Search
Search
View St. Joseph’s Health Care London's 2017-2018 Annual Report
St. Joseph’s Health Care London’s 2017-2018 Annual Report features stories about patients and residents, and their journey of care and recovery.
The following research is highlighted in the 2017-2018 Annual Report:
- Smart tech, smart treatment: Many mobile applications are on the market to help people struggling with mental health issues, but these aren’t necessarily created or used by health care providers. Creating an entire smart mental health system is one of the strategic priorities of St. Joseph’s and Lawson’s Mental Health Research Group led by Dr. Cheryl Forchuk, Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery. Numerous projects have been identified as components of a plan spanning seven years.
- Walking while talking a possible early predictor of dementia: In a new study, researchers at Lawson and Western University are demonstrating that gait, or motion testing, while simultaneously performing a cognitively demanding task can effectively predict the progression to dementia and eventually help with earlier diagnosis. To date, there is no definitive way for health care professionals to forecast the onset of dementia in a patient with memory complaints.
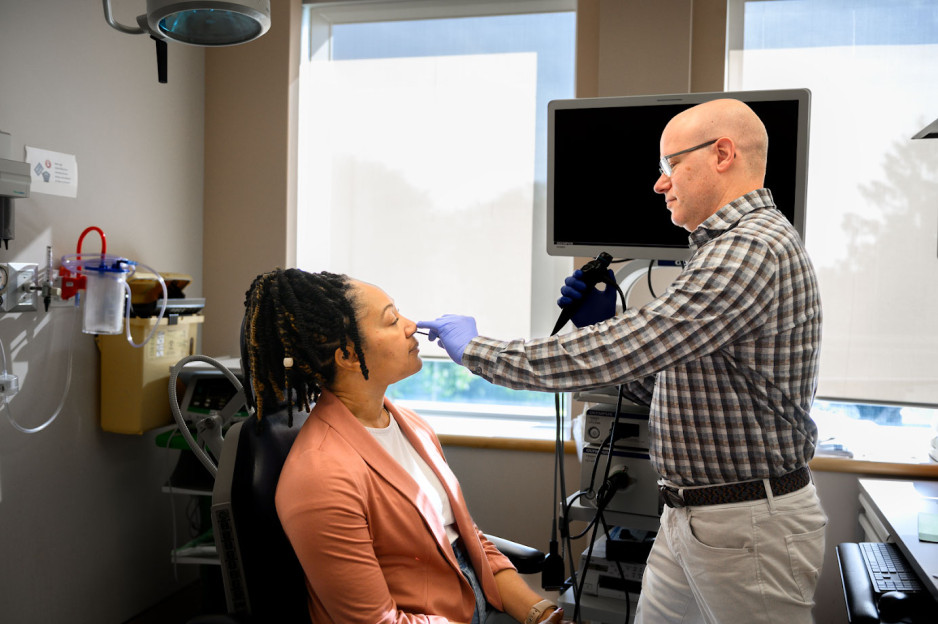
Viral mouth-taping trend ‘sus’ says Canadian sleep expert
Mouth taping, a growing trend on social media channels like TikTok, carries serious health risks, especially for those with sleep-disordered breathing and obstructive sleep apnea, according to a paper published in PLOS One.
The study from Lawson Research Institute (Lawson) of St. Joseph’s Health Care London, London Health Sciences Centre Research Institute (LHSCRI) and Western University’s Schulich School of Medicine & Dentistry also found no strong evidence of health benefits.
The trend involves placing tape over the mouth to stop ‘mouth breathing’ and promote breathing through the nose during sleep. It has been recommended by many social media influencers and celebrities who claim it can lead to better sleep, enhanced oral health and anti-aging results.
“It was concerning to us that celebrities and influencers are endorsing mouth taping without scientific evidence,” says Dr. Brian Rotenberg, researcher at Lawson, LHSCRI and Schulich Medicine & Dentistry. “In the language of social media influencers, it seemed a bit ‘sus,’ so we examined what science is telling us about this trend and whether or not it is safe.”
Rotenberg collaborated with Dr. Elise Graham, paediatric otolaryngologist head and neck surgeon at IWK Health and Jess Rhee a Schulich School of Medicine & Dentistry resident who is training at London Health Sciences Centre (LHSC) on the research. He and his team examined 86 existing scientific studies on the topic, including an in-depth review of 10 studies representing the experience of 213 patients. The team found mouth taping:
- Has no strong scientific evidence of health benefits, contradicting claims on social media.
- Can make existing sleep-disorder breathing worse by restricting airflow, putting additional stress on the respiratory system and increasing risk of suffocation when patients experience a nasal obstruction.
“Our research shows that taping the mouth shut during sleep is dangerous, especially among those who may not be aware they have sleep apnea,” adds Rotenberg, who is also an otolaryngologist and sleep surgeon at St. Joseph’s Health Care London and London Health Sciences Centre (LHSC). “These individuals are unknowingly making their symptoms worse and putting themselves at greater risk for serious health complications like heart disease.”
Rotenberg and his team point to the importance of health research in combatting misinformation and pseudoscience.
“It’s easy for misinformation to run rampant on social media; we’ve seen this countless times over the past few years,” says Rhee. “We need to make health decisions based on strong scientific evidence. Our hope is that people stop taping their mouths during sleep and recognize it is dangerous.”
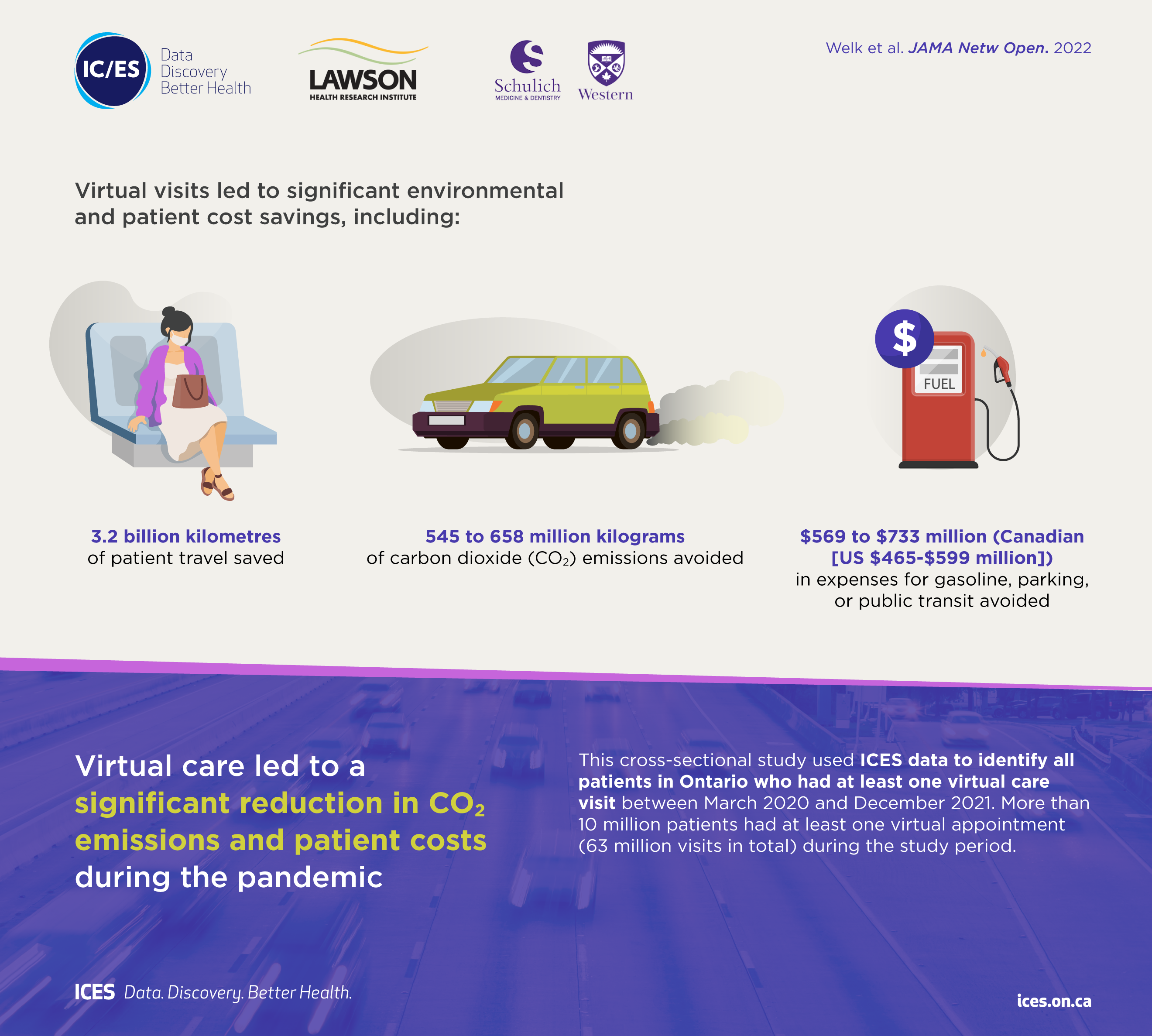
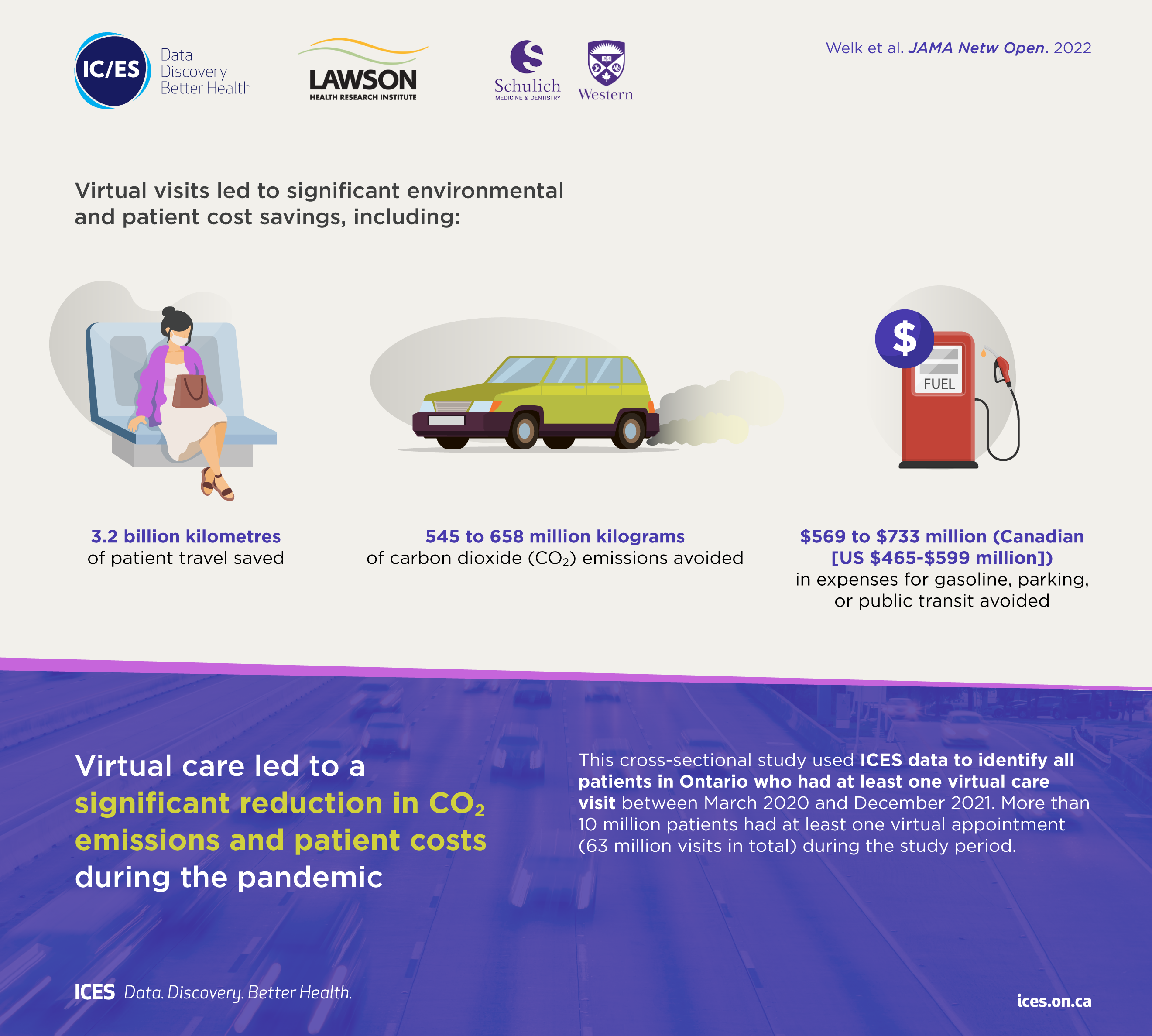
Virtual care associated with significant environmental and patient cost savings
London, ON - A new study by researchers at ICES, Lawson Health Research Institute and Western University finds that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs.
Prior to the pandemic, less than two per cent of patient visits with physicians took place virtually. The beginning of the pandemic (April-June 2020) triggered a rapid transition to virtual visits, which soared to 70 to 80 per cent, and then stabilized at 50 to 60 per cent of all physician visits.
This cross-sectional study published in JAMA Network Open used healthcare administrative data from Ontario, Canada to identify all patients with at least one virtual care visit between March 2020 and December 2021.
“Virtual care has become an important part of the healthcare system in Ontario, and in addition to improved patient convenience, it results in significant environmental and financial benefits for patients,” says lead author Dr. Blayne Welk, associate professor of surgery at Western's Schulich School of Medicine & Dentistry, urologist at St. Joseph’s Health Care London, associate scientist at Lawson, and adjunct scientist at ICES Western. “The financial and environmental benefits of virtual care will likely continue beyond the pandemic and are particularly relevant for some patients who were frequent recipients of virtual care.”
Findings show that for more than 10 million patients with at least one appointment during the study period (63 million visits in total), virtual care was associated with estimated savings of:
• 3.2 billion kilometres of patient travel;
• 545 to 658 million kilograms of carbon dioxide (CO2) emissions; and
• $569 to $733 million (Canadian [US $465-$599 million]) in expenses for gasoline, parking, or public transit.
The avoidance of carbon dioxide emissions during the pandemic due to virtual visits represented approximately 0.2 per cent of the total annual carbon dioxide emissions (150 megatons) from Ontario.
The number of virtual care visits was greater for those aged 65 and older, individuals with multiple health conditions, and those living in urban areas. Due to distance travelled, virtual care may offer more potential environmental benefits and patient cost savings for rural residents. Other factors, such as decreased time off work (given that some virtual visits can
be done during the day with little interruption to work) may have had additional benefits for some working adults and parents of young children.
“Virtual visits should not replace all in-person visits, but they are an important option that can enhance the care that physicians provide for patients,” says Dr. Alexandra Zorzi, a Paediatric Oncologist at Children’s Hospital at London Health Sciences Centre and Associate Scientist at Lawson. “Our findings suggest that physicians should continue to offer virtual care appointments when appropriate, especially for patients living in more remote areas and those that have barriers to accessing in-person health care.”
The study, “Association of virtual care expansion with environmental sustainability and reduced patient costs during the COVID-19 pandemic in Ontario, Canada” was published in JAMA Network Open.
Author block: Welk B, McArthur E, Zorzi AP.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
The Institute for Clinical Evaluative Sciences (ICES) is an independent, non-profit organization that uses population-based health information to produce knowledge on a broad range of health care issues. Our unbiased evidence provides measures of health system performance, a clearer understanding of the shifting health care needs of Ontarians, and a stimulus for discussion of practical solutions to optimize scarce resources. ICES knowledge is highly regarded in Canada and abroad, and is widely used by government, hospitals, planners, and practitioners to make decisions about care delivery and to develop policy. For the latest ICES news, follow us on Twitter: @ICESOntario
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Virtual care associated with significant environmental and patient cost savings
A new study by researchers at ICES, Lawson Health Research Institute and Western University finds that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs.
Prior to the pandemic, less than two per cent of patient visits with physicians took place virtually. The beginning of the pandemic (April-June 2020) triggered a rapid transition to virtual visits, which soared to 70 to 80 per cent, and then stabilized at 50 to 60 per cent of all physician visits.
This cross-sectional study published in JAMA Network Open used healthcare administrative data from Ontario, Canada to identify all patients with at least one virtual care visit between March 2020 and December 2021.
“Virtual care has become an important part of the healthcare system in Ontario, and in addition to improved patient convenience, it results in significant environmental and financial benefits for patients,” says lead author Dr. Blayne Welk, associate professor of surgery at Western's Schulich School of Medicine & Dentistry, urologist at St. Joseph’s Health Care London, associate scientist at Lawson, and adjunct scientist at ICES Western. “The financial and environmental benefits of virtual care will likely continue beyond the pandemic and are particularly relevant for some patients who were frequent recipients of virtual care.”
Findings show that for more than 10 million patients with at least one appointment during the study period (63 million visits in total), virtual care was associated with estimated savings of:
• 3.2 billion kilometres of patient travel;
• 545 to 658 million kilograms of carbon dioxide (CO2) emissions; and
• $569 to $733 million (Canadian [US $465-$599 million]) in expenses for gasoline, parking, or public transit.
The avoidance of carbon dioxide emissions during the pandemic due to virtual visits represented approximately 0.2 per cent of the total annual carbon dioxide emissions (150 megatons) from Ontario.
The number of virtual care visits was greater for those aged 65 and older, individuals with multiple health conditions, and those living in urban areas. Due to distance travelled, virtual care may offer more potential environmental benefits and patient cost savings for rural residents. Other factors, such as decreased time off work (given that some virtual visits can be done during the day with little interruption to work) may have had additional benefits for some working adults and parents of young children.
“Virtual visits should not replace all in-person visits, but they are an important option that can enhance the care that physicians provide for patients,” says Dr. Alexandra Zorzi, a Paediatric Oncologist at Children’s Hospital at London Health Sciences Centre and Associate Scientist at Lawson. “Our findings suggest that physicians should continue to offer virtual care appointments when appropriate, especially for patients living in more remote areas and those that have barriers to accessing in-person health care.”
The study, “Association of virtual care expansion with environmental sustainability and reduced patient costs during the COVID-19 pandemic in Ontario, Canada” was published in JAMA Network Open.
Author block: Welk B, McArthur E, Zorzi AP.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Walking the labyrinth: A path for meaning, insight and reflection
At Southwest Centre for Forensic Mental Health Care (Southwest Centre) in Elgin County, the unique story of every individual is honoured as care practitioners assist in the journey toward recovery. Part of the St. Joseph’s Health Care London family, Southwest Centre is devoted to caring for people with a mental illness who have also come into contact with the criminal justice system.
A new study by Lawson Health Research Institute shows that the use of labyrinths contributes to recovery by promoting spiritual self-care, insight development and personal meaning-making reflection. The research was co-authored by Lawson Allied Scientist and Certified Spiritual Care Practitioner at Southwest Centre, Stephen Yeo, along with his colleagues Dr. Clark Patrick Heard and Jared Scott, both Lawson Associate Scientists and Occupational Therapists.
“Research has demonstrated that labyrinth-walking can result in increased focus and calm, along with a reduction in blood pressure and stress,” explains Yeo. “Additionally, labyrinth-walking is narrative-driven and highly constructivist in nature, which promotes the opportunity for one to critically reflect on his or her unfolding story.”
This can be done in solitude or a trained facilitator can support important narrative reflection and invite opportunities for integration.
The process of reflecting and making meaning helps individuals to think about what they observed or did, why it mattered and how they might think or act differently based on new knowledge. This allows them to set goals and use what they’ve learned from the past to inform future action, and to consider the real-life implications.
Participation supports patients as they cope with mental illness, and the impact is magnified for individuals who have come into contact with the criminal justice system. Their experience can increase existential questions along with spiritual pain and distress.
Even in the most complex and difficult circumstances, walking the labyrinth facilitates a variety of coping approaches including:
- stress reduction and mindfulness;
- understanding one’s awareness of relationship with that which is sacred to them (transcendence) and the environment;
- development of ongoing personal narrative and meaning-making; and,
- kinesthetic prayer and meditation.
Unlike mazes that are like puzzles with many choices of path and direction, labyrinths are created using continuous lines and are easier to navigate with one route to and from the centre. There are two permanent labyrinths at Southwest Centre – one indoors and one outdoors. For the most part, the labyrinths are accessible for self-guided walking and, throughout the year, various group opportunities are scheduled for invited participation. This activity can be continued in the community, as there are labyrinths in various places across the province such as parks, faith communities and other health-care settings.
“Labyrinth participation supports themes related to hope, coping, resiliency, autonomy – all of which are significant contributors to recovery and the maintenance of well-being. Future research in this area could examine the benefits for different patient populations and also for those who reside in the community.”
Labyrinths are trans-religious and their application can be beneficial to religious and non-religious participants. They are also easy to maintain and can be installed in a variety of locations.
Along with his study co-authors, Yeo was honoured with the CASC Group Research Award from the Canadian Association for Spiritual Care. The award recognizes a CASC member who collaborates with other professionals in the research field of spirituality, religion and wellbeing. The recipient supports the core values of professional connection and interdependence, promoting positive relationship with colleagues of various professionals as well as clients.
“Given that this was my first foray into research at this level, I was very humbled to have been nominated for, and to have received, this award,” says Yeo. “I remain especially grateful to the professional guidance and support of my research colleagues.”
“Walking the Labyrinth: Considering mental health consumer experience, meaning making, and the illumination of the sacred in forensic mental health setting” was published in the December 2015 issue of the Journal of Pastoral Care and Counseling. This study is believed to be a first of its kind in a forensic mental health care facility.
Image

|
Left: Photo of the indoor labyrinth at the Southwest Centre for Forensic Mental Health Care. |
What happens to our bodies when we feel social emotions?
Feeling emotions based on the interactions we have with other people is a common part of daily life, yet we know very little about how these emotions are experienced in the body.
Chloe Stewart, a PhD candidate at Lawson Health Research Institute (Lawson) and Western University’s Schulich School of Medicine & Dentistry, has been awarded a Lawson Internal Research Fund (IRF) Studentship to conduct the first study to comprehensively explore the physical experience of social emotions. The study will be supervised by Dr. Elizabeth Finger, a Lawson scientist, neurologist at St. Joseph’s Health Care London’s Parkwood Institute, and associate professor at Schulich Medicine & Dentistry.
“We feel social emotions based on our awareness, interpretation or anticipation of the thoughts and feelings of others. For example, we feel embarrassment not only because we have done something potentially embarrassing, but also because we know that another person is aware of it, or could become aware of it. Other social emotions include pride, empathy and guilt,” explains Stewart.
“These are distinct from basic emotions, such as anger and happiness, which only require us to be aware of how we ourselves are feeling and can occur completely independently of other people. Whether it’s your heart beating faster when you’re angry or the lump in your throat when you’re sad, the ways that our bodies experience basic emotions are very well understood. However, we do not have a good understanding of what happens to our bodies when we feel social emotions,” she adds.
Unhealthy levels of certain social emotions are associated with many conditions, including certain kinds of dementia, obsessive compulsive disorder and psychopathy. The results of the study, which will be conducted at Parkwood Institute, could help in developing potential interventions or treatment approaches to restore these emotions to healthy levels.
The first phase of the study will look at the physical experience of social emotion in healthy adults. Noninvasive electrodes will be attached to participants’ torso, hands and throat. The electrodes are connected by wires to receivers, which in turn send signals to a computer. The researchers can assess how the signals change based on the stimulus the participant is looking at. Stewart expects the emotions will influence several different physical responses, including heart rate, swallowing rate and movement of the stomach muscles.
The research team will then extend the study to patients with frontotemporal dementia, which can impair social functioning. They will compare the physical experience of social emotions in these participants to participants with Alzheimer’s disease and dementia with Lewy bodies. Patients with Alzheimer’s disease or dementia with Lewy bodies usually have healthy levels of social emotions, but those who have dementia with Lewy bodies often have impaired physiological functioning while those with Alzheimer’s do not.
Their goal is to compare how social emotions look in healthy adults to what happens in the body when social functioning is impaired.
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
What is ICES Western? Q&A with Dr. Amit Garg
As ICES Western recruits a new Site Director, Dr. Amit Garg, who currently holds the position, sat down to talk about the importance of the work being done. Dr. Garg is also a Scientist at Lawson Health Research Institute, Nephrologist at London Health Sciences Centre (LHSC) and Professor at Western University’s Schulich School of Medicine & Dentistry.
What is your role with ICES Western?
Starting in 2009, I supervised the team responsible for the ICES Western build over an approximately three-year period. Since then, I have spent the last decade serving as the inaugural Site Director for ICES Western.
Can you briefly describe the work that ICES Western does?
For those people who don't know, ICES is a province-wide non-profit research institute, founded in 1992, that is focused on translating data into trusted evidence. Our community is comprised of world-class research, data and clinical experts who evaluate health care delivery and population outcomes.
ICES scientists and staff (currently about 570 in Ontario) and trainees (currently about 700) access a vast and secure array of Ontario’s demographic and administrative health-related data. ICES currently has 108 linked data holdings (with over one trillion data points), and the amount of data that ICES has available for use in research grows each year. The linked data include vital statistics, hospital services, physician claims, drug benefits, laboratory results, biosamples and immigration records. Our research, including 1,200 active investigator-initiated projects, is focused on making health policy and health care better, and people healthier.
ICES Western is physically located at LHSC’s Victoria Hospital and is one of seven ICES satellite sites across Ontario. The site’s development is an ongoing partnership between LHSC, St. Joseph’s Health Care London, Lawson, the Academic Medical Organization of Southwestern Ontario (AMOSO) and Western.
How does ICES’ work impact research being done in Ontario and across Canada?
ICES Western is a core facility that researchers use for research, training and decision support. Organizations such as our local hospitals and public health agencies make requests for decision support through a procedural mechanism called Applied Health Research Questions.
Over the last two years, our researchers have conducted a great deal of COVID-19 research. Several projects at ICES Western have examined vaccine effectiveness and spread of the virus. Investigators have used a data-driven approach to help protect people experiencing homelessness in Ontario. Another study quantified the impact of COVID infections on physicians, including how many of them became ill, were hospitalized and received care in the intensive care unit.
Research done through ICES Western has led to important changes in health care. For example, Health Canada instituted labeling requirement changes based on drug safety studies done through ICES.
Why is this work so important?
We all want better health outcomes for citizens, both in Ontario and throughout the world. Ideally, we want people to live longer, healthier lives without needing many health care resources, and we want that to be done in an equitable fashion. There is a substantial amount of research needed in multiple areas to achieve this goal. ICES provides a cutting edge infrastructure to enable this work.
What kind of researchers are involved with ICES?
At ICES Western we support a whole host of individuals and entities as they conduct research. Health care delivery organizations and health agencies including LHSC, the Ontario Renal Network and Trillium Gift of Life Network use knowledge received through reports completed at ICES. Our typical individual investigators include both basic science and clinical investigators. We also support trainees in the areas of epidemiology and statistics, as well as many other fields of study, such as computer science and geography. These are all students who have an interest in working with ‘big’ data. Finally, we have personnel that work with privacy, data, analysis, epidemiology and more.
What do you see in the future for the organization?
We've made a lot of progress in the last 10 years and I can't wait to see what's going to happen in the future. We're still just scratching the surface in terms of what's possible. While what we have done in building this site and supporting important research is impressive, in terms of the possibilities – the sky's the limit. There is so much opportunity around new research and trial methodologies, new insights and new evaluation techniques. I expect ICES Western will continue to develop, enabling a growing number of people to make a large impact. I see ICES continuing to contribute to a world where people live longer, healthier lives.
What is the most important thing people should know about ICES?
How enabling it is. It's time well spent to really understand what is and is not possible with ICES data and research expertise. Once you invest in it – really spend your time and energy to understand the potential– you start realizing all of these opportunities that would not be possible otherwise. With more than a thousand research studies underway across all ICES sites, we have great discoveries ahead to shape the future of health care in Ontario.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email