Search
Search
3D imaging technology could improve outcomes for patients with breast cancer
A study at Lawson is looking to determine if digital breast tomosynthesis, a type of 3D imaging, is better at detecting breast tissue abnormalities than the 2D mammography regularly used today.
During a conventional digital 2D mammogram, two x-ray images are taken of the breast, one from top-to-bottom and another from side-to-side at an angle. This technology is limited by the overlapping breast tissue that occurs from the required compression of the breast, and breast abnormalities may be hidden.
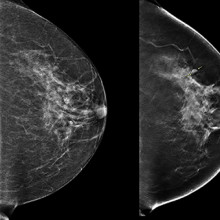
(Left) 2D mammogram image of left breast, where no lesion was visible. (Right) 3D tomographic image of the same breast showing a lesion, indicated by arrows.
A tomosynthesis exam is relatively new technology in which the x-ray tube moves in an arc over the compressed breast and captures multiple images from different angles. The images are then reconstructed into a set of 3D images by a computer. By being able to examine the breast at multiple layers of depth, the radiologist is better able to distinguish normal breast tissue from potential abnormalities. It is therefore assumed that tomosynthesis may solve some challenges associated with standard mammography, and could be especially useful for women with dense breast tissue.
In the Tomosynthesis Mammographic Imaging Screening Trial (TMIST), women are randomized to receive screening with standard digital 2D mammography, or digital 2D mammography plus tomosynthesis. Participants will undergo either an annual or biennial screening frequency, depending on their risk factors for breast cancer, for approximately four years. Then participants will undergo long-term follow-up for at least three more years. Researchers hope this study will help radiologists evaluate whether the newer technology of tomosynthesis is indeed a more effective tool for detecting aggressive tumours.
Through the Ontario Breast Screening Program (OBSP), women between the ages of 50 and 75 receive regular notices through the mail, encouraging them to schedule a mammogram for breast cancer screening. Women scheduled for a regular OBSP breast exam at St. Joseph’s Hospital London (St. Joseph’s) receive a letter with the study’s contact information. Eligible participants are enrolled at the time of their scheduled appointment. Participating in the study does not significantly change the overall experience of the breast exam.
“Our goal is to contribute to the body of evidence around tomosynthesis technology, and ultimately, we hope to improve the outcomes for women diagnosed with breast cancer, meaning, earlier detection,” says Dr. Anat Kornecki, Lawson Scientist and Radiologist at St. Joseph’s.
The TMIST study is being conducted in over 100 centres across Canada, the United States, and Argentina. Approximately 165,000 participants will be recruited.
A “safety net of relationships” to bridge the gap between hospital and community at discharge
A beneficial and cost-effective approach to mental health care that supports people as they go from hospital and back into the community is outlined in a new resource and has been recognized internationally by the World Health Organization (WHO).
"The immediate period after discharge from hospital, usually the first month, can be one of the most vulnerable times in the life of someone experiencing a mental illness. It can be when they are most at risk of committing suicide,” explains Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson Health Research Institute. “However, what we’ve seen is that there’s often a gap between when someone says ‘goodbye’ to the hospital inpatient unit and ‘hello’ to the community care provider.”
During a virtual book launch, a research team from Lawson and several community organizations discussed details of a new publication from Routledge, From Therapeutic Relationships to Transitional Care: A Theoretical and Practical Roadmap, edited by Dr. Forchuk. The book combines theory, research and best practices into a “roadmap” for organizations and others worldwide coordinating services or studying mental health care systems. It includes a practical toolkit for implementing the Transitional Discharge Model (TDM), developed and tested in communities across Ontario.
Purchase your copy of the book HERE and enter promo code SMAO3 at checkout for a 20% discount.

How Transitional Discharge works
TDM was born from a participatory action project with consumers of mental health services. They identified two factors that were most important to them when they were going from hospital to the community: consistency in therapeutic relationships and a supportive peer friendship.
It became known as a “safety net of relationships” that would bridge the gap between hospital and community services.
As a person-centred, evidence-based model, transitional discharge supports a smooth adjustment from hospital to community in two main ways:
- The inpatient staff continue to care for discharged clients until therapeutic relationships are established with community care providers.
- A friendship model of support with trained peer support workers who have lived experience of mental illness as they have made the same journey.

Perspective of a TDM client and peer support coach
Lance Dingman was a TDM client during the early phases of the project. “It makes a big difference when you’re able to get back to living in the community and in your own dwelling. You get to make more of your own decisions and learn about what you want to do. You grow with your experience and the guidance of others who are there to support you.”
Later becoming a peer support coach, Dingman feels implementing TDM for mental health care is important because people can learn from each other and get healthier in the process. “As a peer support worker, I sit with people and they tell me their story. It takes me back and I know what they are going through – I was where they are. I can share my own story and tell them what I did to get better.”
Cost-analysis and savings for the system
Dr. Forchuk’s team analyzed the cost of TDM after being tested in nine hospitals across Ontario, including London Health Sciences Centre and St. Joseph’s Health Care London.
- On average, the length of stay in hospital was reduced by almost 10 (9.8) days per admission.
- Each site saved approximately $3.3 million per year.
“People can return home sooner because a higher level of care and support is in place when they leave hospital. If all hospitals in Ontario with mental health services were able to implement our transitional discharge model, we would save $60 million per year in hospital stay costs alone while providing enhanced mental health care.”
International implementation
In Scotland, the parliament has already declared TDM as a best practice after demonstrating a significant reduction in readmission rates.
The TDM approach is now considered a “good practice” by WHO and was recently the only Canadian example included in its Guidance on community mental health services: Promoting person-centered and rights-based approaches. This set of publications provides information and support to all stakeholders who wish to develop or transform their mental health system and services to align with international human rights standards including the UN Convention on the Rights of Persons with Disabilities.
A “safety net of relationships” to bridge the gap between hospital and community at discharge
LONDON, ON – A beneficial and cost-effective approach to mental health care that supports people as they go from hospital and back into the community is outlined in a new resource and has been recognized internationally by the World Health Organization (WHO).
“The immediate period after discharge from hospital, usually the first month, can be one of the most vulnerable times in the life of someone experiencing a mental illness. It can be when they are most at risk of committing suicide,” explains Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson Health Research Institute. “However, what we’ve seen is that there’s often a gap between when someone says ‘goodbye’ to the hospital inpatient unit and ‘hello’ to the community care provider.”
Today during a virtual book launch, a research team from Lawson and several community organizations discussed details of a new publication from Routledge, From Therapeutic Relationships to Transitional Care: A Theoretical and Practical Roadmap, edited by Dr. Forchuk. The book combines theory, research and best practices into a “roadmap” for organizations and others worldwide coordinating services or studying mental health care systems. It includes a practical toolkit for implementing the Transitional Discharge Model (TDM), developed and tested in communities across Ontario.
TDM was born from a participatory action project with consumers of mental health services. They identified two factors that were most important to them when they were going from hospital to the community: consistency in therapeutic relationships and a supportive peer friendship. They described it as a “safety net of relationships” that would bridge the gap between hospital and community services.
“As a person-centred, evidence-based model, transitional discharge supports a smooth adjustment from hospital to community,” says Dr. Forchuk. “The inpatient staff continue to care for discharged clients until therapeutic relationships are established with community care providers. At the same time, we have a friendship model of peer support. These are trained people with lived experience of mental illness who have made the same journey.”
Lance Dingman was a TDM client during the early phases of the project. “It makes a big difference when you’re able to get back to living in the community and in your own dwelling. You get to make more of your own decisions and learn about what you want to do. You grow with your experience and the guidance of others who are there to support you.”
Later becoming a peer support coach, Dingman feels implementing TDM for mental health care is important because people can learn from each other and get healthier in the process. “As a peer support worker, I sit with people and they tell me their story. It takes me back and I know what they are going through – I was where they are. I can share my own story and tell them what I did to get better.”
Dr. Forchuk’s team analyzed the cost of TDM after being tested in nine hospitals across Ontario, including London Health Sciences Centre and St. Joseph’s Health Care London. On average, the length of stay in hospital was reduced by almost 10 (9.8) days per admission and each site saved approximately $3.3 million per year. “People can return home sooner because a higher level of care and support is in place when they leave hospital. If all hospitals in Ontario with mental health services were able to implement our transitional discharge model, we would save $60 million per year in hospital stay costs alone while providing enhanced mental health care.”
The TDM approach is now considered a “good practice” by WHO and was recently the only Canadian example included in its Guidance on community mental health services: Promoting person-centered and rights-based approaches. This set of publications provides information and support to all stakeholders who wish to develop or transform their mental health system and services to align with international human rights standards including the UN Convention on the Rights of Persons with Disabilities.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
A golden age in microbiome research
According to Dr. Jeremy Burton, we’re in a golden age of microbiome and probiotics research.
“Thanks to advancements in next-generation sequencing, we’re learning more and more every day about the impacts of the microbiome on the human body,” states Dr. Burton.
Effective September 1, 2020, Dr. Burton has been appointed as Research Chair in Human Microbiome and Probiotics at Lawson Health Research Institute for a five-year term. As part of the Chair’s responsibilities, Dr. Burton will also assume the title of Director for the Canadian Centre for Human Microbiome and Probiotics Research, which is located at Lawson.
Funded by an endowment through St. Joseph’s Health Care Foundation, the position is responsible for leading Lawson’s Human Microbiome and Probiotics research program. The specialized research chair was established at St. Joseph’s in 2007 as a result of a significant investment by Danone International, in recognition of groundbreaking microbiome research by Dr. Gregor Reid, the inaugural holder of the Chair.
With extensive experience in both academia and industry, Dr. Burton is a world-renowned scientist specializing in urinary microbiome research. He points to the diversity of microbiome research at Lawson as a strength to be leveraged.
“Our program is conducting a diverse array of microbiota-related research from probiotic studies to fecal transplants to the investigation of drug-microbiome interactions,” explains Dr. Burton. “There’s a lot of interest in conducting microbiome research as it’s become clear how it affects so many human systems. We are also working with a number of other groups across the city – both clinical and basic sciences – to meet their microbiota-related research needs.”
There are two pillars to Dr. Burton’s vision for microbiome and probiotics research at Lawson. The first is advancing translational research that leads to improved patient outcomes, such as new microbial therapies. The second is improving our understanding of the microbiome by studying its function in real-time.
“In most studies, we collect patient samples, put them in the freezer and then analyze them later. We now want to follow people in real-time to get a better understanding of how the microbiome functions inside the human body,” notes Dr. Burton. “We hope to accomplish this by harnessing technologies already available at Lawson. For example, we’ve been collaborating with the Lawson Imaging program to look at bacteria in real-time using the Institute’s imaging technology.”

Above: Dr. Jeremy Burton (right) in the lab with Dr. Kait Al (left), Postdoctoral Fellow
Dr. Burton is known for forging strong interdisciplinary relationships to enhance knowledge translation, especially within the Division of Urology.
“Dr. Burton has established a robust academic laboratory and strategic partnerships that are advancing the Institute’s scientific mandate. He is a natural leader,” says Dr. David Hill, Lawson Scientific Director. “As Research Chair in Human Microbiome and Probiotics, Dr. Burton will further Lawson’s reputation in the field.”
Dr. Burton will build on a 30-year legacy of microbiome research.
“There’s a long history of microbiome research at Lawson and St. Joseph’s,” he says. “We were lucky to have visionaries like Dr. Gregor Reid – my predecessor in this position – who have helped revolutionize the field.”
For Dr. Burton, this is the next step in an illustrious career with Lawson. He first joined the Institute and Western University’s Schulich School of Medicine & Dentistry as a Postdoctoral Fellow in 2001 after completing his BSc, MSc and PhD at the University of Otago in New Zealand.
“I had a very productive time as a Fellow, publishing something like 15 manuscripts in two years. It was an amazing experience and a time that I really relished.”
He was then recruited to industry in 2003 where he developed a strong background in clinical trials and global business development.
“Working in industry helped shape me into the principal investigator that I am today. But there were so many questions about the microbiome that I wanted to answer and I ultimately found myself back in academia.”
Dr. Burton rejoined Lawson as a Scientist in 2011. Prior to his appointment as Lawson Research Chair in Human Microbiome and Probiotics, he held the title of Deputy Director of the Canadian Centre for Human Microbiome and Probiotics Research since 2011 and Miriam Burnett Chair in Urological Sciences since 2013. He is also an Associate Professor in the Departments of Surgery and Microbiology and Immunology at Schulich Medicine & Dentistry.
“What brought me back to London is the people and the collaborative environment. Researchers cross departmental and divisional borders with ease. As a scientist, I can walk from my lab to a clinic, and clinician-researchers can do the same in reverse. Everyone has a ‘can do’ attitude and they are willing to test big ideas with one another.”
Learn about recent microbiome and probiotics research at Lawson:
- Gut microbiome may influence how cancer patients respond to oral therapies, study suggests
- New urinary microbiome study could be first step in providing personalized care to patients with ureteral stents
- Fecal transplants show promise as treatment for non-alcoholic fatty liver disease
- Café Scientifique: The invisible world inside us
- Using probiotics to protect honey bees against fatal disease
- Could microorganisms in poop help treat the deadliest form of skin cancer?
- Researchers find gut microbiome plays an important role in atherosclerosis
- Probiotics for respiratory tract infections could save Canada nearly $100 million a year