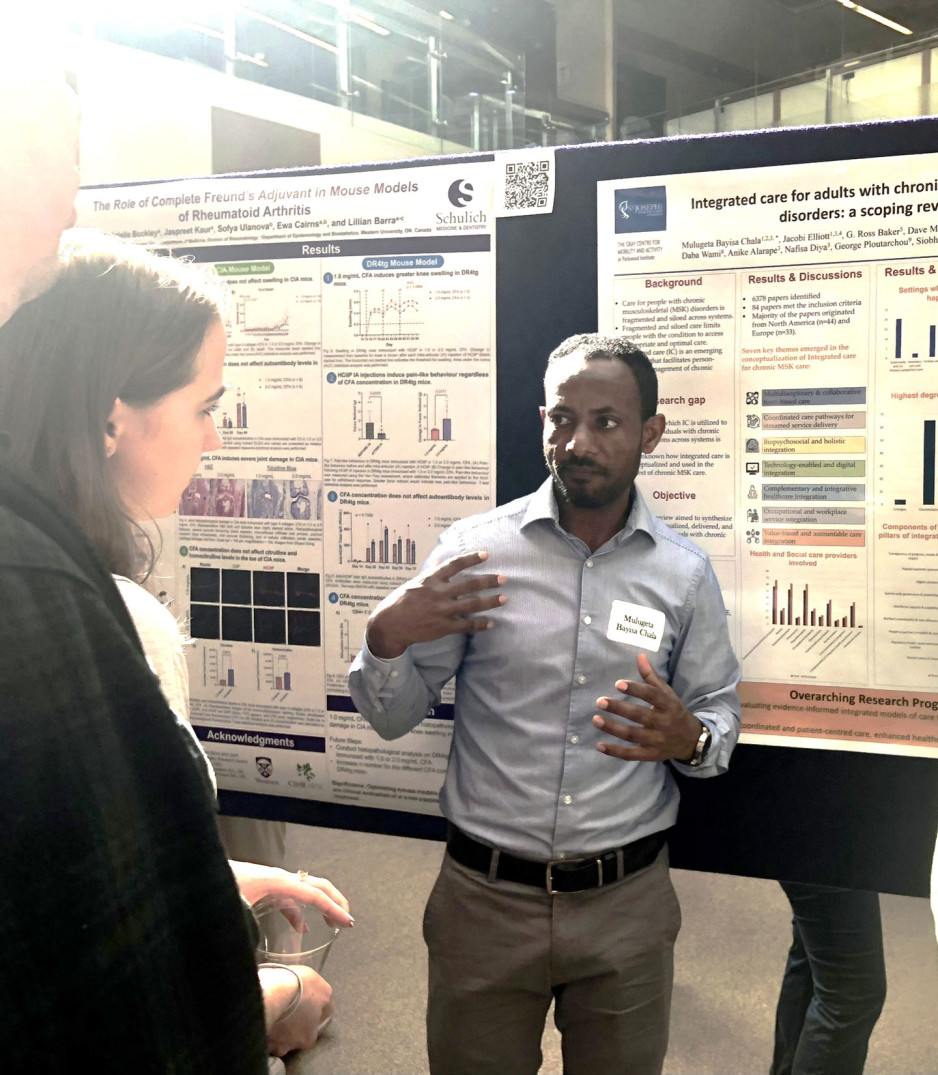
Student innovators showcase work at London Health Research Day 2025
The region’s largest celebration of emerging researchers’ work, London Health Research Day featured oral and poster presentations from undergraduates, grad students, postgraduates and trainees.
They shared their work with peers and globally renowned scientists in an array of specialized health and medical fields.
Their projects were as diverse as concussion treatment for children; large-language models to evaluate cancer diagnoses; brain imaging in people with dementia; and health system change to reduce surgical wait times.
Dozens of projects had Lawson Research Institute connections, included chronic pain’s impact on the brain; self-directed cognitive behavioural therapy for people recovering from stroke; and triaging care for people with shoulder injury.
Participants were also treated to a keynote address by Professor Francesca Ciccarelli, PhD, a global leader in cancer genomics who shared groundbreaking insights into the future of cancer research and precision medicine.
Her presentation was part of the Lucille and Norton Wolf Health Research Lecture Series through the generosity of the Bernard and Norton Wolf Family Foundation.
All told, about 500 people took in the day’s events, including several professional- and career-development workshops.
Student innovators showcase work at London Health Research Day 2025
The region’s largest celebration of emerging researchers’ work, London Health Research Day featured oral and poster presentations from undergraduates, grad students, postgraduates and trainees.
They shared their work with peers and globally renowned scientists in an array of specialized health and medical fields.
Their projects were as diverse as concussion treatment for children; large-language models to evaluate cancer diagnoses; brain imaging in people with dementia; and health system change to reduce surgical wait times.
Dozens of projects had Lawson Research Institute connections, included chronic pain’s impact on the brain; self-directed cognitive behavioural therapy for people recovering from stroke; and triaging care for people with shoulder injury.
Participants were also treated to a keynote address by Professor Francesca Ciccarelli, PhD, a global leader in cancer genomics who shared groundbreaking insights into the future of cancer research and precision medicine.
Her presentation was part of the Lucille and Norton Wolf Health Research Lecture Series through the generosity of the Bernard and Norton Wolf Family Foundation.
London Health Research Day is a shared project of Western’s Schulich School of Medicine & Dentistry, the Faculty of Health Sciences, Lawson Research Institute of St. Joseph's Health Care London and London Health Sciences Centre Research Institute.
All told, about 500 people took in the day’s events, including several professional- and career-development workshops.
Study shows fewer higher-dose radiation treatments safe and well tolerated by women with uterine cancer
MEDIA RELEASE
FOR IMMEDIATE RELEASE
Sunnybrook Health Sciences Centre and Lawson Health Research Institute
April 14, 2022
LONDON,ON - Five high-dose radiation treatments targeting uterine cancer rather than the current standard 25 treatments are safe and well-tolerated by patients, a new study published in JAMA Oncology has found.
SPARTACUS (Stereotactic Pelvic Adjuvant Radiation Therapy in Cancers of the Uterus) — a multi-institutional non-randomized controlled trial — looked to assess the feasibility and safety of using a specialized technique called stereotactic body radiation therapy (SBRT) for women with uterine cancer where instead of 25 treatments over five weeks, five treatments can be delivered over 1.5 weeks.
SBRT uses many precise beams of radiation to target tumours or cancerous cells. It uses a higher dose of radiation in a smaller number of treatments. It can be done on a standard linear accelerator, the machine that delivers radiation treatments.
Sixty-one women were enrolled in SPARTACUS at two centres — Sunnybrook Health Sciences Centre and the London Regional Cancer Program (LRCP) at London Health Sciences Centre (LHSC).
“Uterine cancer is a common cancer in women, usually treated with surgical removal followed by radiation and/or chemotherapy to reduce the risk of recurrence,” said Dr. Eric Leung, radiation oncologist at Sunnybrook’s Odette Cancer Centre. “External beam radiation is usually given over five weeks, and that can place a heavy burden on women who have to travel to a radiation centre every day, spend time away from home and work, and incur the financial burden of these factors as well.”
With a median follow-up of nine months, the patients enrolled in SPARTACUS reported an acceptable level of side effects from the radiation that resolved, and also reported a reasonable quality of life during treatment, Dr. Leung said.
“We were interested in examining the toxicity of the higher dose – would it affect the nearby bowels or bladder and place a heavy symptom burden on patients? We were pleased to find that patients reported their symptoms as manageable.”
“This study represents a novel way of treating uterine cancer in a shorter time. It was conducted mainly through the COVID pandemic and gave women a chance to receive treatment in less time with fewer visits to our centres,” said Dr. David D’Souza, radiation oncologist at LHSC and the study co-lead through Lawson Health Research Institute.
Patients will continue to be followed on the study for late side effects and further research is planned to further compare this more convenient schedule to the standard five-week course of radiation.
“This novel treatment could lead to a practice change that places less burden on patients and on the healthcare system,” Dr. Leung said. “Delivering radiation over the course of a week and half rather than over five weeks for patients facing uterine cancer would open up healthcare resources by reducing visits and usage of the linear accelerators.”
-30-
ADDIONAL QUOTES – Dr. David D’Souza:
“Giving radiation in a shorter time can have several advantages for both the patient and the health care system."
“Our study assessed the safety of delivering a higher dose of radiation in fewer treatments for patients with uterine cancer by adapting what has successfully been done for other types of cancer in the pelvis like prostate and rectal cancer.”
“This study was made possible with advances in treatment planning, radiation machine capabilities, and an outstanding radiation therapy program at LRCP.”
ABOUT LAWSON HEALTH RESEARCH INSTITUTE
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
ABOUT SUNNYBROOK HEALTH SCIENCES CENTRE
Sunnybrook Health Sciences Centre is inventing the future of health care for the 1.2 million patients the hospital cares for each year through the dedication of its more than 10,000 staff and volunteers. An internationally recognized leader in research and education and a full affiliation with the University of Toronto distinguishes Sunnybrook as one of Canada’s premier academic health sciences centres. Sunnybrook specializes in caring for high-risk pregnancies, critically-ill newborns and adults, offering specialized rehabilitation and treating and preventing cancer, cardiovascular disease, neurological and psychiatric disorders, orthopaedic and arthritic conditions and traumatic injuries. The Hospital also has a unique and national leading program for the care of Canada’s war veterans.
Media Contacts:
Celine Zadorsky
Communications & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. 75664
C: 519-619-3872
@email
Sunnybrook Health Sciences Centre
Communications & Stakeholder Relations
416-480-4040
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study to improve geriatric care in Ontario receives CIHR funding
The Canadian Institutes of Health Research (CIHR) has awarded a $100,000 grant to a project that aims to examine and improve the delivery of care for older adults.
Dr. Jacobi Elliott, Associate Scientist at Lawson Health Research Institute and Coordinator (Geriatrics) at St. Joseph’s Health Care London, has received a Priority Announcement award for her study titled “Implementation, Equity and Impact: Examining specialized geriatric care programs in Ontario.”
“It is critical to provide older adults with timely and equitable access to specialized geriatric care,” says Dr. Elliott. “However, waitlists are growing with the current aging population and there is an increased demand for these services.”
Currently 1.6 million older Canadians are considered to be living with frailty, and that number is expected to double over the next decade. Without adequate geriatric services, older adults living with frailty are more likely to need hospital care. The goal of this research is to examine specialized geriatric care programs in Ontario.
“Across Ontario, there are more than twelve different geriatric outreach models of care, but we have no clear understanding of how these models were developed, implemented or evaluated,” says Dr. Elliott. “It is critical to understand whether the existing services are meeting the needs and goals of the diverse older adult population.”
Dr. Elliott hopes that the project’s findings can be used to inform the development of future specialized geriatric care programs.
Congratulations also goes out to the Lawson Scientists who are receiving CIHR funding totaling nearly $2.5 million through Western University’s Schulich School of Medicine & Dentistry:
Dr. Pingzhao Hu with Dr. Samuel Asfaha
A deep learning approach to identify inhibitors of adherent invasive Escherichia coli in the pathogenesis of inflammatory bowel disease
Dr. Steven Laviolette
Understanding the Effects of Adolescent Nicotine Exposure on Increased Risk for Mood and Anxiety Disorders: Bridging the Gap from Pre-Clinical to Clinical Investigations
Dr. Aaron Ward with Dr. Stephen Pautler
Histopathology image analysis for prostate cancer prognosis after radical prostatectomy
CIHR Priority Announcement recipients:
Dr. Xiao Zhen Zhou and Dr. Doug Fraser
Identification of Novel Disease Drivers, Therapeutic Targets, and Biomarkers of Sepsis
Surgeries take 22 per cent longer in teaching hospitals: Ontario study
Patients undergoing common surgeries in teaching hospitals experience significantly longer surgical times, with durations that are 22 per cent longer on average in these academic centres. This is among the findings of a new study from the Institute for Clinical Evaluative Sciences (ICES) and the Lawson Health Research Institute that was published today in theCanadian Journal of Surgery.
“The ability to train new surgeons is undeniably an essential part of a sustainable healthcare system,” says Christopher Vinden, the study’s lead author who is an adjunct scientist at ICES and a surgeon at the London Health Sciences Centre. “However, we see that surgical instruction significantly lengthens the duration of a range of common procedures, raising important questions such as how to minimize patient risk during teaching procedures, and how to address Ontario funding models that currently don’t adjust for academic versus non-academic centres.”
The researchers examined anonymized records for all adult residents of Ontario who underwent any of 14 common surgical procedures from 2002 to 2012. Of the more than 700,000 surgeries looked at, 21 per cent were performed in a teaching hospital. Previous research has shown that teaching can be associated with longer surgeries, but the authors say this is the first study to examine the magnitude of this increase at a population level, and the first to adjust for patient, procedure and surgeon-related factors such as the experience of the attending surgeon.
They found that of the 14 procedures, hip and knee replacements were least impacted by teaching status, respectively taking 8 and 9 per cent longer (less than 10 minutes longer) in academic centres. However, for the more complex laparoscopic right hemicolectomy (removing the right side of the bowel, usually due to colon cancer) the procedure took 33 per cent longer (62 minutes longer) in teaching hospitals.
Overall, every procedure took longer in teaching hospitals, at a mean of 22 per cent longer duration.
To choose which procedures to investigate, the authors consulted a panel of experts who selected representative procedures that are common in both teaching and community settings. Procedures included laparoscopic cholecystectomy, right hemicolectomy, appendectomy, unilateral inguinal hernia repair, hysterectomy, hip hemiarthroplasty, open reduction and internal fixation for hip fracture, hip and knee arthroplasty, and tonsillectomy. Where applicable, they considered open and laparoscopic procedures separately.
The study authors note that academic centres tend to use dedicated surgical teams for hip and knee replacements, compared to community hospitals where these procedures are typically performed by general orthopedic surgeons in non-dedicated units. They say it’s likely that this team-based specialist approach is helping to shave off that excess teaching time for knee and hip surgeries, and suggest that it may be useful to explore whether these efficiencies can be achieved for other common surgeries in teaching hospitals by adopting specialized units.
Noting that longer surgical durations have been linked to negative patient outcomes, Vinden adds: “In addition to addressing funding gaps created by longer procedure durations at teaching hospitals, it will be vitally important to identify at what point, for each type of surgery, this longer duration due to teaching introduces excess patient risk, and to find ways to minimize this risk. Training the next generation of surgeons should not negatively impact the funding of a teaching hospital, or the health of our patients.”
The study “Teaching surgery takes time: the impact of surgical education on time in the operating room” was published today in the Canadian Journal of Surgery.
Author block: Christopher Vinden, Richard Malthaner, Jacob McGee, J Andrew McClure, Jennifer Winick-Ng, Kuan Liu, Danielle M Nash, Blayne Welk, Luc Dubois.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
The Institute for Clinical Evaluative Sciences (ICES) is an independent, non-profit organization that uses population-based health information to produce knowledge on a broad range of health care issues. Our unbiased evidence provides measures of health system performance, a clearer understanding of the shifting health care needs of Ontarians, and a stimulus for discussion of practical solutions to optimize scarce resources. ICES knowledge is highly regarded in Canada and abroad, and is widely used by government, hospitals, planners, and practitioners to make decisions about care delivery and to develop policy. For the latest ICES news, follow us on Twitter: @ICESOntario
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
SWAHN Presents: Choosing Wisely in Southwestern Ontario - A Knowledge Exchange Forum
Objectives of the day:
- To encourage knowledge exchange concerning the implementation of Choosing Wisely Canada projects – featuring special presentations by representatives from North York General Hospital and St. Michael’s Hospital in Toronto as well as local organizations in the SWAHN region;
- To foster networking and collaboration among participants to discuss how the information shared by forum presenters concerning best practices can be translated to organizations in the SWAHN region;
- To obtain recommendations for SWAHN’s next steps concerning its role in promoting and advancing Choosing Wisely initiatives in the region.
Registration Fee: $75.00 + HST = $84.75
(Students/Residents: $25 + HST = $28.25)
Deadline to Register: April 28, 2017.
Space is limited so register early!
To register please complete the information in the attached form and submit the information as indicated.
For more information contact Catherine Joyes, SWAHN Manager: @email.
The SouthWestern Academic Health Network (SWAHN) seeks to transform health in Southwestern Ontario through integrated excellence in research, education, and clinical practice. For more information please visit www.swahn.ca.
Team players: FMT and microbiome research could have widespread impact
There is still much to learn about the human microbiome and its role in fighting disease, but ongoing studies at Lawson Health Research Institute, including a focus on fecal microbial transplants (FMT), are making strides in harnessing this complex system.
FMT is being studied in connection with conditions as varied as non-alcoholic fatty liver disease, rheumatoid arthritis, atherosclerosis, HIV, cancer and multiple sclerosis.
FMT is already in clinical use for the treatment of C. diff (Clostridium difficile), and in addition to showing promise in the treatment of other diseases, it is also being studied as a way to improve response to existing cancer treatments and ease treatment side effects.
Dr. Saman Maleki, a Scientist at Lawson Health Research Institute and the London Regional Cancer Program (LRCP) at London Health Sciences Centre (LHSC), says they’ve just begun to explore the possibilities.
"We are just starting to study FMT as an intervention outside its traditional use in patients with C. difficile infection, and we will be expanding to other areas, particularly in cancer.”
FMT can overhaul a patient’s microbiome, Dr. Maleki explains, and a healthy microbiome is beneficial especially when a treatment is trying to activate the body’s immune system.
Dr. Michael Silverman, Lawson Associate Scientist and Medical Director of St. Joseph’s Health Care London’s Infectious Diseases Care Program, is a pioneer in the field of FMT. He has been performing the procedure since 2003 with C. difficile patients and was one of the first in North America to do so. He sees a wide range of possible applications.
“FMT has enormous potential in being an important adjunctive therapy in many cancers. It may, for example, help cancer patients respond to immunotherapy,” says Dr. Silverman, who is also Chair/Chief of Infectious Disease at St. Joseph’s Health Care London, LHSC and Western University. “The potential to impact autoimmune and metabolic diseases is also quite exciting, but still in early development.”
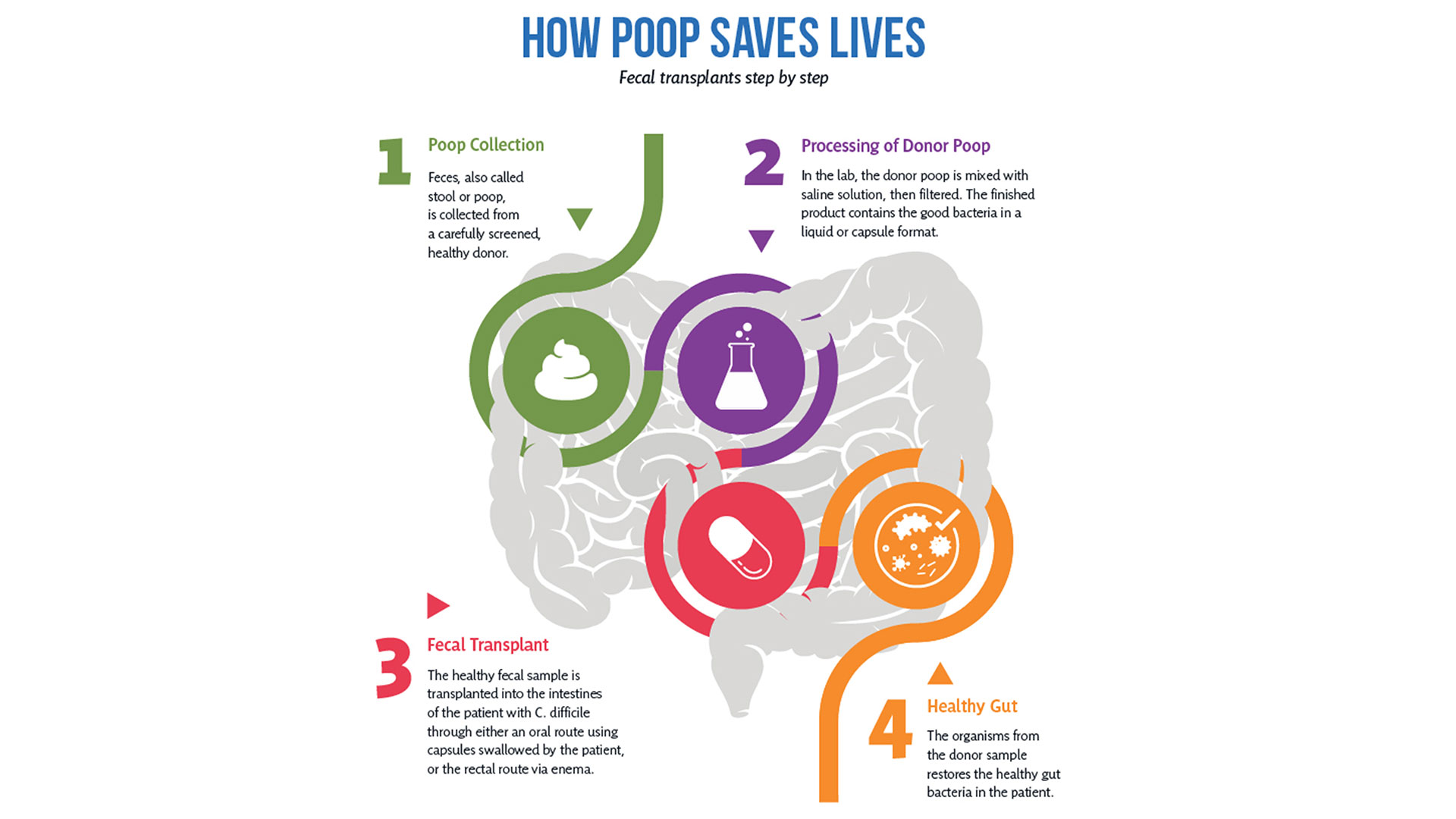
So how does it work?
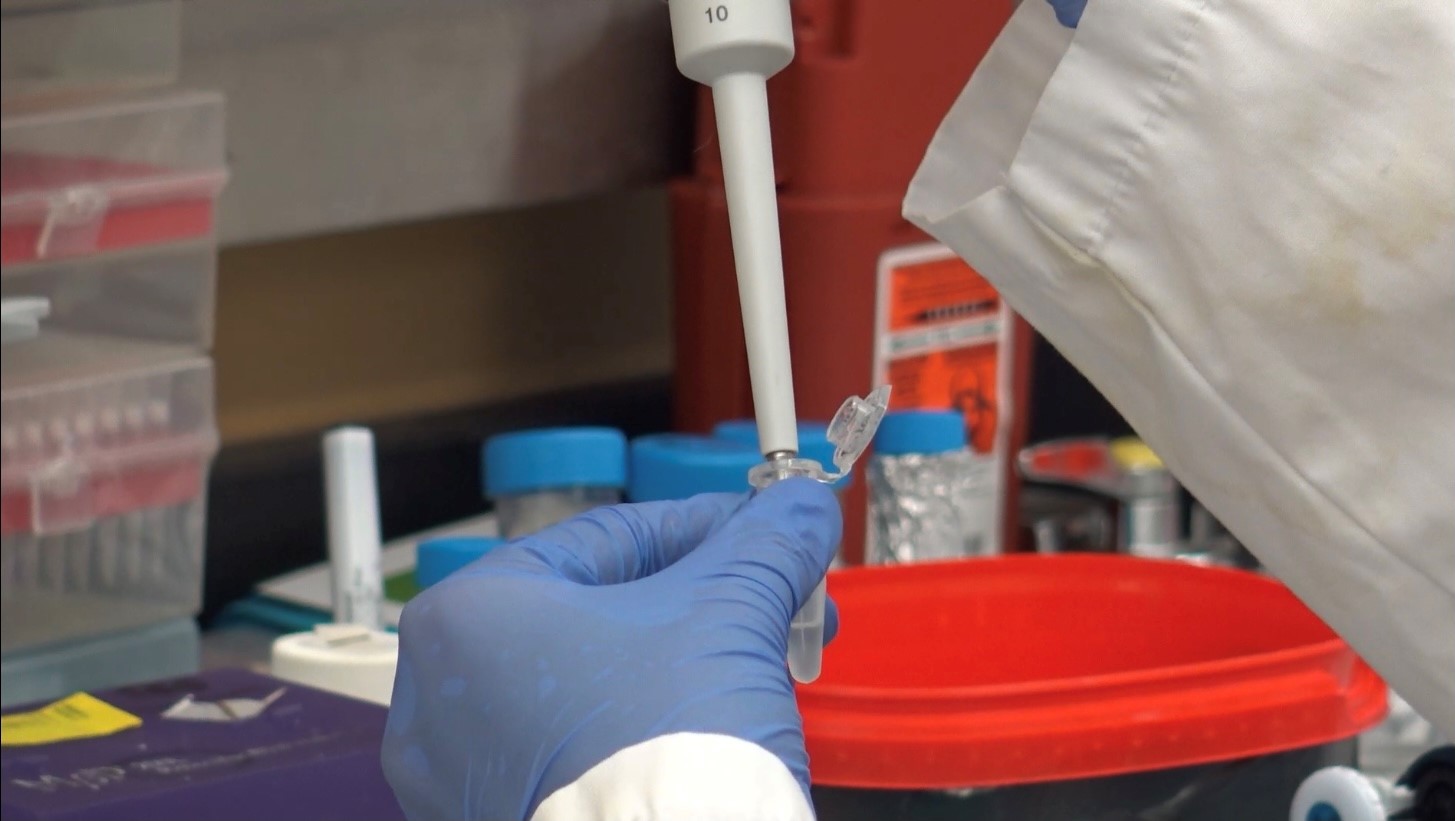
After rigorous screening, stool from a healthy donor is collected and then processed in a lab into a liquid or capsule containing the good bacteria, which can then be administered to a patient’s gastrointestinal tract.
The Lawson team is also one of few delivering FMT using specially-prepared oral capsules. Introduced in 2018, they have been a game changer in patient acceptance and ease of administration, according to Research Coordinator Dr. SeemaNair Parvathy, who has been coordinating the program since 2015.
“There is a link between the fitness of the intestinal microbiome and the fitness of the immune system,” says Dr. John Lenehan, Associate Scientist at Lawson and Medical Oncologist at LHSC. “A ‘healthy’ microbiome leads to a more robust immune response when using immunotherapy. FMT from a healthy donor is expected to improve the fitness of the recipient’s intestinal microbiome and promote a better immune response.”
People with chronic disease can often experience what’s called a ‘leaky gut,’ allowing food, bacterial and microbial components to pass through the intestinal wall, negatively impacting the immune system.
“When people get FMTs their intestinal permeability improves – meaning it actually reduces,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at Lawson and St. Joseph’s. “What changes that intestinal permeability? The microbes at the site. They play a role in interacting with the host cells, providing nutrients and vitamins.”
With the immune system so closely tied to the health of the microbiome, it’s not surprising scientists are exploring how strengthening one can have a big impact on the other.
Boosting immunotherapy
Immunotherapy can be used to either stimulate or suppress the immune system to help the body fight disease, and FMT is showing promise in reducing resistance to the treatment.
While immunotherapy has been effective in treating a number of cancers – the number one cause of death in Canada – not all patients respond to the treatment.
But early work presented at a conference by the Lawson team for the Journal for ImmunoTherapy of Cancer has shown that using FMT to modify the microbiome could reduce resistance to immunotherapy. The study involved patients from LHSC with advanced melanoma, a type of skin cancer.
While in the very early stages, the combination of FMT and anti-PD1 immunotherapy has been found to be safe, and it appears that FMT could make tumours more responsive to the immunotherapy treatment.
“Microbiome-based treatment strategies, including FMT, have a high potential in oncology,” says Dr. Maleki. “Our team is also exploring its potential in treating pancreatic cancer.”
The research is so interesting that a recent Nature article listed the Phase I melanoma trial as “seminal” research. The study was also unique in that it used healthy donors, as opposed to donors who had previously responded to immunotherapy treatment.
A separate Lawson study with LHSC patients with metastatic renal cell carcinoma, a type of kidney cancer, published in the Journal of Clinical Oncology, also looked at combining immunotherapy and FMT to ease the adverse effects of the treatment.
The Phase I study, led by Dr. Maleki and Dr. Ricardo Fernandes, Medical Oncologist at LHSC, found adding FMT to doublet immunotherapy was safe, but further study is needed to determine whether it could bring about changes in the microbiome and immune system.
Dr. Lenehan says Lawson researchers are in a position to be leaders in this field in the near future for two reasons.
“One is that other academic researchers have not been able to assemble the expertise, and some who have, do not have the access to healthy donor stool. The second is that some biotechnology companies are interested in FMT, but almost exclusively for C. difficile infections.”
Autoimmune, metabolic and other illnesses
Two other areas that have seen recent advances include FMT for the treatment of non-alcoholic fatty liver disease (NAFLD) and multiple sclerosis.
“The gut microbiome is very important in the metabolism of foods and metabolic products. It can therefore have a major effect on obesity and atherosclerosis,” says Dr. Silverman. “It also is tightly involved in regulating the immune system and therefore moderating the microbiome may potentially impact autoimmune diseases.”
A study published in 2020 by the team in The American Journal of Gastroenterology showed that FMT appears to reduce intestinal permeability in patients with NAFLD.
The number of people with NAFLD is growing rapidly and studies show patients have different microbiota than healthy persons.
The trial included 21 NAFLD patients from LHSC and St. Joseph’s. While the researchers found no changes in percentage of liver fat or insulin resistance, they observed significant reduction in intestinal permeability in those patients who had elevated intestinal permeability at the study’s start (seven patients in total). They also observed changes to the gut microbiome in all patients who received a fecal transplant from a healthy donor.
“Metabolic syndromes including obesity and its complications of NAFLD and atherosclerosis are massive public health problems. Any impact on these would be of huge importance,” Dr. Silverman adds. “Autoimmune diseases also cause major morbidity and mortality. We have a lot of work to do before we can consider FMT as a routine therapy for any of these conditions, but the long-term promise is great.”
Research into the use of FMT for treatment of patients with multiple sclerosis is in the very early stages. But patients with MS show a difference in gut microbiota and higher small intestine permeability, which could contribute to the development of the disease.
A Phase I trial by the Lawson team published in the Multiple Sclerosis Journal – Experimental, Translational and Clinical, found FMT to be safe and tolerable.
While the study was very small, MS patients treated with FMT were found to have beneficial changes to gut microbiota and intestinal permeability, but further study is needed to determine if FMT could be used as a treatment.
Lawson scientists are also currently studying the use of FMT for patients with atherosclerosis, along with ongoing studies on melanoma and lung cancer. Funding for a study on pancreatic cancer has been secured and researchers are in the process of planning trials for a number of other applications.
Dr. Lenehan says, “The microbiome is connected to several diseases and their treatments. Evidence is growing that an individual’s health is related to their microbiome.”

The donor challenge
The challenge of finding fecal donors for FMT and the cost of that process remain an issue for research into this promising treatment, even as more potential applications are discovered.
There is currently no process in place to match donors and recipients – as with organ donation – but there is an extensive screening process for both infectious and non-infectious conditions, one that needs to be repeated if a donor experiences any lifestyle changes.
Dr. Burton says, “We still don't understand the full role of the microbiota. We have to ensure that we're not giving patients a microbiota that might cause them some other issue in the future, so the donors are screened very thoroughly for that.”
Screening also excludes donors with an increased risk of developing the diseases scientists are hoping to treat, such as metabolic syndrome related conditions.
A 2017 article published in Open Forum Infectious Diseases by Drs. Silverman and Burton found the cost of screening high numbers of potential donors could make establishing local programs extremely difficult, so having a central program such as the one in London could help patients in many regions.
In the study, only five of 46 potential donors passed the history, examination, blood, stool and urine tests, and of the five, four later travelled or had illnesses that made donation inadvisable.
The search continues in London for potential donors to help drive this research forward. You can read one donor’s story and learn how you can get involved here.
More on FMT and the microbiome:
Drugs vs. bugs: Harnessing the microbiome to improve treatments
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
Top 12 research stories of 2022
As the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, our teams impact the lives of people in Ontario, Canada and around the globe with groundbreaking studies, world firsts and translational research that enhances care, health and wellbeing. Here are some of Lawson Health Research Institute’s top research highlights of 2022.
Researchers looking to better personalize treatment for PTSD

In a new study through Lawson and Western University’s Schulich School of Medicine & Dentistry, scientists are looking at a form of treatment called deep brain reorienting (DBR) for those suffering from post-traumatic stress disorder (PTSD). Read more.
Virtual care associated with significant environmental and patient cost savings

A new study by researchers at ICES, Lawson and Western finds that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs. Read more.
Novel test that could easily diagnose blast injury created by local scientists

In a world first, researchers at Lawson and Defence Research and Development Canada have developed a breath test that could be used to diagnose repetitive blast injury – a mild traumatic brain injury resulting from pressure changes that occur during explosions. The device will soon go through clinical trials to validate its efficacy. Read more.
Local researchers using artificial intelligence to lead the way in bedside lung imaging
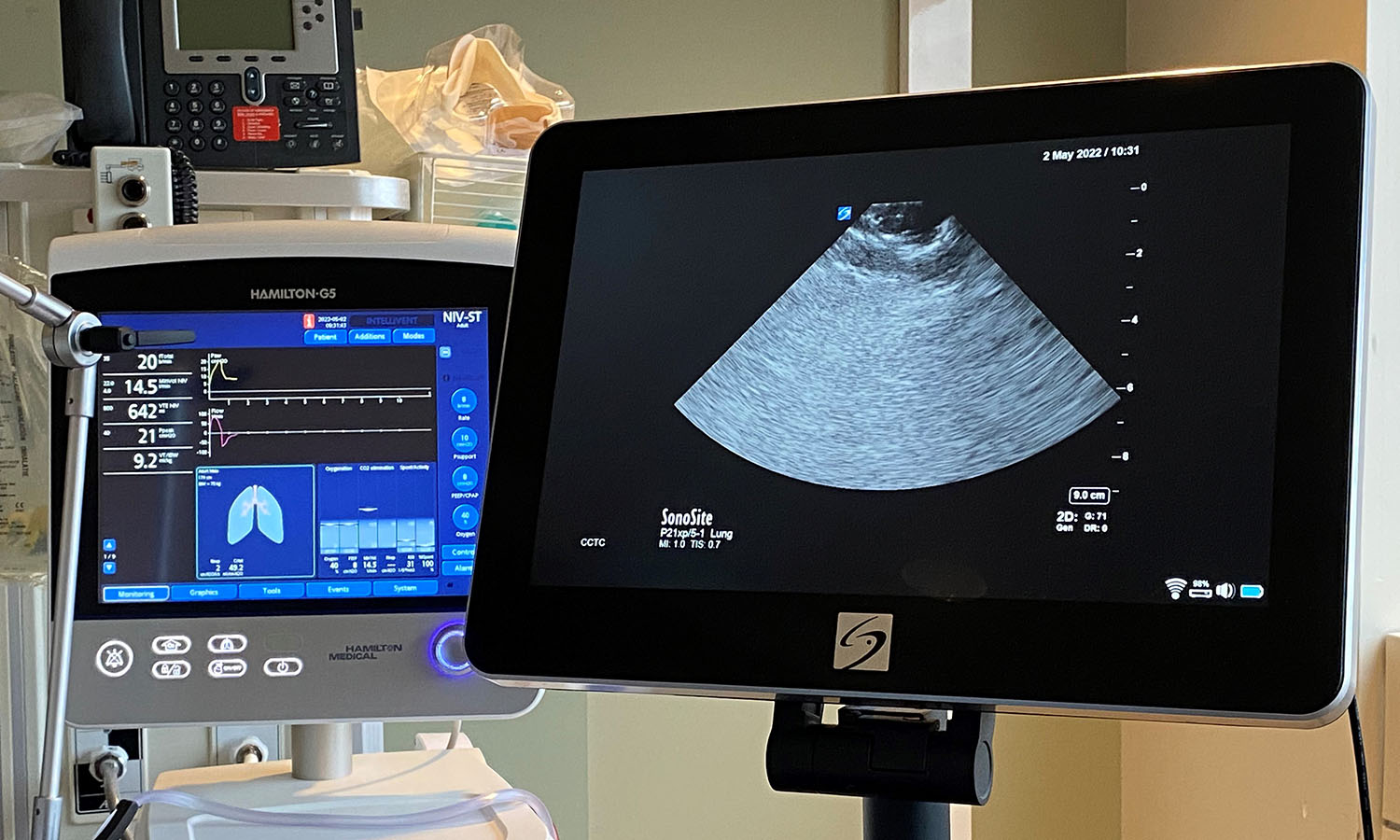
A team at Lawson is testing a new form of artificial intelligence (AI), paired with portable ultrasound machines, to image and identify lung concerns in real time, right at the beside of critically ill patients. Approximately 100 critical care patients at LHSC will be part of this study. Read more.
New tool shows promise in helping people manage traumatic brain injuries one pace at a time

A team at Lawson has developed a new app called MyBrainPacer™ which aims to better assist and treat those living with mild traumatic brain injuries (mTBI), including concussions. mTBI may come with lasting effects that can alter a person’s life. Although a person with a mTBI may appear fine on the outside, many have to pace their day-to-day activities in order to allow the time needed for the brain to properly heal. Much like point tracking used by dieters to monitor food choices, through MyBrainPacer™ App, users can assign values to tasks like driving, grocery shopping, screen use and exercise so they can plan and pace their daily activity. Read more.
Study shows a decline in Veterans' mental health throughout the pandemic

When it comes to mental health conditions, Veterans are an at-risk population, often having higher rates of depression and post-traumatic stress disorder (PTSD). When the COVID-19 pandemic hit, scientists at Lawson wanted to understand its effects on this already at-risk population. They found that more than half of Canadian Veterans reported a decline in their mental health. Read more.
Growing evidence that PSMA imaging improves prostate cancer detection
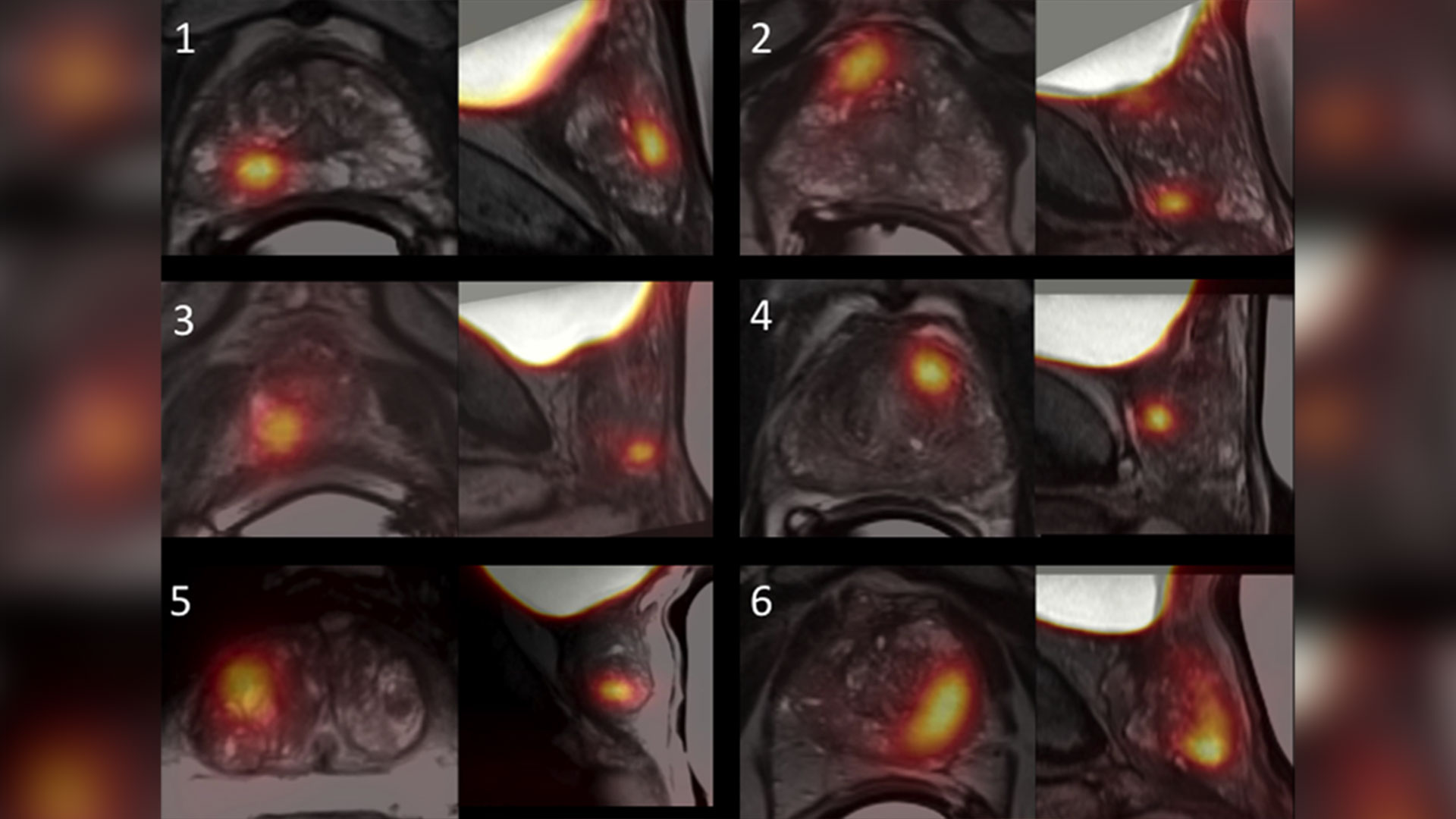
Scientists at Lawson are leading the way in using specialized imaging to detect prostate cancer – the fifth leading cause of cancer death in men around the world. Early evidence indicates that PSMA PET scans have changed how prostate cancer is being treated, but more work is underway to understand the impact of those treatment changes. Read more.
Leveraging virtual reality to manage pain in paediatric patients

A study underway through Lawson and Children’s Hospital at LHSC is using virtual reality (VR) to help paediatric patients during painful and distressing procedures. The study is focusing on paediatric patients who need port access. A port is a little reservoir that sits underneath the skin that allows access to blood or medication with the use of a needle. Ports are most commonly used in paediatric cancer patients. Read more.
Team players: FMT and microbiome research could have widespread impact

There is still much to learn about the human microbiome and its role in fighting disease, but ongoing studies at Lawson, including a focus on fecal microbial transplants (FMT), are making strides in harnessing this complex system. FMT is being studied in connection with conditions as varied as non-alcoholic fatty liver disease, rheumatoid arthritis, atherosclerosis, HIV, cancer and multiple sclerosis. Read more.
London researchers adapt MRI technology to image salt within the kidneys

Scientists at Lawson have adapted PET/MRI technology to accurately image salt within the kidneys of patients with kidney disease. Imaging salt within the kidneys has never been accurately accomplished in patients with kidney disease, but Dr. McIntyre and his team developed new technology and software that was adaptable to a PET/MRI machine at St. Joseph’s. Read more.
London researchers discover novel method to diagnose long COVID
Published in Molecular Medicine, researchers at Lawson have found that patients with post-COVID-19 condition (long COVID) have unique biomarkers in their blood. The team is now working on developing a first of its kind blood test that could be used to diagnose long COVID. The discovery could also lead to new therapeutics for this condition. Read more.
Largest trial ever done in hemodialysis care examines optimal dialysis temperature

Published in the Lancet findings from a large clinical trial through Lawson, ICES Western and Western University suggest that lowering dialysis temperatures does not lead to improved patient outcomes, despite previous studies suggesting otherwise. Read more.
To learn more about Lawson research studies, please visit our News and Media page
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca