Search
Search
Addressing the impacts of the COVID-19 pandemic
As the COVID-19 pandemic has continued for a year and a half, many people from all walks of life are feeling the impacts especially when it comes to their mental health and wellbeing.
Hospital researchers through Lawson Health Research Institute, along with its hospital partners, have been studying the impacts for some key groups.
Health care workers have been at the forefront of the pandemic. These heroes have worked tirelessly through every wave and continue to provide excellent care to their patients and community. Dr. Kamia Honarmand, Critical Care Physician at London Health Sciences Centre (LHSC), remembers the stress that she and her colleagues were feeling, and know that something needed to be done.
“Our team wanted to better understand the impact of the pandemic on the lives of health care workers, both personally and professionally, and understand how they were coping when it came to their mental health,” says Dr. Honarmand who is also an Associate Scientist at Lawson. “There was a lot of reasons to be stressed even before the height of the first wave in our region. There was a lot of anxiety. The hospital wanted to find ways to support health care workers and identify resources that would assist them.”

Dr. Kamia Honarmand, Critical Care Physcian at LHSC and Lawson Associate Scientist
Frontline health care workers across the region were invited to take part in an online survey about their experiences during the pandemic. “We looked at both the impacts and the preferred coping strategies, and what supportive strategies they would like to have in the hospital in the future.”
The Veterans Care Program located at Parkwood Institute, a part of St. Joseph’s Health Care London, provides complex continuing and long-term care for Canadian war Veterans. Dr. Don Richardson, Director of the MacDonald Franklin OSI Research Centre at Parkwood Institute, has been treating and studying mental health among Veterans for many years. He believed this was a group was likely to be affected by the pandemic in unique ways.
“We know that Veterans in general are at a higher risk for depression, anxiety and PTSD,” explains Dr. Richardson, who is also a Scientist at Lawson. “We also knew the pandemic and forced restrictions would have significant impact on Veterans and their families who would be more isolated than they already are.”
More than 1,100 Veterans and around 250 spouses were recruited for the study, completing an online survey every three months for 18 months.
The study is still ongoing, but Dr. Richardson says the initial data has been telling. “We have been able to analyze some of the preliminary data and what we have found is that almost 50 per cent did not indicate their mental health had worsened during the pandemic but 40 to 50 per cent have had difficulty accessing care.”

Dr. Don Richardson, Director, Macdonald Franklin OSI Research Centre
The hope is that this study will lead to better preparedness in the future to safeguard the mental health of Veterans and ensure their access to care during a pandemic.
Many people have felt isolation during the pandemic, but that feeling may have even more of an impact for youth suffering from mood and anxiety disorders.
Dr. Elizabeth Osuch, Director of the First Episode Mood and Anxiety Program (FEMAP) at LHSC says the pandemic-led lockdown forced more than a hundred mental health clients out of in-person services.

Dr. Elizabeth Osuch, Director of FEMAP and Lawson Scientist
“They lost their resources for mental health services and support as soon as the quarantine was announced,” shares Dr. Osuch, who is also a Scientist at Lawson. “We were concerned that it would be devastating to people – and to some people it was. We wanted to make sure they had an avenue to connect with the program.”
Dr. Osuch and the FEMAP team created an online research platform to find out how patients were doing by having them fill out a symptoms and function questionnaire.
“We have analyzed the first wave so far and it shows that male patients were doing better and female patients were doing worse, which was a surprise. One of the risk factors for not doing well was the loss of their job.”
The pandemic added an extra layer of stress and worry for women who were having a baby.
“This has been an enormous and pivotal time for everyone in the world,” says Dr. Genevieve Eastabrook, Obstetrician-Gynecologist at LHSC. “The experiences during pregnancy and post-partum for both the birthing person and their baby can have effects later in life for children. For example, their overall cardiovascular and metabolic health, bonding experiences and the risk of mood disorders.”
Dr. Eastabrook, who is also an Associate Scientist at Lawson and Assistant Professor at Western University’s Schulich School of Medicine & Dentistry, is working with a team to examine the effects the pandemic may be having for mothers and their babies. As part of the study, the London research team is using an approach called ‘One Health’ which offers a holistic perspective to explore how various risk factors and social determinants of health interact.

Dr. Genevieve Eastabrook, OBGYN at LHSC and Lawson Associate Scientist
“The unique aspect is that we have a comparative group to see if there are differences in markers such as risk of depression, perceived stress and social supports,” adds Dr. Eastabrook.
Study participants are asked to complete a 30-minute questionnaire at around 6-12 weeks after their delivery. The research team is still recruiting patients for this study.
Advancing Hospital Based Clinical Research Conference
When: Thursday October 19th, 2023 9am – 4pm (check in starts at 8am)
Where: Parkwood Institute Auditorium B2 - 109
Agenda: Dr. David Hill – Opening Remarks
Speakers include:
- Dr. Naveen Poonai (Chair HSREB)
- Dr. Steve Smith (Ontario Hospital Association, Research and Innovation Committee)
- Mr. Jonathan Mitchell, HealthCareCan, Vice President, Research and Policy
- Mr. Reza Salehzadeh-Asl and Ms. Shila Rastegar (Health Canada, Clinical Trial Inspectorate Program)
Earn 5.0 CEUs * Conference fee is $50 for LHSC, St. Joseph’s Health Care London, Lawson and Western affiliates (Non-Affiliates $150). *Breakfast and lunch included.
Spaces are Limited *You must register before October 15th*
Click to REGISTER TODAY (use your institutional email - LHSC, SJHC, Lawson, UWO, Schulich, etc.).
For more information or questions contact Lawson at @email or @email.
Advancing research during the COVID-19 pandemic
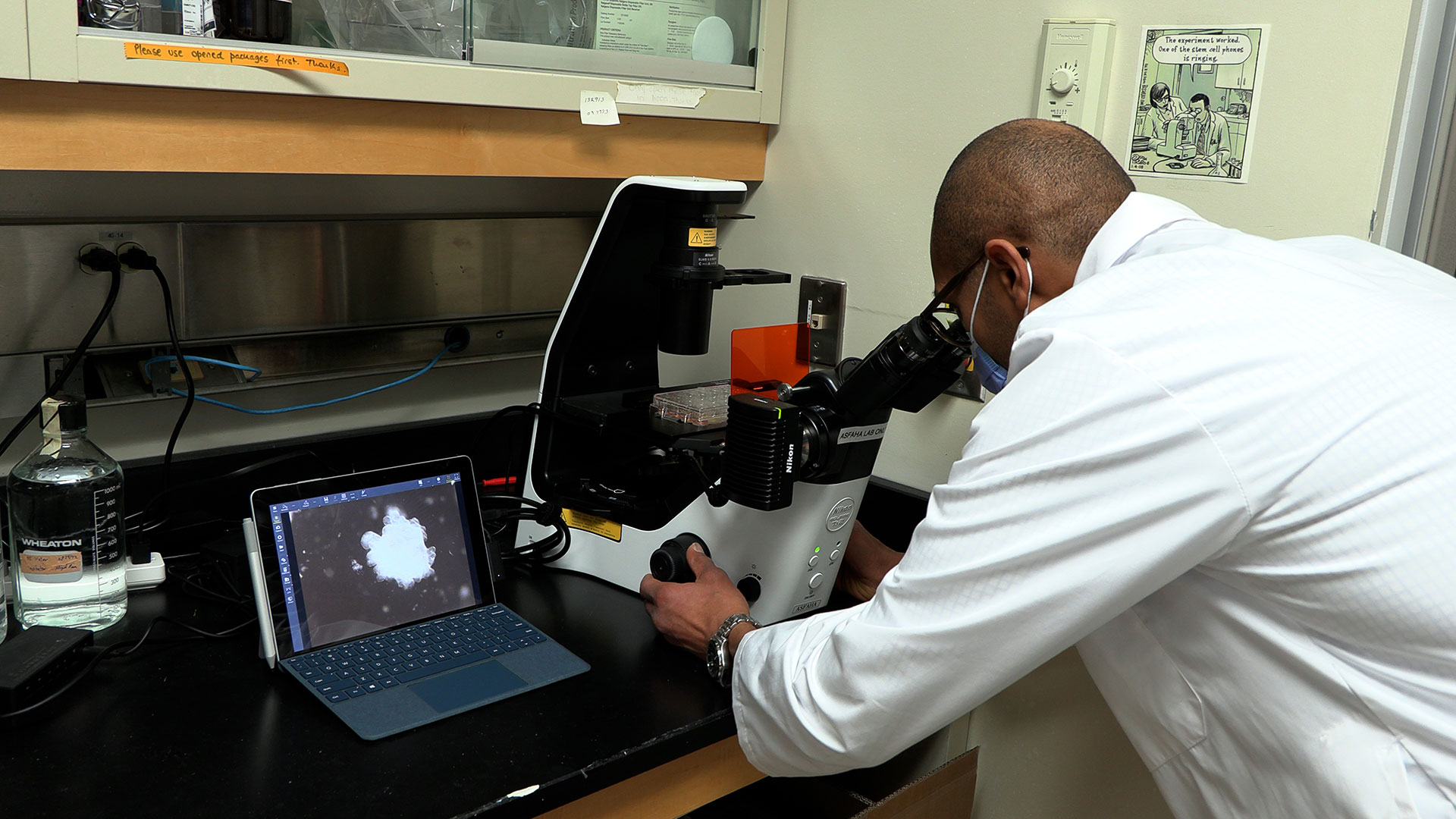
From the moment the COVID-19 pandemic was declared in March 2020, our teams at Lawson Health Research Institute have been at the forefront. Researchers at London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London immediately began to work towards understanding the new virus in an effort to discover lifesaving health-care solutions.
To date, dozens of research projects have been advanced through Lawson with some receiving international attention as ‘world firsts’. As we mark the three-year anniversary of COVID-19 being declared a global pandemic by the World Health Organization (WHO), we share with you COVID-19 research highlighted over the past year.
Study finds acute kidney injury associated with severe COVID-19 leads to high mortality rates

Severe cases of a COVID-19 infection can cause a host of serious complications, including acute kidney injury. In a published study, scientists at Lawson found that acute kidney injury in patients with a severe COVID-19 infection leads to a high mortality rate.
By accessing data collected through the Ontario Renal Network (ORN), Dr. Peter Blake, Lawson Researcher and Provincial Medical Director at the Ontario Renal Network, and his colleagues examined 271 people at 27 renal programs across the province, including patients at LHSC, who received dialysis for acute kidney injury due to a COVID-19 infection. Read more.
Study shows a decline in Veterans’ mental health throughout the pandemic

In published findings from Lawson, more than half of Canadian Veterans reported a decline in their mental health over the course of the COVID-19 pandemic.
When it comes to mental health conditions, Veterans are an at-risk population, often having higher rates of depression and post-traumatic stress disorder (PTSD). When the COVID-19 pandemic hit, scientists at Lawson wanted to understand its effects on this already at-risk population.
To examine the potential impacts the research team launched a longitudinal study recruiting Canadian Veterans and spouses of Canadian Veterans. Participants complete online questionnaires every three months, with questions focused on mental health and virtual health care services. Read more.
Virtual care associated with significant environmental and patient cost savings

A study published in JAMA Network Open by researchers at ICES, Lawson and Western University found that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs.
Findings show that for more than 10 million patients with at least one appointment during the study period (63 million visits in total), virtual care was associated with estimated savings of:
• 3.2 billion kilometers of patient travel;
• 545 to 658 million kilograms of carbon dioxide (CO2) emissions; and
• $569 to $733 million (Canadian [US $465-$599 million]) in expenses for gasoline, parking, or public transit. Read more.
London researchers discover novel method to diagnose long COVID

Published in Molecular Medicine, researchers at Lawson found that patients with post-COVID-19 condition (long COVID) have unique biomarkers in their blood. The team is now working on developing a first of its kind blood test that could be used to diagnose long COVID. The discovery could also lead to new therapeutics for this condition.
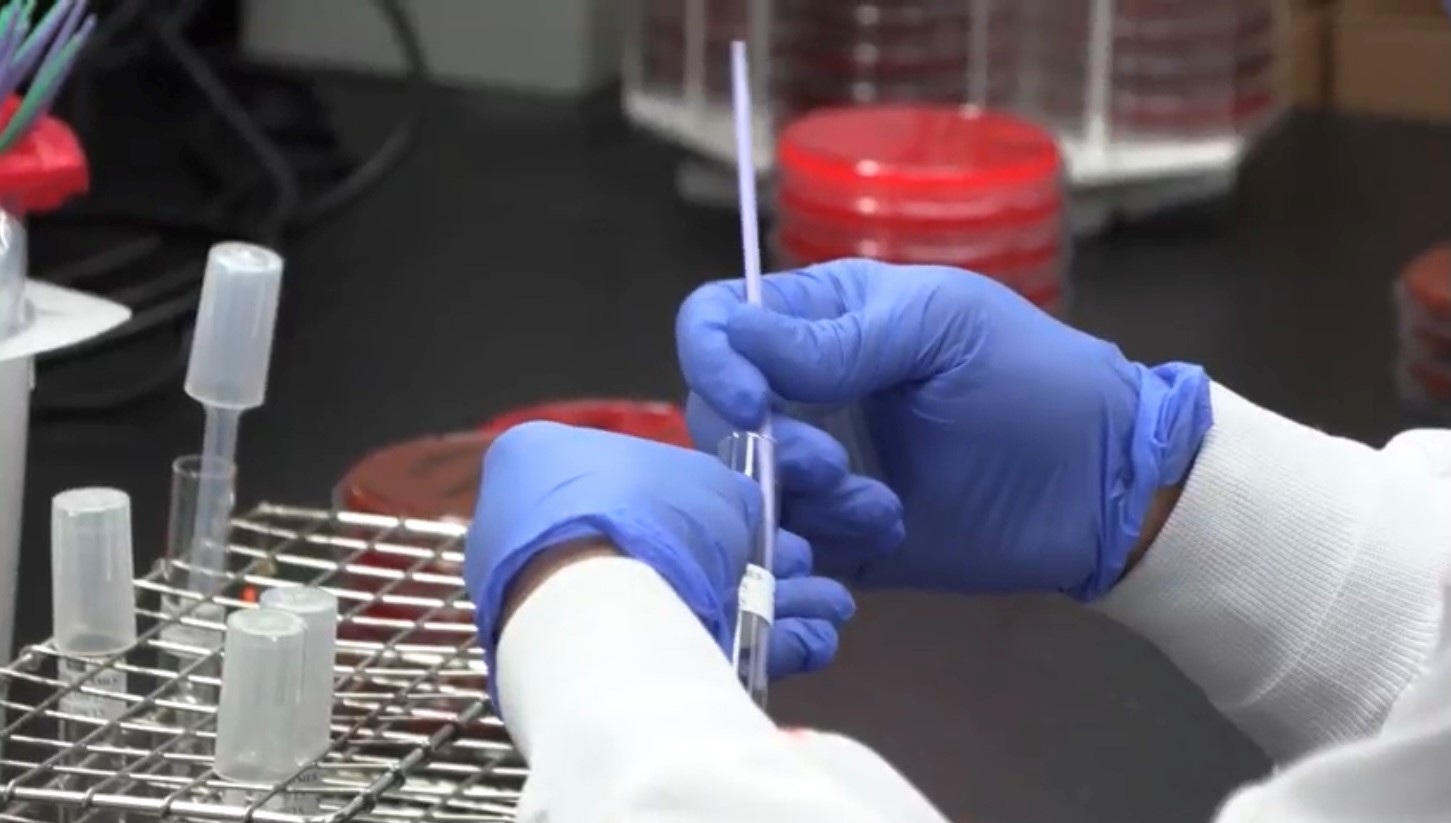
The researchers studied 140 blood samples from participants at LHSC and St. Joseph’s Health Care London, including St. Joseph’s Post-Acute COVID-19 Program. Participants were those with presumed long COVID, hospital inpatients with acute COVID-19 infection and healthy control subjects. Read more.
Researchers are combining new technologies to examine blood proteins in COVID-19 patients
Published in the Journal of Cellular and Molecular Medicine, a team at Lawson discovered unique patterns of blood plasma proteins in critically ill patients that may help develop a more personalized approach to treating severe COVID-19.
Called the plasma proteome, the proteins studied are released by cells that often play an important role in the body’s immune response to viruses. The research team studied how they adapt and change to a COVID-19 infection. Read more.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Advancing research on haemochromatosis
Thanks to decades of work by dedicated researchers like London, Ont.-based Dr. Paul Adams, haemochromatosis has become much easier to diagnose, though many people are still unaware of the genetic condition. And while treatment options are effective, they are limited, according to a new review published in The Lancet.
In Canada and the United States, one in 227 people have haemochromatosis, making it more common than cystic fibrosis. However, the U.K. Biobank Project, a large-scale biomedical database and research resource, found that only 12 per cent of people who have the condition actually know they have it.
Dr. Adams, a Scientist at Lawson Health Research Institute and Professor at Western University’s Schulich School of Medicine & Dentistry, explains, “The most common genetic test done in Canada and the U.S. is the best way to make the diagnosis, but you have to think of the condition and the doctor has to know that there is a genetic test available. So those two steps are some of our stumbling blocks.”
In Ontario, testing and diagnosis often comes only after some other issue arises, “One day someone stumbles on the fact that there's a liver abnormality, or the patient is complaining of fatigue and the doctor orders blood tests, thinking blood iron is going to be low,” Dr. Adams explains. “And then it turns out to be very high.”
Most common in people of Northern European ancestry, haemochromatosis results in excess iron in the body and includes symptoms such as fatigue and arthritis pain, and can lead to serious complications like cirrhosis of the liver, liver cancer and death.

Starting in January 2000, Dr. Adams conducted a multi-year study involving 20,000 London, Ont. residents that helped change how haemochromatosis is diagnosed – moving from testing iron levels to genetic testing. With iron levels affected by alcohol consumption, obesity, inflammation and some types of cancer, the previous measure led to many false positive tests.
But knowing when genetic testing should be done remains a challenge. The underdiagnosis and lack of awareness also remain an issue when it comes to more serious complications.
“If this is diagnosed early, like as a young adult, then this can be treated and those complications won’t develop,” Dr. Adams says. “If you donate blood, treatment is very similar to that procedure and it's tolerated extremely well in most. People who have a lot of excess iron will have this blood taken once a week until their iron levels come down.”
He hopes this new publication will lead to better diagnosis and treatment, and sees a future in emerging biological therapies.
Dr. Adams continues to be involved in global research, including work with the U.K. Biobank Project on genomic testing, and is investigating partnerships to develop future gene editing treatment.
People looking for more information about haemochromatosis can reach learn more on the Canadian Haemochromatosis Society’s website.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
Advocating for health research during “H on the Hill”
HealthCareCAN held its third annual Lobby Day “H on the Hill” event on Parliament Hill in Ottawa, on Tuesday, October 30, 2018.
Canada’s hospital CEOs and vice presidents of health research joined HealthCareCAN - the national voice of Canada’s healthcare organizations, community and research hospitals - to meet with MPs, Senators and senior government staff.
Collectively, they issued a call for federal action to unlock the tremendous economic potential of the health and life sciences sector to support better health for Canadians.
Dr. David Hill, Scientific Director for Lawson and Integrated Vice President of Research for London Health Sciences Centre and St. Joseph’s Health Care London, participated in the lobby day. Dr. Hill currently sits on the Board of Directors for HealthCareCAN.

Image

“Minister of Crown Indigenous Relations @Carolyn_Bennett, Parliamentary Secretary for Science, Sport, and Accessibility @KateYoungMP, and Dr. David Hill, catching up over lunch at #HontheHill #CDNpoli #CDNhealth”
Meeting participants stressed the need for action on HealthCareCAN’s recommendations for the 2019 federal budget, specifically:
- Setting a minimum 25% funding floor for the indirect costs of research under the Research Support Fund;
- Granting eligibility to federal infrastructure funding competitions to healthcare organizations, and;
- Investing in digital health platforms to support care, training, and research in healthcare organizations.
Diverse areas of the health and life sciences sector and key health issues were discussed, including:
- Health and science research, granting councils;
- Hospital infrastructure;
- Health innovation;
- Electronic health technology;
- Opioid crisis response;
- Mental health;
- Aboriginal health; and,
- Home care.
Read Dr. Hill’s recent column in Hospital News on bridging the gap from discovery to patient care.

HealthCareCAN provides high-quality policy research advocacy and leadership development services to our members while championing healthcare system transformation in Canada. Visit www.healthcarecan.ca to learn about our solutions to health and healthcare challenges. Follow us on Twitter: @HealthCareCAN
Ali Bateman
Ali Bateman, MD
Assistant Professor, Schulich School of Medicine and Dentistry
Acquired and Traumatic Brain Injury; Spinal Cord Injury
Dr. Ali Bateman is a physiatrist at Parkwood Institute and an Assistant Professor in the Department of Physical Medicine and Rehabilitation Schulich School of Medicine & Dentistry at Western University. She is also an Associate Scientist at Lawson Health Research Institute, and the Quality Improvement Lead in the Department of Physical Medicine & Rehabilitation.
Dr. Bateman completed her medical degree and residency training at Western University, and is currently completing a master’s degree in Quality Improvement and Patient Safety through the Institute of Health Policy, Management, and Evaluation at the University of Toronto. She is also certified by the Canadian Society of Clinical Neurophysiologists and holds the designation of CSCN Diplomate (EMG). As a consultant physiatrist, Dr. Bateman provides care in acquired brain injury and spinal cord injury rehabilitation programs and the electrodiagnostic laboratory at Parkwood Institute.
Her research interests centre on quality improvement, patient safety, and knowledge translation with the aim of achieving best practices so that all persons with spinal cord and/or brain injury receive the best quality care.

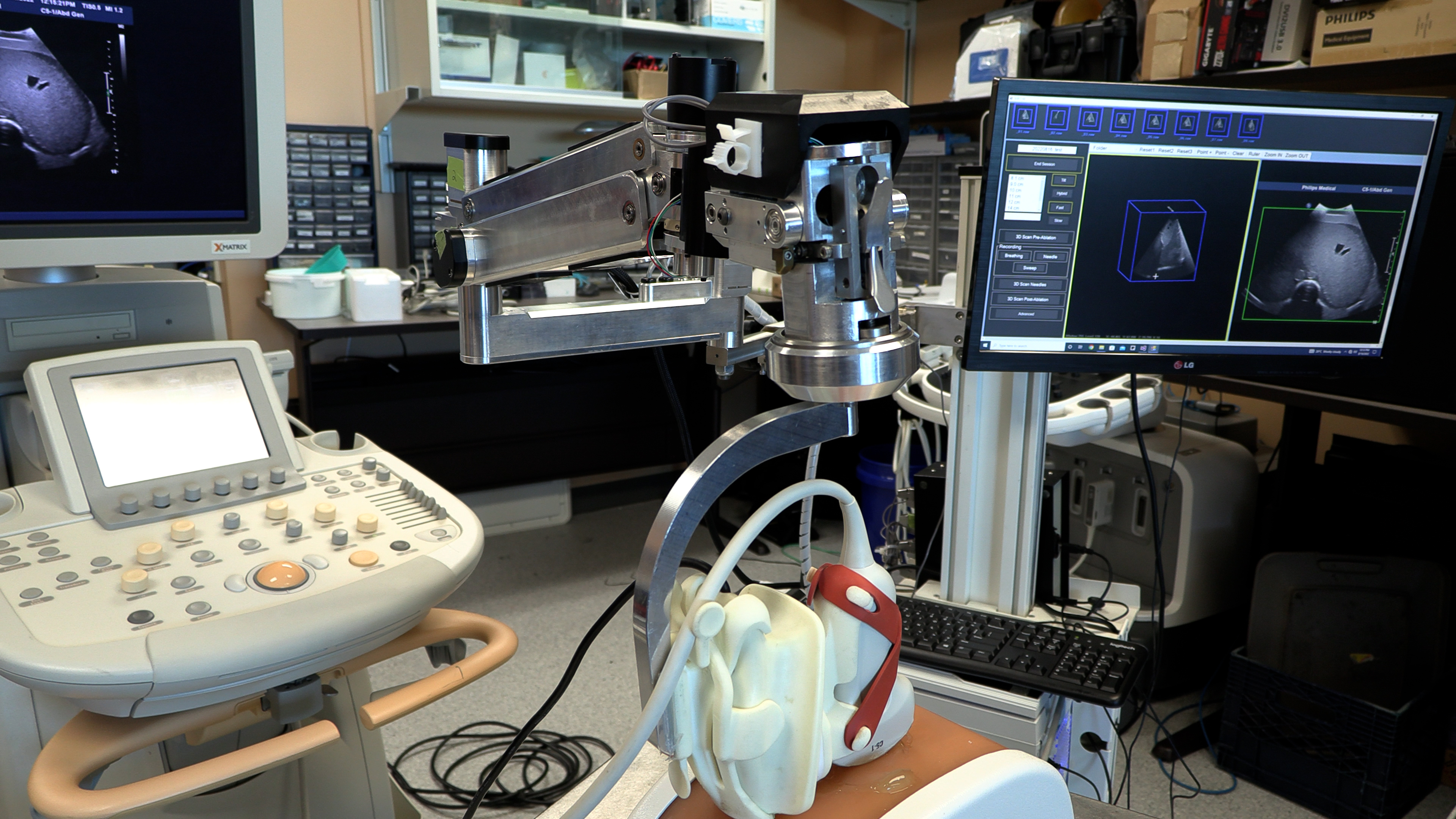
An image of the future: Innovations in imaging research
Lawson Health Research Institute (Lawson) has long been a leader in biomedical imaging. The first Canadian magnetic resonance imaging (MRI) of a human occurred at St. Joseph’s Health Care London (St. Joseph’s). The country’s first positron emission tomography/computed tomography (PET/CT) and positron emission tomography/magnetic resonance imaging (PET/MRI) scanners were also installed at St. Joseph’s. New developments in imaging research continue to enhance the diagnosis, prevention and treatment of a wide range of diseases, from cancer to post-traumatic stress disorder.
On May 23, Lawson hosted a Café Scientifique event where a panel of Lawson Imaging scientists discussed their cutting-edge work. Guests had the opportunity to ask questions as part of an open-forum discussion to gain insights from the speakers, and from one another.
In celebration of Canada’s 150th anniversary as a nation, this event is the first of a two-part series focusing on the future vision for health care in Canada and the legacy that research at Lawson will leave.
Imaging of the heart: Seeing the cause of chest pain more clearly
By Dr. Ting-Yim Lee, Lawson scientist, Medical Physicist at St. Joseph’s, professor at Western University’s Schulich School of Medicine & Dentistry, and scientist at Robarts Research Institute
When patients with chest pain arrive in the emergency department, they are given an electrocardiogram (ECG) and blood test. These diagnostic tests determine if the pain has a non-cardiac cause (such as heart burn), if it is caused by a heart attack, or if the patient has angina (plaque formation in the coronary arteries that either reduces or temporarily cuts off blood flow to the heart) but did not have a heart attack.
If a patient has angina, they are then given additional diagnostic testing to see whether a blood clot has formed and where it is located. This is determined by two different imaging techniques: x-ray imaging (angiogram) and nuclear imaging. This process is invasive and means that patients must be scheduled for two different exam days. Using two techniques also means that there can be image misalignment, and the images often provide poor detail.
Dr. Ting-Yim Lee’s lab has pioneered a Computed Tomography (CT) method for imaging blood flow to the heart muscle (CT Perfusion), which can help patients avoid unnecessary tests and treatment, as well as reduce health care costs.
“CT imaging is a non-invasive imaging technique that uses x-rays to create high-detail cross-sectional images of the body. Using this method, we can evaluate the degree of blockage in coronary arteries – with one diagnostic test instead of two,” says Dr. Lee.
Using light and sound to improve breast surgery
By Dr. Jeffrey Carson, Lawson scientist and associate professor at Western University’s Schulich School of Medicine & Dentistry
“Most women diagnosed with breast cancer undergo surgery, and months of chemotherapy and radiotherapy. They must deal with the discomfort, side-effects, emotional stress and financial burden of treatment. Almost one in four surgeries for breast cancer must be repeated, meaning many women have to go through this all over again,” says Dr. Jeffrey Carson.
In breast conserving surgery, there is a high chance of repeat surgery as the surgeon must see and remove 100 per cent of the tumour in order for it to be successful. They are not able to determine whether the entire tumour was removed until after the surgery has been completed.
Dr. Carson and his team at St. Joseph’s have developed a technology called Intraoperative Photoacoustic Tomography (iPAT), which has the potential to reduce the chance of repeat surgery for breast cancer. The technology is able to image surgery specimens in the operating room during surgery, allowing surgeons to determine whether the whole tumour has been removed before the surgery is complete.
How imaging can improve the management of epilepsy
By Dr. Udunna Anazodo, postdoctoral fellow at Lawson
Most patients with epilepsy are effectively treated with antiepileptic drugs. However, 36 per cent will not respond to the drugs. For these patients, surgery on the area of the brain that is causing seizures is the standard of care – if patients are good surgical candidates.
“If patients with epilepsy are to undergo surgery there must be a good indication of where the seizure focus is and it must be possible to determine that removing this portion of the brain will not affect brain function,” says Dr. Udunna Anazodo.
To see whether they are good candidates for surgery, patients must undergo an invasive procedure called intracranial monitoring, where electrodes are placed on the brain.
Dr. Anazodo has been studying how PET/MRI can be used to map seizures with the goal of minimizing the need for invasive intracranial monitoring. This technique makes it possible to locate areas in the brain that cause seizures and to see if the seizures affect brain functions.
See photos from the event on Lawson’s Facebook page.

Above: Café Scientifique presenters (from left to right): Drs. Jeffrey Carson, Frank Prato (moderator), Ting-Yim Lee and Udunna Anazodo.
An image of the future: Innovations in imaging research
Lawson Health Research Institute has long been a leader in biomedical imaging. The first MRI images in Canada were captured at St. Joseph’s Hospital and we were the first in the country to install PET/CT and PET/MRI scanners. New developments in imaging research continue to enhance the diagnosis, prevention and treatment of a wide range of diseases, from cancer to PTSD.
You are invited to Lawson’s Café Scientifique, a free community event providing an informal opportunity to get involved with science. Hear a panel of Lawson Imaging scientists discuss their cutting-edge work and have the opportunity ask questions as part of an open-forum discussion to gain insights from the speakers, and from one another.
In celebration of Canada’s 150th anniversary as a nation, this event is the first of a two-part series focusing on the future vision for health care in our country and the legacy our research will leave.
Presented Talks
- “Imaging of the heart: Seeing the cause of chest pain more clearly”
Dr. Ting-Yim Lee - “Using light and sound to improve breast surgery”
Dr. Jeff Carson - “How imaging can improve the management of epilepsy”
Dr. Udunna Anazodo - MODERATOR – Dr. Frank Prato
Registration
To register, please complete our registration form. To sign up to our email list for notification of future events, please email @email.
Event Information
Date: Tuesday, May 23, 2017
Time: 7 to 9 p.m.
Location: Mercato at Brescia University College, Clare Hall, 271 Ramsay Road, London ON, N6G 0S2
An innovative year: Top 12 research stories of 2023
It’s been another year of transformational research at Lawson Health Research Institute. Our teams have published groundbreaking findings and launched new studies that will have a profound impact on patient care.
The following are 12 highlights of research and innovation from across London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London (St. Joseph’s). From trialing new cancer treatments to advancing understanding of mental health, our research teams have achieved a number of important milestones.

1. New study suggests blood plasma proteins hold answers to better understanding long COVID
Lawson researchers continued to advance understanding of COVID-19 this past year. In one study, researchers found that unique patterns in blood plasma proteins of patients with suspected long COVID could act as a drug target to improve patient outcomes. Read more.

2. New study finds exercise, cognitive training combo boosts mental sharpness in seniors
A study from Lawson and Western University found that a combination of computerized cognitive training and aerobic-resistance exercises can improve functions like memory, attention, recognition and orientation in older adults with mild cognitive impairment. The results suggest a new way to address declining mental sharpness in older adults. Read more.

3. $7.55 million in funding to take LHSC-developed technology global
Technology to diagnose rare genetic disorders developed by researchers at Lawson and LHSC will be going global thanks to $7.55 million in funding from Genome Canada grant and Illumina Inc. The new artificial intelligence-led technology could allow rare diseases to be diagnosed with a simple blood test. Read more.
4. Fecal transplants show promise in improving melanoma treatment
Fecal microbiota transplants (FMT) from healthy donors are safe and could improve response to immunotherapy in patients with advanced melanoma, according to results from a world-first multi-centre clinical trial led by Lawson researchers. Read more.

5. New study shows technology could play an important role in mental health support
A team of Lawson researchers found that the use of ‘smart home’ technology like touch screen devices, activity trackers, weigh scales and medication dispensers may lead to better outcomes for those living with both mental health and physical disorders. The study found that participants using the technology started logging more exercise, making healthier food choices and not missing medication doses. Read more.

6. Canadian children’s hospital visits for suicidal thoughts, self-poisoning and self-harm up during pandemic, study finds
A national study with Lawson researchers found that during the first two years of the COVID-19 pandemic, adolescent emergency department (ED) visits and hospitalizations for suicidal thoughts, self-harm and self-poisoning increased across Canada, with the greatest increase occurring among adolescent girls. Read more.

7. St. Joseph’s to become Canada’s first centre of excellence in molecular imaging and theranostics
A partnership between Lawson, St. Joseph’s Health Care London and GE HealthCare will create Canada’s first centre of excellence in molecular imaging and theranostics at St. Joseph’s. The centre will focus on using precision diagnostic imaging and targeted therapy to advance personalized treatment of cancer and other diseases. Read more.

8. Researchers investigate a new method of sedation for paediatric patients
Intravenous sedatives are normally used to sedate critically ill children. However, they can contribute to a complication called delirium, which includes symptoms of confusion, disorientation, agitation, excessive drowsiness and poor attention. To improve outcomes, scientists at Children’s Health Research Institute (a program of Lawson), Sunnybrook Research Institute and The Hospital for Sick Children (SickKids) are collaborating on a pilot study to understand whether inhaled sedation could be a better alternative to keep critically ill children sedated and comfortable. Read more.
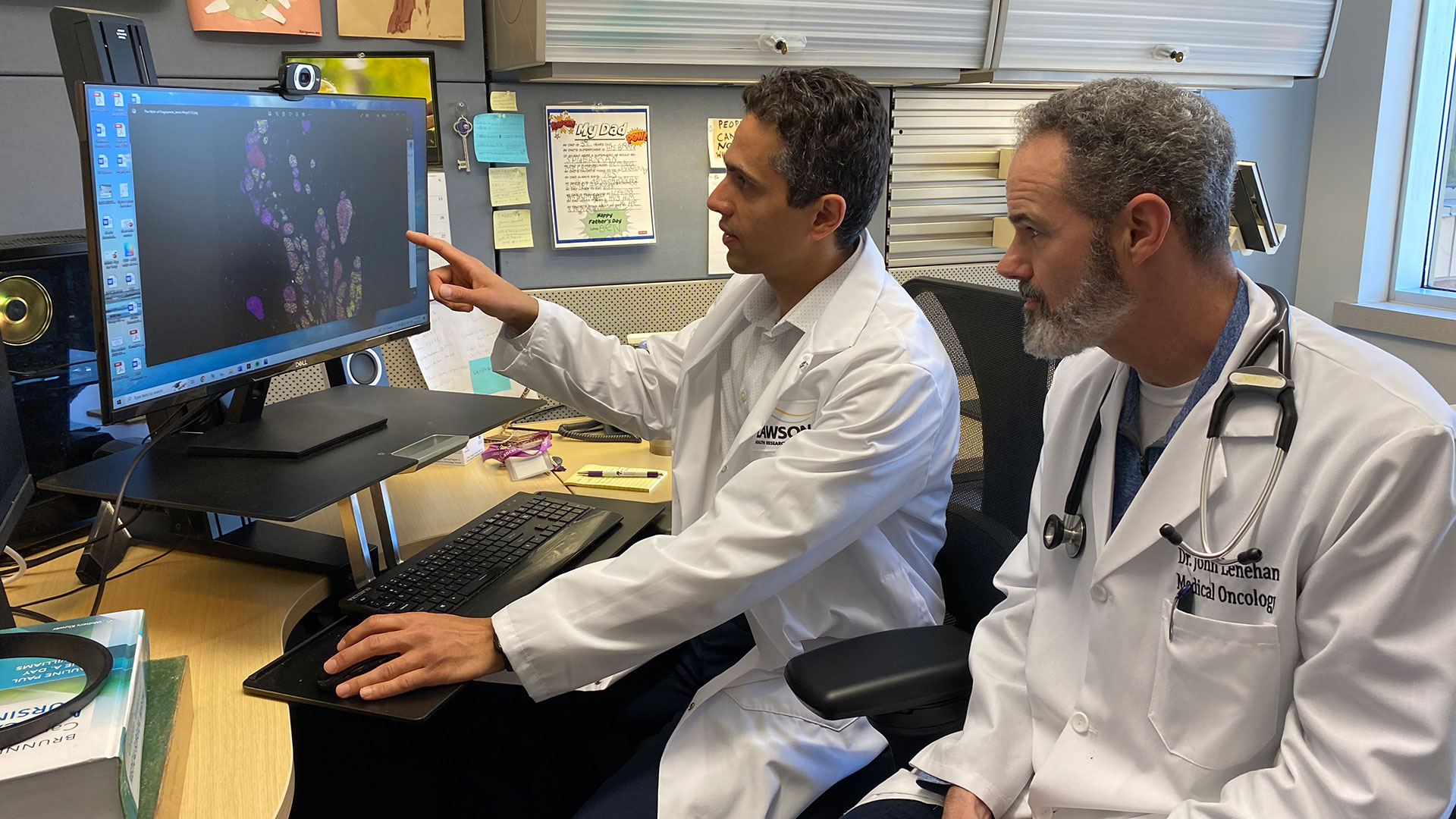
9. New robotic 3D ultrasound may improve accuracy of liver cancer ablation therapy
A technique that turns a normal ultrasound into a 3D image is showing promise in making thermal ablation for liver cancer treatment more accurate in a study from Lawson and Western University. Thermal ablation – using heat to destroy a cancerous tumour – can have fewer complications and a shorter recovery time than surgery. Read more.

10. Assessing neurofeedback in stroke survivors
Functional near-infrared spectroscopy (fNIRS) is used to detect changes in brain oxygen levels using light, but more recently it has also been used to develop brain-computer interfaces – allowing patients with brain injuries to control a device with their thoughts. Researchers at Lawson launched a new study to assess whether fNIRS can be used to improve patient outcomes during stroke rehabilitation. Read more.
11. Specific type of inflammation may be linked to risk of colorectal cancer
A preclinical study found that a specific type of inflammation may be linked to an increased risk of colorectal cancer. Previously, the degree of inflammation caused by illnesses like colitis, Crohn’s disease and other forms of inflammatory bowel disease were shown to be an important indicator of the development of colorectal cancer. However, this new study found the type of inflammation, rather than the severity and duration, may be more important in determining cancer risk. Read more.

12. New study examining if probiotics can improve outcomes in knee replacement surgeries
Lawson researchers launched a study to assess whether daily probiotics can improve outcomes in patients undergoing a total knee replacement surgery. Of the more than 70,000 knee replacement surgeries in Canada each year, nearly 10 per cent of patients experience complications. With patients who are considered healthy likely to have better outcomes, the research team is interested in improving the gut microbiome as a way to support patients’ overall health. Read more.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
An online approach to care
With an aging population, neurological conditions like stroke, brain injury and multiple sclerosis (MS) are on the rise in Canada. Those living with neurological conditions face many long-term challenges that can affect both their physical and cognitive functioning. They are also at an increased risk for mental health challenges such as depression and anxiety.
“While mental health challenges are common for those with neurological conditions, they often go untreated for a number of reasons,” says Dr. Swati Mehta, Scientist at Lawson Health Research Institute. “For example, those living in remote areas often do not have access to specialized services and many patients are concerned about stigma.”
Yet seeking mental health care is critically important for patients with neurological conditions. “Research suggests that depression among these patients can impair recovery, leading to decreased quality of life and increased health care costs.”
To improve patient outcomes, Dr. Mehta and a collaborative research team are developing an internet-delivered cognitive behavioural therapy (ICBT) program.

Cognitive behavioural therapy (CBT) is a specialized type of therapy that involves patients learning strategies and skills to self-manage mental health symptoms. It’s one of the most widely used therapies for the treatment of depression and anxiety.
A panel of researchers, persons with lived experience of neurological conditions and community organizations are working collaboratively to develop an accessible ICBT program that meets the needs of persons with neurological conditions and mild cognitive impairment who are also experiencing symptoms of depression or anxiety. The program, called The Neuro Course, will be a modified version of an existing course developed in Australia by the eCentreClinic.
“Through co-development with patients and experts in the field, the ICBT program will meet the specific needs of persons with neurological conditions who are also experiencing mental health challenges,” explains Dr. Mehta. “With online delivery, it can provide personalized treatment while being flexible and easily accessible.”
The Neuro Course will be piloted with a small group of research participants, including patients from Parkwood Institute, a part of St. Joseph’s Health Care London. Eligible participants can sign up to be notified of the course’s availability at https://www.onlinetherapyuser.ca/neuro.
The free online course consists of six easy-to-understand CBT lessons and will take approximately 10 weeks to complete. In addition to the six lessons, participants will be encouraged to work through various activities during the week.
Participants will also receive regular support from a designated online guide. Guides will be health educators who are certified providers or graduate students working under the supervision of certified providers. All guides will have training in psychology or social work. The participant’s guide will review the participant’s progress and answer any questions or comments through a secure messaging system.
Participants in the study will be asked to complete brief questionnaires before they begin the course, on a weekly basis throughout the course and then again three months after treatment ends. The research team will use the questionnaires to assess patient outcomes and improve future versions of the course.
The goal of the program is to overcome barriers to face-to-face therapy, such as limited access to specialized care and concerns about stigma related to seeking care, by providing an effective online alternative. By reaching those in need, the research team hopes to improve patient outcomes and overall wellbeing.
“The long term goal would be to implement the ICBT program into clinical practice to provide increased access to mental health services among this population,” says Dr. Mehta. “The program could be used to provide care to those with mild to moderate mental health concerns or those waiting to access face-to-face programs.”
The team is being funded for this project through Lawson’s Internal Research Fund (IRF) competition. “As an early career researcher, receiving funding from Lawson’s IRF is a great honour. It’s a great opportunity to help researchers obtain funding for small feasibility studies to develop evidence for larger grants that can be used to translate knowledge across the community,” states Dr. Mehta.
Annual London Imaging Discovery Conference
London Imaging Discovery Day was launched in 2006 as a platform for scientists and residents in radiology and nuclear medicine to share their research with mentors, peers, graduate students, and others. This conference, coordinated by the Department of Medical Imaging at the Schulich School of Medicine & Dentistry, was another brilliant idea conceived by Dr. Aaron Fenster, Director of Imaging Sciences and Dr. Andrea Lum, Chair of Medical Imaging and City-Wide Chief of the Department of Diagnostic Radiology.
The LID conference focuses on Functional, Morphological and Molecular Imaging and targets London’s current and future leaders in Imaging Research, to meet and share their most advanced discoveries. London is a major, leading center for the medical industry and over the past 10 years, the LID conference has grown and now attracts interest from the rest of Canada and from the United States.
Residents and graduate students present their research projects. Their posters and oral presentations are judged every year by our expert panel of judges.
Tuesday June 21, 2016 will mark the 11th Annual London Imaging Discovery, an event showcasing the best and brightest residents, fellows, and scientists Schulich Medicine & Dentistry, Medical Imaging has to offer. This year, the venue will be at The Mercato, Brescia University College, 1285 Western Road.
The objectives of the event are as follows:
- To provide a forum for trainees, residents, and graduate students
- To enable residents and graduate students to learn and experience presenting to an audience
- To facilitate a congregation of knowledge with an extensive poster exhibition of research with the department
- To invite Keynote speakers on education and research to showcase their expertise
- To further develop the CANMEDS roles of Communicator and Collaborator through the focus on leadership development and relationship building
The event is free, open to all, and is a great opportunity to review the research at hand, enjoy refreshments and good company, and celebrate our successes over the past year.
Online registration and abstract submission is now open! For more information, please click here.