Search
Search
Fast Facts
- Vision: Lawson will be pivotal in preventing the onset and reducing the burden of disease through the acquisition, evaluation and translation of new scientific knowledge
- Year Established: 2000
- Number of Research Personnel: Over 2,060 principal investigators, support staff, volunteers, students and fellows
- Our Hospitals: London Health Sciences Centre and St. Joseph’s Health Care London
- Key Affiliations: Western University, including the Schulich School of Medicine & Dentistry, Robarts Research Institute and the Faculty of Health Sciences.
- Number of Worldwide Partners: Over 600 business and industry partners in more than 25 countries.
- Current Funding: Attracts over $118 million in annual research income
- Space: Over 250,000 square feet of research space within London, Ontario
- Projects: Partners on more than 600 research projects annually
- Publications: Over 1000 peer-reviewed original publications per year, cited more than 10,000 times annually
- Number of National and World Firsts: 100+
- Active Clinical Studies: Over 2,245 clinical studies
- Current Active Clinical Research Participants: 4,386
- Ranking: 8th in the country of Canada’s Top 40 Research Hospitals
Fecal transplants show promise as treatment for non-alcoholic fatty liver disease
LONDON, ON – A new study from Lawson Health Research Institute and Western University suggests that fecal transplants could be used as a treatment for non-alcoholic fatty liver disease (NAFLD). The randomized controlled trial published in The American Journal of Gastroenterology found that fecal transplants in patients with NAFLD result in a reduction in how easily pathogens and other unwanted molecules pass through the human gut and into circulation, known as intestinal permeability. The results could have implications for the treatment of numerous conditions including metabolic syndrome and autoimmune diseases.

“Intestinal permeability plays a role in the development of metabolic syndrome which is a major cause of coronary and cerebrovascular disease. It has also been associated with autoimmune diseases like multiple sclerosis (MS), rheumatoid arthritis, systemic lupus and type 1 diabetes,” explains Dr. Michael Silverman, Associate Scientist at Lawson and Professor at Western’s Schulich School of Medicine & Dentistry.
Many NAFLD patients have increased intestinal permeability which triggers inflammation, increased fat in the liver, insulin resistance and elevated levels of triglycerides in the blood. The human microbiome – the diverse collection of microbes in our body – is thought to play a role. Previous studies have shown differences between the gut microbiome of NAFLD patients compared to healthy individuals.
“Our team wondered whether we could change the gut microbiome of NAFLD patients to reduce intestinal permeability,” says Dr. Jeremy Burton, Lawson Scientist and Associate Professor at Schulich Medicine & Dentistry.
The trial included 21 NAFLD patients from London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London. Patients were randomized to receive a fecal transplant using stool from a healthy donor or a placebo (the patient’s own stool). Fecal material was delivered to the small intestine using endoscopy. Patients were followed for six months to assess changes to their gut microbiome, intestinal permeability, percentage of liver fat and insulin resistance.
While the researchers found no changes in percentage of liver fat or insulin resistance, they observed significant reduction in intestinal permeability in those patients who had elevated intestinal permeability at the study’s start (seven patients in total). They also observed changes to the gut microbiome in all patients who received a fecal transplant from a healthy donor.
“Our study demonstrates that intestinal permeability can be improved through fecal transplant from a healthy donor,” says Dr. Laura Craven, a recent PhD graduate from Schulich Medicine & Dentistry and first author on the published study. “This suggests that fecal transplant could be used as an early intervention in the treatment of NAFLD to reduce intestinal permeability and prevent inflammation”
“Our findings have implications for other conditions too,” adds Dr. Silverman, who is also Chair/Chief of Infectious Diseases at Western, LHSC and St. Joseph’s. “Changing the gut microbiome could hold promise in preventing and treating metabolic syndrome and autoimmune diseases associated with increased gut permeability.”
The team hopes to next conduct a large multi-centre trial to further investigate FMT as an intervention for NAFLD and as a therapy to reduce intestinal permeability.
NAFLD is an obesity-related disorder and is the second-leading cause of liver transplant in North America. While reversible if treated early, its progression can lead to liver failure or cancer. Current therapies are not overly effective and the prevalence of NAFLD is increasing.
Dr. Silverman is a pioneer in the field of fecal transplants, including their use as a treatment for Clostridioides difficile (C. diff). He is involved in multiple studies examining the potential of fecal transplants as treatments or supportive therapies for numerous conditions including multiple sclerosis (MS) and different types of cancer.
“In order to conduct this research, we need stool donors,” notes Dr. Silverman. “By donating your poop, you can help us assess the value of fecal transplants to treat a variety of diseases.”
The team is in need of young, healthy stool donors for fecal transplants. All donors are required to go through a screening process. Those interested in becoming a stool donor can contact Dr. Seema Nair Parvathy, Research Coordinator, Fecal Transplant Program, at 519-646-6100 ext. 61726.
-30-
DOWNLOADABLE MEDIA
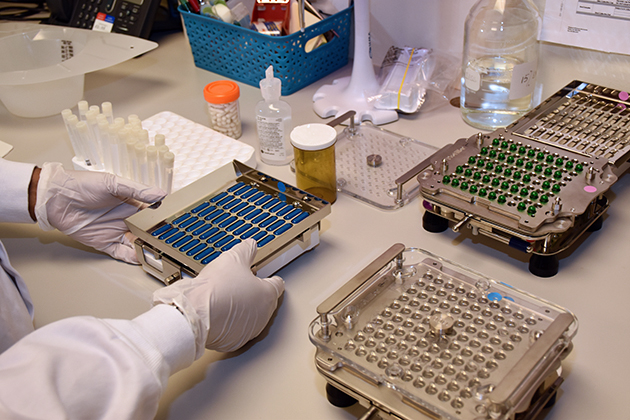
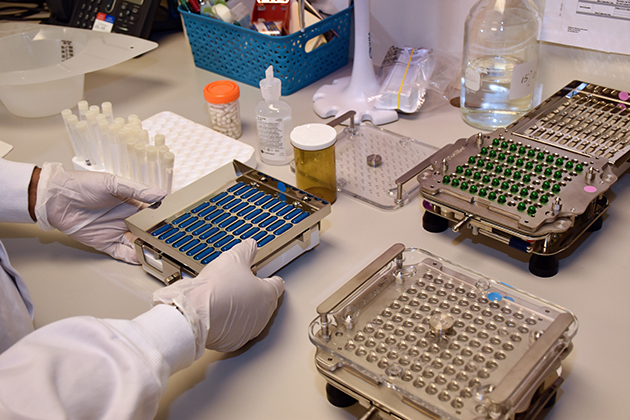
Stool samples being prepared in the lab.

Dr. Michael Silverman (left) and Dr. Jeremy Burton (right)

Dr. Laura Craven
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Fecal transplants show promise as treatment for non-alcoholic fatty liver disease
A new study from Lawson Health Research Institute and Western University suggests that fecal transplants could be used as a treatment for non-alcoholic fatty liver disease (NAFLD). The randomized controlled trial published in The American Journal of Gastroenterology found that fecal transplants in patients with NAFLD result in a reduction in how easily pathogens and other unwanted molecules pass through the human gut and into circulation, known as intestinal permeability. The results could have implications for the treatment of numerous conditions including metabolic syndrome and autoimmune diseases.
“Intestinal permeability plays a role in the development of metabolic syndrome which is a major cause of coronary and cerebrovascular disease. It has also been associated with autoimmune diseases like multiple sclerosis (MS), rheumatoid arthritis, systemic lupus and type 1 diabetes,” explains Dr. Michael Silverman, Associate Scientist at Lawson and Professor at Western’s Schulich School of Medicine & Dentistry.
Many NAFLD patients have increased intestinal permeability which triggers inflammation, increased fat in the liver, insulin resistance and elevated levels of triglycerides in the blood. The human microbiome – the diverse collection of microbes in our body – is thought to play a role. Previous studies have shown differences between the gut microbiome of NAFLD patients compared to healthy individuals.

“Our team wondered whether we could change the gut microbiome of NAFLD patients to reduce intestinal permeability,” says Dr. Jeremy Burton, Lawson Scientist and Associate Professor at Schulich Medicine & Dentistry.
The trial included 21 NAFLD patients from London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London. Patients were randomized to receive a fecal transplant using stool from a healthy donor or a placebo (the patient’s own stool). Fecal material was delivered to the small intestine using endoscopy. Patients were followed for six months to assess changes to their gut microbiome, intestinal permeability, percentage of liver fat and insulin resistance.
While the researchers found no changes in percentage of liver fat or insulin resistance, they observed significant reduction in intestinal permeability in those patients who had elevated intestinal permeability at the study’s start (seven patients in total). They also observed changes to the gut microbiome in all patients who received a fecal transplant from a healthy donor.
“Our study demonstrates that intestinal permeability can be improved through fecal transplant from a healthy donor,” says Dr. Laura Craven, a recent PhD graduate from Schulich Medicine & Dentistry and first author on the published study. “This suggests that fecal transplant could be used as an early intervention in the treatment of NAFLD to reduce intestinal permeability and prevent inflammation”

Dr. Laura Craven
“Our findings have implications for other conditions too,” adds Dr. Silverman, who is also Chair/Chief of Infectious Diseases at Western, LHSC and St. Joseph’s. “Changing the gut microbiome could hold promise in preventing and treating metabolic syndrome and autoimmune diseases associated with increased gut permeability.”
The team hopes to next conduct a large multi-centre trial to further investigate FMT as an intervention for NAFLD and as a therapy to reduce intestinal permeability.
NAFLD is an obesity-related disorder and is the second-leading cause of liver transplant in North America. While reversible if treated early, its progression can lead to liver failure or cancer. Current therapies are not overly effective and the prevalence of NAFLD is increasing.
Dr. Silverman is a pioneer in the field of fecal transplants, including their use as a treatment for Clostridioides difficile (C. diff). He is involved in multiple studies examining the potential of fecal transplants as treatments or supportive therapies for numerous conditions including multiple sclerosis (MS) and different types of cancer.
“In order to conduct this research, we need stool donors,” notes Dr. Silverman. “By donating your poop, you can help us assess the value of fecal transplants to treat a variety of diseases.”
The team is in need of young, healthy stool donors for fecal transplants. All donors are required to go through a screening process. Those interested in becoming a stool donor can contact Dr. Seema Nair Parvathy, Research Coordinator, Fecal Transplant Program, at 519-646-6100 ext. 61726.

Drs. Michael Silverman (left) and Jeremy Burton (right)
Fecal transplants show promise in improving melanoma treatment
LONDON, ON – In a world-first clinical trial published in the journal Nature Medicine, a multi-centre study from Lawson Health Research Institute, the Centre hospitalier de l’Université de Montréal (CHUM) and the Jewish General Hospital (JGH) has found fecal microbiota transplants (FMT) from healthy donors are safe and show promise in improving response to immunotherapy in patients with advanced melanoma.
Immunotherapy drugs stimulate a person’s immune system to attack and destroy cancer. While they can significantly improve survival outcomes in those with melanoma, they are only effective in 40 to 50 per cent of patients. Preliminary research has suggested that the human microbiome – the diverse collection of microbes in our body – may play a role in whether or not a patient responds.
“In this study, we aimed to improve melanoma patients’ response to immunotherapy by improving the health of their microbiome through fecal transplants,” says Dr. John Lenehan, Medical Oncologist at London Health Sciences Centre’s (LHSC) London Regional Cancer Program (LRCP), Associate Scientist at Lawson and Associate Professor in the Department of Oncology at Western University’s Schulich School of Medicine & Dentistry.
A fecal transplant involves collecting stool from a healthy donor, screening and preparing it in a lab, and transplanting it to the patient. The goal is to transplant the donor’s microbiome so that healthy bacteria will prosper in the patient’s gut.
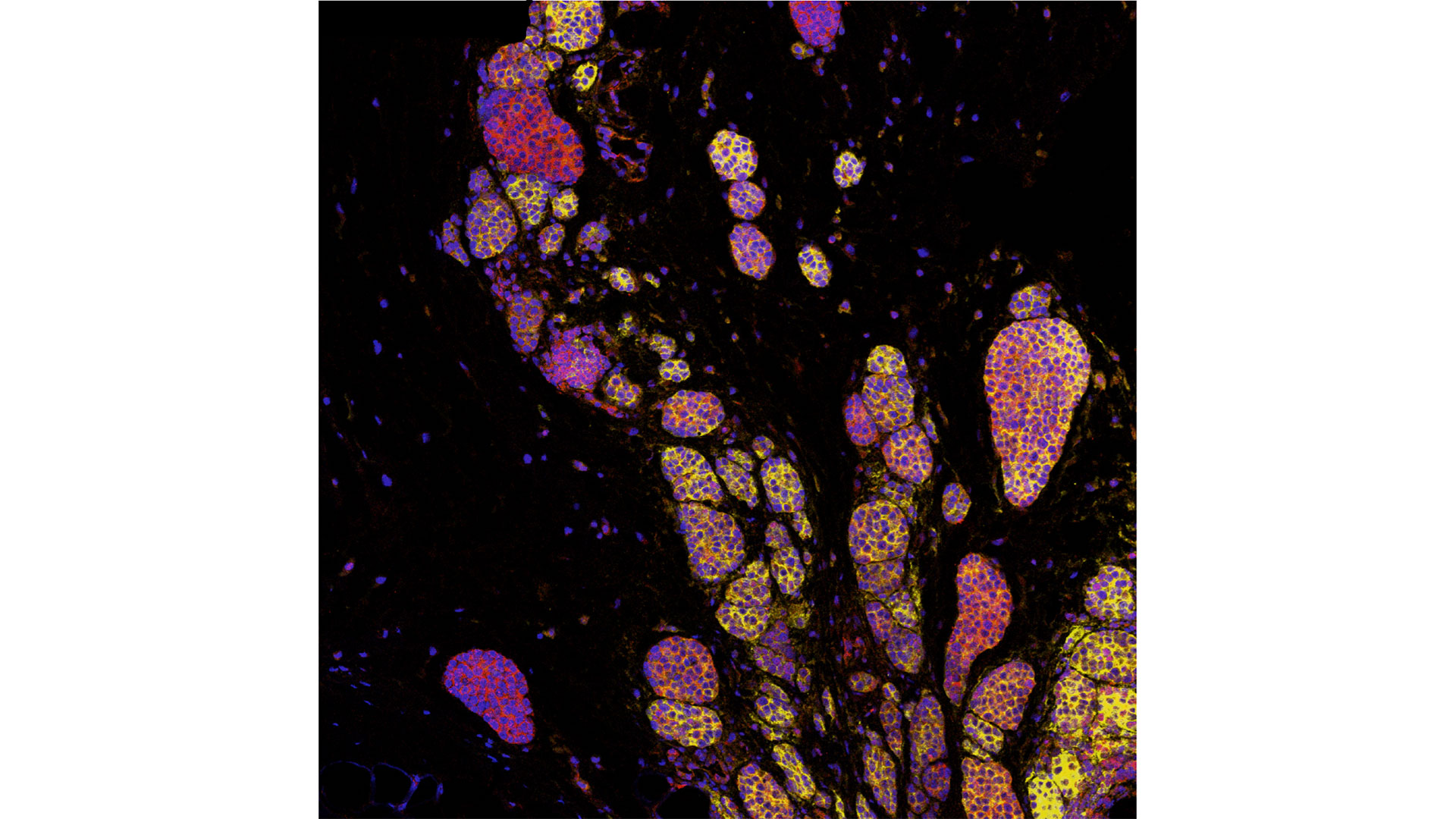
“The connection between the microbiome, the immune system and cancer treatment is a growing field in science,” explains Dr. Saman Maleki, Scientist at Lawson and LHSC’s LRCP, Assistant Professor in Schulich Medicine’s Departments of Oncology, Pathology and Laboratory Medicine, and Medical Biophysics, and senior investigator on the study. “This study aimed to harness microbes to improve outcomes for patients with melanoma.”
The phase I trial included 20 melanoma patients recruited from LHSC, CHUM and JGH. Patients were administered approximately 40 fecal transplant capsules orally during a single session, one week before they started immunotherapy treatment.
The study found that combining fecal transplants with immunotherapy is safe for patients – which is the primary objective of a phase I trial (also called ‘safety trials’). The study also found 65 per cent of patients who retained the donors’ microbiome had a clinical response to the combination treatment. Five patients experienced adverse events sometimes associated with immunotherapy and had their treatment discontinued.
“We have reached a plateau in treating melanoma with immunotherapy, but the microbiome has the potential to be a paradigm shift,” says Dr. Bertrand Routy, Oncologist and Director of CHUM’s Microbiome Center. “This study puts Canada at the forefront of microbiome research by showing we can safely improve patients’ response to immunotherapy through fecal transplants.”
“These exciting results add to a rapidly growing list of publications suggesting that targeting the microbiome may provide a major advance in the use of immunotherapy for our patients with cancer,” adds Dr. Wilson H. Miller Jr. of the JGH and Professor in the Departments of Medicine and Oncology at McGill University.
The study is unique due to its administration of fecal transplants (from healthy donors) in capsule form to cancer patients – a technique pioneered in London by Dr. Michael Silverman, Lawson Scientist, Chair of Infectious Diseases at Schulich Medicine and Medical Director of the Infectious Disease Care Program at St. Joseph’s Health Care London.
“Our group has been doing fecal transplants for 20 years, initially finding success treating C. difficile infections. This has enabled us to refine our methods and provide an exceptionally high rate of the donor microbes surviving in the recipient’s gut with just a single dose,” says Dr. Silverman. “Our data suggests at least some of the success we are seeing in melanoma patients is related to the efficacy of the capsules."
The team has already started a larger phase II trial involving centres in Ontario and Quebec. Lawson researchers are also studying the potential of fecal transplants in the treatment of other cancers, including renal cell carcinoma, pancreatic cancer and lung cancer, as well as HIV and rheumatoid arthritis.
This research is supported in part through donor funding from London Health Sciences Foundation, Western University, the Lotte and John Hecht Memorial Foundation, the JGH Foundation, Canadian Cancer Society’s Impact Grant program and The Terry Fox Foundation.
-30-
ADDITIONAL DOWNLOADABLE MEDIA

About the CRCHUM
The CHUM Research Centre (CRCHUM) is one of North America’s leading hospital research centres. It strives to improve the health of adults through a continuum of research spanning disciplines such as basic science, clinical research and population health. More than 2,150 people work at the CRCHUM, including nearly 500 researchers and nearly 650 students and postdoctoral fellows. crchum.com
About the Jewish General Hospital
Part of the Integrated Health and Social Services University Network for West-Central Montreal (CIUSSS), the Jewish General Hospital has served patients from Montreal, elsewhere in Quebec, and beyond, since 1934. This McGill University teaching hospital, with approximately 600 beds, is one of the province's largest acute-care hospitals. It admits more than 22,000 patients per year, while handling approximately 578,000 outpatient visits, more than 84,000 emergency visits and more than 3,600 births. Treatment is provided by approximately 800 affiliated doctors, many of whom have teaching appointments at McGill University, as well as more than 300 medical residents per year, together with nursing and a wide range of allied health services.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
Fecal transplants show promise in improving melanoma treatment
In a world-first clinical trial published in the journal Nature Medicine, a multi-centre study from Lawson Health Research Institute, the Centre hospitalier de l’Université de Montréal (CHUM) and the Jewish General Hospital (JGH) has found fecal microbiota transplants (FMT) from healthy donors are safe and show promise in improving response to immunotherapy in patients with advanced melanoma.
Immunotherapy drugs stimulate a person’s immune system to attack and destroy cancer. While they can significantly improve survival outcomes in those with melanoma, they are only effective in 40 to 50 per cent of patients. Preliminary research has suggested that the human microbiome – the diverse collection of microbes in our body – may play a role in whether or not a patient responds.
“In this study, we aimed to improve melanoma patients’ response to immunotherapy by improving the health of their microbiome through fecal transplants,” says Dr. John Lenehan, Medical Oncologist at London Health Sciences Centre’s (LHSC) London Regional Cancer Program (LRCP), Associate Scientist at Lawson and Associate Professor in the Department of Oncology at Western University’s Schulich School of Medicine & Dentistry.
A fecal transplant involves collecting stool from a healthy donor, screening and preparing it in a lab, and transplanting it to the patient. The goal is to transplant the donor’s microbiome so that healthy bacteria will prosper in the patient’s gut.
“The connection between the microbiome, the immune system and cancer treatment is a growing field in science,” explains Dr. Saman Maleki, Scientist at Lawson and LHSC’s LRCP, Assistant Professor in Schulich Medicine’s Departments of Oncology, Pathology and Laboratory Medicine, and Medical Biophysics, and senior investigator on the study. “This study aimed to harness microbes to improve outcomes for patients with melanoma.”
The phase I trial included 20 melanoma patients recruited from LHSC, CHUM and Jewish General Hospital. Patients were administered approximately 40 fecal transplant capsules orally during a single session, one week before they started immunotherapy treatment.
The study found that combining fecal transplants with immunotherapy is safe for patients – which is the primary objective of a phase I trial (also called ‘safety trials’). The study also found 65 per cent of patients who retained the donors’ microbiome had a clinical response to the combination treatment. Five patients experienced adverse events sometimes associated with immunotherapy and had their treatment discontinued.
“We have reached a plateau in treating melanoma with immunotherapy, but the microbiome has the potential to be a paradigm shift,” says Dr. Bertrand Routy, Oncologist and Director of CHUM’s Microbiome Center. “This study puts Canada at the forefront of microbiome research by showing we can safely improve patients’ response to immunotherapy through fecal transplants.”
“These exciting results add to a rapidly growing list of publications suggesting that targeting the microbiome may provide a major advance in the use of immunotherapy for our patients with cancer,” adds Dr. Wilson H. Miller Jr. of the JGH and Professor in the Departments of Medicine and Oncology at McGill University.
Previous studies looking at patients receiving immunotherapy who do not respond have found many had an unhealthy microbiome, explains Dr. Lenehan.
“There's a portion of people who don't respond or the treatment just doesn't work,” says Dr. Lenehan. “The hope with the fecal transplant is to make more people respond to treatment.”
These results have also led to a closer examination of the role of the microbiome in regulating how the body responds to disease and how the drugs themselves interact with the microbiome.

“The microbes on and in us - and there's actually a huge amount of those – play a critical role, including modulating some of our immune responses,” explains Dr. Jeremy Burton, Research Chair of Human Microbiome and Probiotics, Scientist at Lawson and St. Joseph’s Health Care London and Associate Professor in the Department of Microbiology and Immunology at Schulich Medicine.
The study is unique due to its administration of fecal transplants (from healthy donors) in capsule form to cancer patients – a technique pioneered in London by Dr. Michael Silverman, Lawson Scientist, Chair of Infectious Diseases at Schulich Medicine and Medical Director of the Infectious Disease Care Program at St. Joseph’s Health Care London.
“Our group has been doing fecal transplants for 20 years, initially finding success treating C. difficile infections. This has enabled us to refine our methods and provide an exceptionally high rate of the donor microbes surviving in the recipient’s gut with just a single dose,” says Dr. Silverman. “Our data suggests at least some of the success we are seeing in melanoma patients is related to the efficacy of the capsules."
The team has already started a larger phase II trial involving centres in Ontario and Quebec. Lawson researchers are also studying the potential of fecal transplants in the treatment of other cancers, including renal cell carcinoma, pancreatic cancer and lung cancer, as well as HIV and rheumatoid arthritis.
This work is not possible without poop donors, and there is a critical need for more. Donors must be between the ages of 18 to 50 and reside in the London, Ont. area. To learn more about eligibility and donating, call the 519 646-6100, ext. 61726 or email Dr. Seema Nair Parvathy, Research Scientist, at SeemaNair.Parvathy@sjhc.london.on.ca.
This research is supported in part through donor funding from London Health Sciences Foundation, Western University, the Lotte and John Hecht Memorial Foundation, the JGH Foundation, Canadian Cancer Society’s Impact Grant program and The Terry Fox Foundation.