Search
Search
Understanding the COVID-19 virus through health research
In the early months of the COVID-19 pandemic, there was little known about the virus that was causing the COVID-19 illness. Hospital researchers in London, Ontario, through Lawson Health Research Institute, quickly got to work to study and better understand the SARS-CoV-2 virus. Lawson is the research arm of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London.
“When the pandemic hit, we were well prepared in London to start research studies. We had existing expertise, laboratories and teams through the hospitals, Lawson and Western University that could be mobilized quickly,” explains Dr. Douglas Fraser, Critical Care Physician at LHSC and Scientist at Lawson. “Patients started coming to hospital with COVID-19 and we began research that involved collecting human samples and bringing them to the lab for analysis.”
Dr. Fraser, who is also a Professor at Western’s Schulich School of Medicine & Dentistry, led the research team studying the samples from COVID-19 patients in hospital. “We learned very quickly that COVID-19 patients were experiencing a strong inflammatory response to the virus. We looked at the molecules involved because many of these are signaling molecules to the immune system.”

Dr. Douglas Fraser, Critical Care Physician (LHSC) and Lawson Scientist
“By studying the molecules, we were able to determine the pathways. This is important because it also points to how we should be targeting our diagnostics and therapeutics,” adds Dr Fraser.
As a hospital research institute, Lawson is uniquely positioned to address the medical questions posed by a new virus. Its Clinical Research Services (LCRS) and Center for Clinical Investigation and Therapeutics (CCIT) teams responded rapidly when researchers initiated COVID-19 studies, including Dr. Fraser’s study to examine the immune response in patients with COVID-19.
“Starting a clinical trial usually takes a certain amount of time to put together, but the pandemic created a perfect storm,” explains Sue Tereschyn, Manager of LCRS at Lawson. “Clinical researchers had to develop studies at a speed they have never seen, and they needed implementation support at the same speed. In Dr. Fraser’s case, we needed samples from the Intensive Care Unit (ICU) and we were processing samples from COVID-19 patients seven days a week. A high level of skill was needed.”
Dr. Fraser and his team soon became the first in the world to understand the immune response and several pathophysiological features of the virus. This work led to a critical understanding of how the virus was impacting patients and potential avenues for therapy.
“It’s important to understand what’s happening in the body when someone has COVID-19 because that gives us information as to why some patients don’t do well and why others recover,” shares Dr. Fraser. “This helps us know who is vulnerable to COVID-19 and how to best offer treatments in the future.”
Read about Dr. Fraser's COVID-19 research:
- Researchers team up with Diagnostics Biochem Canada to study COVID-19
- Study identifies biomarkers that could be used in a quick, inexpensive COVID-19 blood screening tool
- Researchers unravel two mysteries of COVID-19
Work is also underway to find the unique fingerprint that the COVID-19 virus can leave on the lungs. Hospital researchers at Lawson have developed and tested an artificial neural network for diagnosing COVID-19.

Dr. Robert Arntfield, Medical Director, Critical Care Trauma Centre (LHSC) and Lawson Researcher
“The lung ultrasound techniques and the findings of COVID-19 by looking at the lungs didn’t initially look unique when compared to other conditions like pneumonia. Our group wanted to investigate whether or not there were differences that were possibly subvisible,” says Dr. Robert Arntfield, Medical Director of Critical Care Trauma Centre at LHSC and Lawson Researcher. “Through our work, we were able to show that in fact artificial intelligence could outperform a trained clinician in identifying a COVID-19 lung from a similar affected lung that was not due to COVID-19.”
This new technique just scratches the surface of the beneficial use of AI when it comes to medical imaging for patients. “It shone a light on the idea that there were hidden details within all the noise of the image,” adds. Dr. Arntfield. “When you can input that into a machine that is extremely portable the way ultrasounds are, you have a precise diagnostic machine that you can take anywhere a tablet can go.”
The team is now expanding on these findings with further research. Lawson has recently approved Dr. Arntfield’s “Project Deep Breath” which aims to go beyond COVID-19 and explore multiple conditions where lung ultrasounds and AI can be paired together.
Unique imaging research by Lawson sparks international collaboration
The Bioelectromagnetics and Human Threshold Research Group at Lawson Health Research Institute has an international reputation and expertise on human brain response to time-varying magnetic fields (MFs). This pioneering research has inspired an international collaboration to duplicate Lawson Imaging’s unique experimental expertise in Europe.
The team is now working with EuroMov, a research centre located in France, to duplicate the scientific approach and techniques in a new lab. The goal is to double research capabilities and further stimulate scientific knowledge in this area.
Fluctuating MF induces electric fields and currents in conductive tissues. Above a certain threshold, these fields and currents will change the physiological electric activity within neuronal tissues. Lawson’s team is currently the only one in the world stimulating participants with power-frequency MF of sufficient intensity to result in acute neurophysiological response. This can involve interferences with visual perception, motor output and other cognitive functions.
“An international synergy between the Bioelectromagnetics and Human Threshold Research Group at Lawson and EuroMov will increase the scope of scientific expertise for both institutions” explains Dr. Legros, Director of Bioelectromagnetics and the Human Threshold Research Group at Lawson Imaging. “Both will have access to a wide range of brain stimulation techniques and imaging modalities.”
Through this new collaboration, researchers are excited to merge their expertise and tackle questions together, opening new avenues for original research ideas and projects. This new intercontinental synergy also increases the scope of options for academic funding and international training programs for students.
Furthermore, there is great potential for reinforcing and extending the group’s industry-partnered supporting program, which already associates industry sponsors (such as Hydro-Québec, Électricité De France, Réseau de Transport d’Électricité, NationalGrid/Energy Network Association, Electric Power Research Institute) under an international consortium: the Utilities Threshold Initiative Consortium (UTIC).
The growing network of international scientists working in this field assist international regulation agencies, governments and industries to better understand the impact of electromagnetic exposure on brain activity and physical behaviour. Knowing the thresholds for human responses allows these institutions to adjust their recommendations and policies for when exposures could become unsafe for the public and workers.
The potential applications in research, industry and health care are vast, including the world of video gaming and virtual reality!
“We are excited to see discovered effects and mechanisms translated towards therapeutic applications to the benefit of patients,” says Dr. Legros. “For example, we could improve neuromodulation and neurostimulation technologies to better address movement disorders such as in Parkinson’s Disease. In another application, knowledge of the vestibular responses to stimulation may help to manage symptoms such as motion sickness.”
EuroMov is a university-based European centre for research and innovation in the science of movement. Conducting both fundamental and clinical research, it proposes innovative technological solutions allowing the capture, simulation, learning and rehabilitation of movement. EuroMov contributes to the creation of innovative starts ups and businesses in the field of health, performance, sport, human factors, and rehabilitation.
Dr. Legros is also an Associate Professor in the Departments of Medical Biophysics, Medical Imaging and Kinesiology at Western University’s School of Kinesiology, and an Associate Scientist at EuroMov.
Find out more about his research:

Above: Members of the Bioelectromagnetics and Human Threshold Research Group at Lawson.
From left to right, bottom: Shirin Davarpanah Jazi, Postdoctoral Scholar; Alicia Allen, Masters Candidate; Cadence Maureen Baker, Masters Candidate.
From left to right, top: Michael Corbacio, RA/Lab Manager); Dr. Alexandre Legros, Principal Investigator and group leader; Sebastien Villard, Postdoctoral Scholar.
Missing from the photo: Nicolas Bouisset, PhD Candidate; Lynn Keenliside; Manager Technical Services.
Unlocking boundless potential
Ashmeet Gill had her first PET/CT scan shortly after being diagnosed with Hodgkin’s lymphoma, a cancer of the body’s germ-fighting immune system. She was nervous. Claustrophobia is an issue for the young Stratford resident and the scan, necessary to determine if the cancer had spread beyond the lymph nodes in her neck, would take 34 to 45 minutes, she was told.
Wrapped in a sheet and tucked inside the tube of the PET/CT at St. Joseph’s Health Care London (St. Joseph’s), Ashmeet, then 24, steeled herself to remain calm. But near the end of the scan, a sense of panic set in.
“It was not pleasant but I endured it. I made it through.”
Ashmeet’s next PET/CT scan would be six months later, after six cycles of chemotherapy, to determine if the treatment had worked. She was terrified of another panic episode. By then, however, St. Joseph’s had a brand-new PET/CT – Canada’s first, next generation, state-of-the-art Omni Legend PET/CT from GE HealthCare.
This time, Ashmeet’s scan took “barely 15 minutes or so,” she recalled.
“I thought, seriously? I couldn’t believe I was done. I was so happy.”
With the very first patients scanned with St. Joseph’s new PET/CT machine, it was obvious the breakthrough technology was living up to high expectations.
The machine is fast – decreasing the time it took for a scan from about 45 minutes on the older system to less than 14 – head to toe. Patients are exposed to less radiation, and the ability to precisely detect disease and tiny abnormalities is outstanding.
“This is what we have been waiting for,” says Ting-Yim Lee, a pioneer in the use of machines like PET/CT to gather new, vital information about diseases. “St. Joseph’s new Omni Legend by GE HealthCare is answering the call for patients, clinicians and researchers alike.”
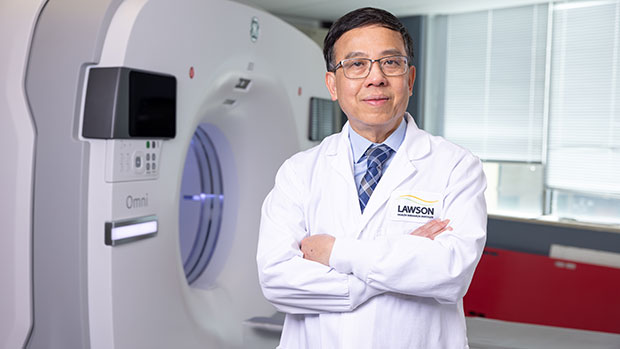
PET/CT is the medical ace in imaging for the assessment and treatment monitoring of cancer, neurodegenerative disorders, and metabolic and cardiovascular diseases. At St. Joseph’s, the possibilities of this technology took a giant leap forward in August 2023, thanks in part to the generosity of donors and a $1 million contribution from St. Joseph’s Health Care Foundation. With the arrival of the new system, St. Joseph’s is set to become Canada’s first national GE HealthCare centre of excellence in molecular imaging and theranostics. This two-pronged approach to diagnosing and treating cancers and other diseases merges molecular imaging with the use of radiopharmaceuticals to identify the location and extent of diseased tissues and selectively destroy the abnormal cells.
“The speed at which we can now do exams means significantly improved comfort for patients while the exceptional image quality changes the game in the hunt for cancerous lesions,” explains Ting, Director of PET/CT Research at Lawson Health Research Institute (Lawson) and medical physicist at St. Joseph’s Hospital.
“For young adults undergoing repeat PET/CT exams due to their medical conditions, managing the radiation dose is critical,” explains Dr. Narinder Paul, Lawson scientist and Chief, Medical Imaging, at St. Joseph’s. “These individuals already face an elevated life-time risk of developing cancer from radiation, and this risk further increases with additional exposures.”
For older adults, the time it takes for the examination is also of great concern. Lying still for long periods can be a hardship due to pain from bone metastases or other conditions, and is a challenge for those who have dementia, are claustrophobic or experiencing other issues, adds Dr. Paul.
“Reducing the exam time is a huge improvement in the patient experience for these individuals.”
While patients hail the new PET/CT experience, clinicians and scientists are raving about the machine’s imaging prowess. The advanced AI-driven image formation technology now empowers the precise detection of cancer within lymph nodes and other anatomical structures, “achieving remarkable accuracy even for very small lesions,” says Dr. Paul.
“The advantages we have seen so far are already impressive but what’s on the horizon in research and care – what we will be able to study and do – is even more exciting,” says Ting.
In particular, the new PET/CT is expected to be the catalyst for ground-breaking clinical research for patients facing breast cancer, Alzheimer’s disease, prostate cancer, epilepsy and obesity. Scientific exploration in these areas is currently being planned at St. Joseph’s that will pave the way for novel treatments, new, non-invasive ways to identify a patient’s risk of disease, the potential to clearly and painlessly view how treatment is working, and the ability to uncover the tiniest abnormalities at play when it comes to diseases and conditions.
The deets on PET-CT
Positron emission tomography (PET) is a medical imaging method that uses a small amount of radioactive material, called a radiotracer or radiopharmaceutical, along with a special camera and computer. This helps doctors see how organs and tissues in the body are working. The radiotracer moves through the body and collects in specific areas, showing where there might be a problem or disease. PET can also be used to check how well a patient is responding to treatment.
A computed tomography (CT) scan takes x-ray images of the body from different angles and uses computer processing to create highly detailed, cross-sectional images (slices) of the body’s structures. It is used to see things that regular X-rays can’t show.
A PET-CT machine allows both types of scans to be performed at the same time and information from these two different types of scans to be viewed on a single set of images. Together, PET-CT provides intricate views with fine details about both the body’s various structures and their functions.
Peering into the future
The following are landmark research projects nearing the starting gate at Lawson Health Research Institute made possible by St. Joseph’s Health Care London’s revolutionary new PET-CT machine.
Breast Cancer
Within the Breast Care Program at St. Joseph’s, research with the new PET-CT scanner will make breast cancer theranostics a clinical reality for the first time worldwide. In other words, it will be possible to treat breast cancer using the powerful, one-two punch of molecular imaging and radiopharmaceuticals to identify the location and extent of diseased tissues and selectively destroy the abnormal cells. Two exciting projects are on the horizon:
The one-two punch: Herceptin is a cancer medicine that interferes with the growth and spread of cancer cells in the body. HER2-positive breast cancer is a type of breast cancer that is more aggressive than other types. By using PET-CT imaging with a specialized form of Herceptin that has been chemically tagged, or "labeled," with a radioactive substance, researchers believe it’s possible for a woman to avoid undergoing a breast biopsy. They will be able to see – literally – if the radiolabeled Herceptin binds to the HER2 proteins and the extent of the HER2-positive cancer. Then, by tagging Herceptin with a therapeutic radioisotope – a special type of atom that emits radiation – the hope is to destroy the breast cancer. St. Joseph’s is investigating this approach first in animal studies before progressing into human trials.
Reducing the risk: Not all breast cancers can be effectively treated with Herceptin. For this group of patients, researchers plan to evaluate newer drugs to reduce the risk of both disease progression and death. The new PET-CT scanner will be able to monitor response from these new treatments.
Alzheimer's disease
The super sensitivity of St. Joseph’s new PET-CT will empower innovative methods to identify individuals at risk of Alzheimer’s disease, those who might benefit from treatment, and early response to treatment. The high-powered machine will allow researchers to simultaneously study both blood flow and glucose metabolism in the brain – something that has not been possible before. Both these mechanisms are believed to be contributing factors in the onset of Alzheimer’s. By measuring both at the same time, researchers hope to uncover early signs that the brain is in trouble and at risk of plaque deposits and toxic proteins that have been linked to the development of Alzheimer’s. Patients will be recruited from St. Joseph’s Aging Brain and Memory Clinic at Parkwood Institute for this ground-breaking study.
Epilepsy
Patients with uncontrolled seizures currently require a hospital stay and the implanting of electrodes deep into the brain to record brain signals that pinpoint where the epileptic seizures are originating. The hospital stay is often long as this method relies on the patient having seizures to properly record and identify the location in the brain responsible. Once the problem area is determined, surgeons intricately remove this part of the brain. Research with the new PET-CT will explore a more efficient approach – the ability to precisely reveal the brain’s seizure epicentre using non-invasive imaging looking at characteristics in the epileptic brain that is present between seizures.
Obesity
In Canada, one in four adults are currently living with obesity, a problem that is causing a surge of obesity-related health challenges. Ozempic is a ground-breaking drug that not only helps people shed weight but also slashes the risk of heart disease by an impressive 20 per cent. However, weight loss attributed to this drug is linked to a reduction in lean muscle mass and the long term effects of that muscle loss remain uncertain. Using PET-CT, researchers will explore potential alterations in muscle energy metabolism resulting from obesity treatment with Ozempic and similar drugs.
Using AI to detect lung cancer recurrence
Lung cancer is the most commonly diagnosed cancer in Canada. While the standard treatment for patients with early-stage lung cancer is surgery, up to half of these patients may develop a recurrence after their treatment.
Jaryd Christie is a Master’s candidate working with Lawson Scientist, Dr. Sarah Mattonen. Together, they are working to develop a new software that uses artificial intelligence (AI) to identify which patients are likely to have recurring cancer.
Currently, basic information like the size of the tumour is extracted from medical images such as a computed tomography (CT) scan to determine a patient’s cancer stage and prognosis. With the new technology, multiple sources of information about the patient will be extracted and used to increase accuracy for determining likelihood of recurrence.
Christie is looking to integrate multi-modal imaging, including CT and positron emission tomography (PET) with a patient’s clinical, pathological and genomic information to build the software. The AI software will find patterns from the data that is extracted and identify imaging features that are associated with recurrence after treatment.
The goal of this research is to improve the ability to identify which patients are likely to be cured. By being able to extract and combine additional information, physicians could provide aggressive treatment options for patients who need it. This would provide lung cancer patients with personalized treatments that could improve their outcomes.
“We also want to look not only at the tumour, but other places like bone marrow and non-cancerous areas in the lung, to see if these additional areas can provide information on disease progression and prognosis,” says Christie, who is completing his Master’s degree in the Department of Medical Biophysics at the Schulich School of Medicine & Dentistry at Western University. “We hope that by combining these different sources of information, we can obtain better disease characterization to more accurately determine if a patient will be cured.”
Christie received a Lawson Internal Research Fund (IRF) Studentship to conduct this research, which will be supervised by Dr. Mattonen.
“Lawson’s IRF is such an important funding opportunity for new investigators. This studentship allows me to support a student while building my research program,” adds Dr. Mattonen. “These funds will allow us to obtain preliminary data that we can use to apply for external funding.”
Using artificial intelligence and brain stimulation to improve treatment for psychosis
Leading the Canadian arm of the project is Dr. Lena Palaniyappan who is using Artificial Intelligence to help personalize treatment for patients with psychosis. Dr. Palaniyappan is an Associate Scientist at Lawson Health Research Institute, Associate Professor at Schulich Medicine & Dentistry and Scientist at Robarts Research Institute.

Dr. Lena Palaniyappan who is using AI to help personalize treatment for patients with psychosis.
In collaboration with five European centres, Dr. Palaniyappan and a team at Robarts Research Institute and Lawson Health Research Institute, the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, will be collecting brain scans and genetic information from more than 60,000 patients in order to understand the relationship between genetics and brain development.
“The study itself involves collecting neuroimaging and genetic information from multiple sites in order to understand the mechanisms of mental illness,” said Dr. Palaniyappan. “The translational portion of this is applying this information to clinic. How genes and brain networks interact to cause mental disorders, and how we can use this information to match patients to specific treatment choices.”
The group is specifically studying a treatment called magnetic stimulation which will be delivered within the mental health care program at St. Parkwood Institute, a part of St. Joseph’s, in collaboration with Dr. Amer Burhan. Dr. Burhan is a Lawson Associate Scientist, Associate Professor at Schulich Medicine & Dentistry and Clinical Physician Lead for Therapeutic Brain Stimulation (ECT and TMS) at Parkwood Institute.

Dr. Lena Palaniyappan is collaborating with Dr. Amer Burhan for this study.
The treatment uses focused magnetic pulses that stimulate a specific group of neurons. Dr. Palaniyappan says the treatment is very effective, but only in one-third of patients.
“We want to know if there are clear markers that show who will respond to this treatment, and who will not. This will help reduce the burden of failed treatment trials for this challenging illness,” said Dr. Palaniyappan.
To enable this, the researchers will look for patterns in a very large amount of imaging and clinical data collected in Europe and Canada. That’s where Artificial Intelligence comes in. In order to understand the patterns that are clinically useful, they use a technique called Machine Learning that trains a computer to recognize expected patterns and then make predictions for new patients.
The data is being collected from six centres, coordinated by Dr. Emanuel Schwarz at the University of Heidelberg, Mannheim, Germany. In addition to the centre here in London, Ontario, other partners include Munich, Germany; Oslo, Norway; Rotterdam, Netherlands; and Montpellier, France.
The research project will also mean that this form of magnetic stimulation treatment will be offered for psychosis patients in London for the first time.
“Magnetic brain stimulation is a safe and well-tolerated treatment that is used currently in London to treat depression, but now we will be able to offer this to patients with psychosis as well,” said Dr. Palaniyappan.
The project will begin in May 2019 and will continue until the end of 2022.
View St. Joseph’s Health Care London's 2016-2017 Annual Report
St. Joseph’s Health Care London’s 2016-2017 Annual Report features stories of care, recovery, discovery, teaching and resiliency – of care teams, patients, residents, and their families.
Included in the 2016-2017 Annual Report are the following research stories:
- New imaging research chairs make history: In a historical-first, St. Joseph’s Health Care Foundation and Western University announced two research chairs to advance imaging research at Western University and Lawson Health Research Institute. The research chairs have been named after the two scientists who are revolutionizing health care through their groundbreaking imaging research – Drs. Ting-Yim Lee and Frank Prato.
- A world-first approach to dementia: Researchers at Lawson Health Research Institute are the first in the world conducting a clinical trial to test a triple intervention aimed at treating mild cognitive impairment (MCI) and delaying the onset of dementia. The Mobility, Exercise and Cognition (MEC) team will be incorporating physical exercises, cognitive training and vitamin D supplementation to determine the best treatment for improving mobility and cognition.
- First clinical guidelines in Canada for pain following spinal cord injury: Researchers at Lawson Health Research Institute are the first in Canada to develop clinical practice guidelines that address the unique challenges for managing pain during recovery and rehabilitation from spinal cord injury.
- CAHO HWS field trip to Lawson: The Council of Academic Hospitals of Ontario (CAHO) toured the labs of Lawson Health Research Institute to encourage stable investment in hospital-based research and showcase the groundbreaking work underway at St. Joseph’s and London Health Sciences Centre.
- iSee Vision Screening Research Program: iSee, an innovative vision screening research program of St. Joseph’s Ivey Eye Institute is catching problems early for children ages 18 months to five years. The screening, which takes only seconds, detects amblyopia (lazy eye) and other eye conditions that can cause poor vision
View St. Joseph’s Health Care London's 2017-2018 Annual Report
St. Joseph’s Health Care London’s 2017-2018 Annual Report features stories about patients and residents, and their journey of care and recovery.
The following research is highlighted in the 2017-2018 Annual Report:
- Smart tech, smart treatment: Many mobile applications are on the market to help people struggling with mental health issues, but these aren’t necessarily created or used by health care providers. Creating an entire smart mental health system is one of the strategic priorities of St. Joseph’s and Lawson’s Mental Health Research Group led by Dr. Cheryl Forchuk, Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery. Numerous projects have been identified as components of a plan spanning seven years.
- Walking while talking a possible early predictor of dementia: In a new study, researchers at Lawson and Western University are demonstrating that gait, or motion testing, while simultaneously performing a cognitively demanding task can effectively predict the progression to dementia and eventually help with earlier diagnosis. To date, there is no definitive way for health care professionals to forecast the onset of dementia in a patient with memory complaints.
Viral mouth-taping trend ‘sus’ says Canadian sleep expert
Mouth taping, a growing trend on social media channels like TikTok, carries serious health risks, especially for those with sleep-disordered breathing and obstructive sleep apnea, according to a paper published in PLOS One.
The study from Lawson Research Institute (Lawson) of St. Joseph’s Health Care London, London Health Sciences Centre Research Institute (LHSCRI) and Western University’s Schulich School of Medicine & Dentistry also found no strong evidence of health benefits.
The trend involves placing tape over the mouth to stop ‘mouth breathing’ and promote breathing through the nose during sleep. It has been recommended by many social media influencers and celebrities who claim it can lead to better sleep, enhanced oral health and anti-aging results.
“It was concerning to us that celebrities and influencers are endorsing mouth taping without scientific evidence,” says Dr. Brian Rotenberg, researcher at Lawson, LHSCRI and Schulich Medicine & Dentistry. “In the language of social media influencers, it seemed a bit ‘sus,’ so we examined what science is telling us about this trend and whether or not it is safe.”
Rotenberg collaborated with Dr. Elise Graham, paediatric otolaryngologist head and neck surgeon at IWK Health and Jess Rhee a Schulich School of Medicine & Dentistry resident who is training at London Health Sciences Centre (LHSC) on the research. He and his team examined 86 existing scientific studies on the topic, including an in-depth review of 10 studies representing the experience of 213 patients. The team found mouth taping:
- Has no strong scientific evidence of health benefits, contradicting claims on social media.
- Can make existing sleep-disorder breathing worse by restricting airflow, putting additional stress on the respiratory system and increasing risk of suffocation when patients experience a nasal obstruction.
“Our research shows that taping the mouth shut during sleep is dangerous, especially among those who may not be aware they have sleep apnea,” adds Rotenberg, who is also an otolaryngologist and sleep surgeon at St. Joseph’s Health Care London and London Health Sciences Centre (LHSC). “These individuals are unknowingly making their symptoms worse and putting themselves at greater risk for serious health complications like heart disease.”
Rotenberg and his team point to the importance of health research in combatting misinformation and pseudoscience.
“It’s easy for misinformation to run rampant on social media; we’ve seen this countless times over the past few years,” says Rhee. “We need to make health decisions based on strong scientific evidence. Our hope is that people stop taping their mouths during sleep and recognize it is dangerous.”
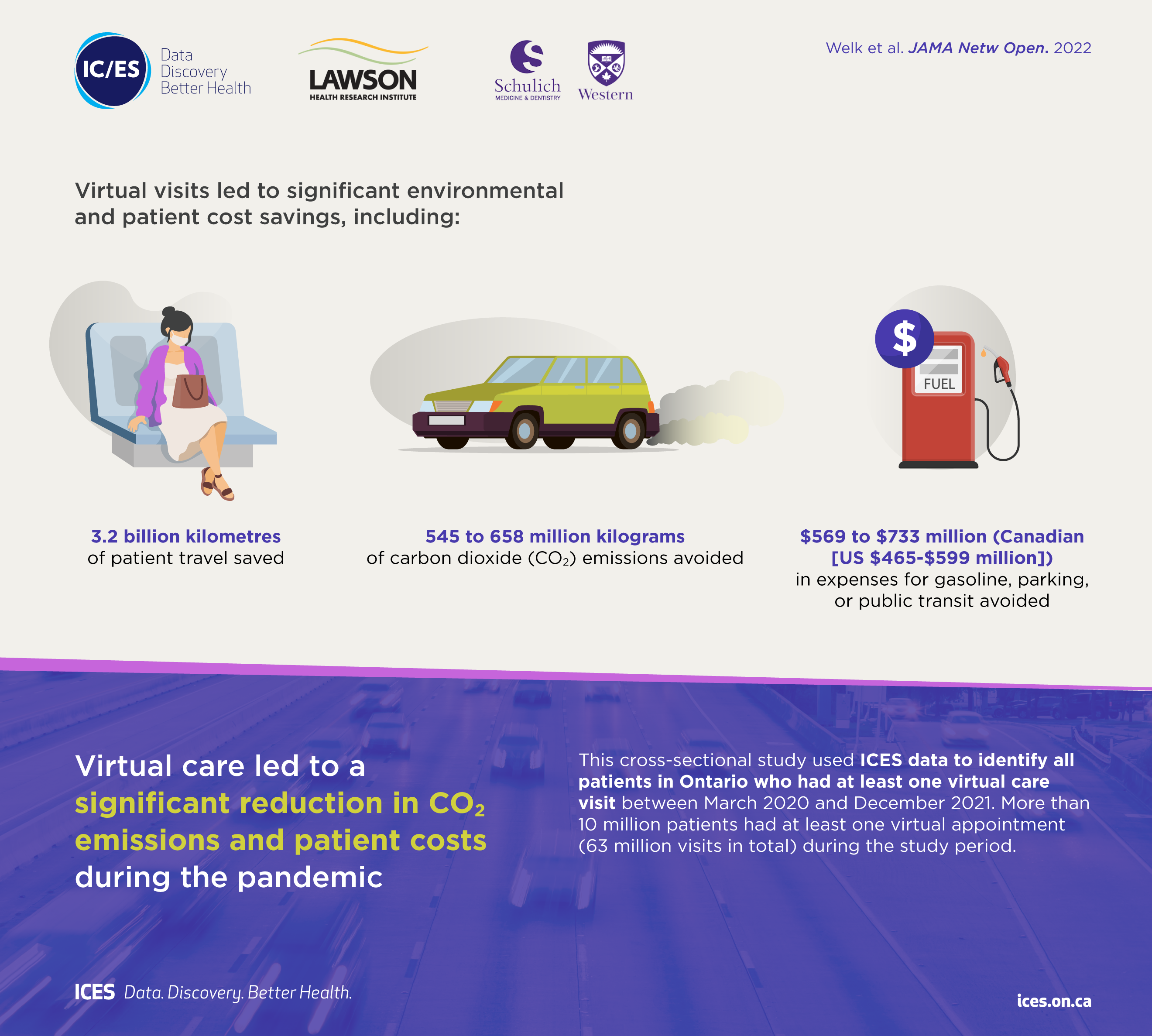
Virtual care associated with significant environmental and patient cost savings
London, ON - A new study by researchers at ICES, Lawson Health Research Institute and Western University finds that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs.
Prior to the pandemic, less than two per cent of patient visits with physicians took place virtually. The beginning of the pandemic (April-June 2020) triggered a rapid transition to virtual visits, which soared to 70 to 80 per cent, and then stabilized at 50 to 60 per cent of all physician visits.
This cross-sectional study published in JAMA Network Open used healthcare administrative data from Ontario, Canada to identify all patients with at least one virtual care visit between March 2020 and December 2021.
“Virtual care has become an important part of the healthcare system in Ontario, and in addition to improved patient convenience, it results in significant environmental and financial benefits for patients,” says lead author Dr. Blayne Welk, associate professor of surgery at Western's Schulich School of Medicine & Dentistry, urologist at St. Joseph’s Health Care London, associate scientist at Lawson, and adjunct scientist at ICES Western. “The financial and environmental benefits of virtual care will likely continue beyond the pandemic and are particularly relevant for some patients who were frequent recipients of virtual care.”
Findings show that for more than 10 million patients with at least one appointment during the study period (63 million visits in total), virtual care was associated with estimated savings of:
• 3.2 billion kilometres of patient travel;
• 545 to 658 million kilograms of carbon dioxide (CO2) emissions; and
• $569 to $733 million (Canadian [US $465-$599 million]) in expenses for gasoline, parking, or public transit.
The avoidance of carbon dioxide emissions during the pandemic due to virtual visits represented approximately 0.2 per cent of the total annual carbon dioxide emissions (150 megatons) from Ontario.
The number of virtual care visits was greater for those aged 65 and older, individuals with multiple health conditions, and those living in urban areas. Due to distance travelled, virtual care may offer more potential environmental benefits and patient cost savings for rural residents. Other factors, such as decreased time off work (given that some virtual visits can
be done during the day with little interruption to work) may have had additional benefits for some working adults and parents of young children.
“Virtual visits should not replace all in-person visits, but they are an important option that can enhance the care that physicians provide for patients,” says Dr. Alexandra Zorzi, a Paediatric Oncologist at Children’s Hospital at London Health Sciences Centre and Associate Scientist at Lawson. “Our findings suggest that physicians should continue to offer virtual care appointments when appropriate, especially for patients living in more remote areas and those that have barriers to accessing in-person health care.”
The study, “Association of virtual care expansion with environmental sustainability and reduced patient costs during the COVID-19 pandemic in Ontario, Canada” was published in JAMA Network Open.
Author block: Welk B, McArthur E, Zorzi AP.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
The Institute for Clinical Evaluative Sciences (ICES) is an independent, non-profit organization that uses population-based health information to produce knowledge on a broad range of health care issues. Our unbiased evidence provides measures of health system performance, a clearer understanding of the shifting health care needs of Ontarians, and a stimulus for discussion of practical solutions to optimize scarce resources. ICES knowledge is highly regarded in Canada and abroad, and is widely used by government, hospitals, planners, and practitioners to make decisions about care delivery and to develop policy. For the latest ICES news, follow us on Twitter: @ICESOntario
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Virtual care associated with significant environmental and patient cost savings
A new study by researchers at ICES, Lawson Health Research Institute and Western University finds that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs.
Prior to the pandemic, less than two per cent of patient visits with physicians took place virtually. The beginning of the pandemic (April-June 2020) triggered a rapid transition to virtual visits, which soared to 70 to 80 per cent, and then stabilized at 50 to 60 per cent of all physician visits.
This cross-sectional study published in JAMA Network Open used healthcare administrative data from Ontario, Canada to identify all patients with at least one virtual care visit between March 2020 and December 2021.
“Virtual care has become an important part of the healthcare system in Ontario, and in addition to improved patient convenience, it results in significant environmental and financial benefits for patients,” says lead author Dr. Blayne Welk, associate professor of surgery at Western's Schulich School of Medicine & Dentistry, urologist at St. Joseph’s Health Care London, associate scientist at Lawson, and adjunct scientist at ICES Western. “The financial and environmental benefits of virtual care will likely continue beyond the pandemic and are particularly relevant for some patients who were frequent recipients of virtual care.”
Findings show that for more than 10 million patients with at least one appointment during the study period (63 million visits in total), virtual care was associated with estimated savings of:
• 3.2 billion kilometres of patient travel;
• 545 to 658 million kilograms of carbon dioxide (CO2) emissions; and
• $569 to $733 million (Canadian [US $465-$599 million]) in expenses for gasoline, parking, or public transit.
The avoidance of carbon dioxide emissions during the pandemic due to virtual visits represented approximately 0.2 per cent of the total annual carbon dioxide emissions (150 megatons) from Ontario.
The number of virtual care visits was greater for those aged 65 and older, individuals with multiple health conditions, and those living in urban areas. Due to distance travelled, virtual care may offer more potential environmental benefits and patient cost savings for rural residents. Other factors, such as decreased time off work (given that some virtual visits can be done during the day with little interruption to work) may have had additional benefits for some working adults and parents of young children.
“Virtual visits should not replace all in-person visits, but they are an important option that can enhance the care that physicians provide for patients,” says Dr. Alexandra Zorzi, a Paediatric Oncologist at Children’s Hospital at London Health Sciences Centre and Associate Scientist at Lawson. “Our findings suggest that physicians should continue to offer virtual care appointments when appropriate, especially for patients living in more remote areas and those that have barriers to accessing in-person health care.”
The study, “Association of virtual care expansion with environmental sustainability and reduced patient costs during the COVID-19 pandemic in Ontario, Canada” was published in JAMA Network Open.
Author block: Welk B, McArthur E, Zorzi AP.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca