Search
Search
This will be a huge benefit for society because sepsis is the leading cause of death worldwide
It’s a discovery that has been more than ten years in the making: the use of a human protein to potentially treat patients with sepsis.
Lawson Scientist Dr. Qingping Feng noticed that a human protein called annexin A5 showed positive results with sepsis back in 2007.
Fast forward 14 years later to now, and this discovery could very well be the first ever viable treatment for sepsis patients, including severe COVID-19 patients who develop sepsis. “With COVID initially, it is in the airway and then in the lungs, then from there the inflammatory response in fact spreads to the whole body,” says Dr. Feng, Ivey Chair in Molecular Technology at Western University's Schulich School of Medicine & Dentistry. “Sepsis causes major organ dysfunction and carries a high mortality unfortunately.”
It has become a challenging issue for Intensive Care Physician at London Health Sciences Centre (LHSC), Dr. Claudio Martin, who can only do so much to treat severe COVID-19 patients that develop sepsis.
“What we have seen is a very primary severe respiratory failure to the lungs for severe COVID patients,” says Dr. Martin, Associate Scientist at Lawson. “We have used steroids and other treatments to try to help, but the results and effects aren’t dramatic and we see patients who have these treatments and still progress and end up in the ICU.”
However, Dr. Feng and his team has found in a pre-clinical study, that annexin A5 can inhibit inflammation, improve organ function, and survival when treating sepsis.
Another potentially deadly situation for COVID-19 patients is cell death and blood clots, specifically near the lungs. The good news is that the research team also believes the annexin A5 drug will prevent these complications through the drugs anti-apoptotic (cell death prevention) and anti-coagulant (blood clot prevention) properties.

Supported by provincial funding through Ontario's COVID-19 Rapid Research Fund, the research team has launched a clinical trial with critically ill COVID-19 patients at LHSC, using a manufactured form of annexin A5. The goal is to enroll a total of 60 patients for the clinical trial, and enrollment has already begun. “Patients are receiving standard treatment and then those enrolled will also receive the annexin,” says Dr. Martin. “It’s a placebo blinded clinical trial, so patients will either get a lower dose of annexin, a higher dose of annexin, or a placebo.”
If the clinical trial shows promising results, Dr. Feng says the team plans on expanding into a larger phase three trial with not just COVID-19 patients with sepsis, but other sepsis patients as well. “If in fact annexin A5 is shown to be effective in sepsis, then this will be a huge benefit for society because sepsis is the leading cause of death worldwide.”
The drug is currently being produced through a partnership with Suzhou Yabao Pharmaceutical R&D Co., Ltd., based in China, Lawson Health Research Institute, and WorldDiscoveries. “Our long-standing partnership with Suzhou Yabao has enabled annexin A5 drug development to proceed to this point,” says Kirk Brown, Manager of Business Development, Lawson Health Research Institute. “We are now in a unique position through this trial to offer a potential life-saving treatment for this emergent global disease, with the objective of soon expanding to all cause septic patients.”
Tim Doherty
Tim Doherty, MD; PhD
Professor, Schulich School of Medicine and Dentistry
Neuromuscular Function
Dr. Tim Doherty is a physiatrist and is the Chair/Chief of the Physical Medicine and Rehabilitation department at Parkwood Institute and a Professor in the Schulich School of Medicine and Dentistry at Western University. Dr. Doherty completed a PhD in kinesiology at Western University in 1993 and residency training in in Physical Medicine and Rehabilitation at McMaster in 2000.
Dr. Doherty is a past President of the Canadian Association of Physical Medicine and Rehabilitation, examiner for the Canadian Society of Clinical Neurophysiology, Associate Scientist at the Lawson Health Research Institute and is a member of the Editorial Boards of Muscle and Nerve, and the Journal of Clinical Neuromuscular Disease. Dr. Doherty is a renowned expert in the study of mobility and pioneered the development of quantitative electromyography (EMG) techniques that have been employed to study aging, motor neuron disease and peripheral neuropathies.

Time for Canada to reclaim its place as a leader in scientific discovery
The following editorial was provided to Post Media by Dr. David Hill, scientific director, Lawson Health Research Institute.
Last week the Nobel Prizes for 2017 were announced, recognizing incredible advances in science that will impact all our lives for the better. If you were looking for Canadian scientists amongst the teams, you would be disappointed.
According to a federal government report commissioned by the minister of science titled Investing in Canada’s Future — Strengthening the Foundations of Canadian Research and released in April, Canada’s momentum in the sciences has never been worse.
Our country’s investment in key emerging areas such as artificial intelligence, clean technology, nanotechnology, immunotherapy, bioinformatics or bio-engineering is flat-lined or declining, and falling seriously behind competitor nations.
We are not talking about matching the United States or Germany. Canada invests less in science research and development relative to gross domestic product than does Taiwan or Singapore.
Why should we care?
Because smart science delivers technologies we take for granted every day, such as Siri on our iPhones, minimally invasive surgery and secure online banking.
Science also creates companies, delivers high-paying and rewarding jobs, and is the backbone of the economy.
In London, Ont., jobs that depend on advancing science include those at Lawson Health Research Institute, the research institute of London Health Sciences Centre and St. Joseph’s Health Care London and where I work; academic institutions such as Western University and Fanshawe College; and local businesses generating health devices, computer software and engineered products. A lack of investment in science could be devastating to our city.
This report places the failure to invest in science at the door of successive federal governments during the past decade.
Of course, it is not only government that should invest in science. It is industry that takes proven scientific findings and translates them into products we all consume.
But these innovative products need to start somewhere, most often in the laboratory. Fostering high risk, fundamental discovery science should be a core responsibility of government in a knowledge-driven economy.
In Canada, the contribution of federal funds to discovery science is now below 25 per cent of the total research investment, and lower than most of our competitor nations. Consequently, research funds are scarce, laboratories are closing, fewer students are receiving advanced training, and fewer new businesses are emerging.
It is not too late.
The report provides evidence to show that Canadian scientists are still respected leaders in their fields. The engine simply needs fuel.
To return Canada’s discovery science enterprise back to 2006 productivity levels, we require an additional investment of $1.3 billion during four years, representing 0.1 per cent of the entire federal budget for each of those years.
The investment quickly pays for itself. Every $1 invested in fundamental research has been calculated to return $2.20 to $2.50 in direct and indirect economic activity.
Next year’s federal budget is being put together right now in Ottawa, and we have an opportunity to reclaim our past reputation as a discovery nation; a nation that brought the world insulin, the Canadarm, Pablum, canola and the electron microscope.
The journey toward that next Canadian Nobel Prize needs to start now.
Dr. David Hill
Scientific Director
Lawson Health Research Institute
Tom Miller
Tom Miller, MD
Associate Professor, Schulich School of Medicine and Dentistry
Neuromuscular Function
Dr. Thomas Miller is a physiatrist at Parkwood Institute and an Associate Professor in the Schulich School of Medicine and Dentistry at Western University in the Department of Physical Medicine and Rehabilitation. Dr. Miller completed his medical degree at Queen’s University in 1989, and then completed subsequent training in physical medicine & rehabilitation at the University of Ottawa and a fellowship in clinical neurophysiology at University of New South Wales in Australia.
Dr. Miller is the Medical Director of the neuromusculoskeletal rehabilitation program at Parkwood Institute, Director of the Electrodiagnostic laboratory, consultant physiatrist with the Hand and Upper Limb Centre. He is also the co-director of the Peripheral Nerve Clinic at Parkwood Institute, a multidisciplinary assessment and treatment program for major nerve injury. Specific areas of academic research include peripheral nerve injury and its rehabilitation, spasticity rehabilitation and the neurophysiological assessment of function and mobility.
Tomorrow’s scientists tour Lawson research facilities
A group of senior chemistry students from H.B. Beal Secondary School visited Lawson Health Research Institute (Lawson) facilities at St. Joseph’s Hospital on Wednesday, November 8. In addition to learning about Lawson’s world-renowned imaging research, the group toured the Cyclotron and PET Radiochemistry Facility and Dr. Alexandre Legros’ brain stimulation lab.
The students first learned about Lawson’s simultaneous PET/MRI – the first in Canada – and its associated research. Led by Dr. Jonathan Thiessen, Lawson imaging scientist, the presentation focused on the benefits of combining Positron Emission Tomography (PET) with Magnetic Resonance Imaging (MRI) across multiple disciplines.

Above: Dr. Jonathan Thiessen discusses Lawson's simultaneous PET/MRI
Benjamin Wilk, a PhD candidate working under Dr. Thiessen’s supervision, presented on his research which is focused on developing methods to image the heart after myocardial infarction, or heart attack, using PET/MRI. Qi Qi, another of Dr. Thiessen’s PhD candidates, discussed his research that looks at multimodal imaging to evaluate tumour perfusion and glycolysis in brain tumours.
"It is an incredible opportunity to present our work to high school students,” said Dr. Thiessen. “By seeing examples of the research happening in their own community, my hope is that some of them will be inspired and work hard to become the scientists and healthcare professionals of tomorrow."
The students were then split into two tour groups. The first group toured Lawson’s Nordal Cyclotron and PET Radiochemistry Facility with the facility’s director, Dr. Michael Kovacs; Jeff Corsaut, engineer; and Dr. Justin Hicks, Lawson imaging scientist.

Above: Dr. Justin Hicks provides a tour of The Cyclotron and PET Radiochemistry Facility
The Cyclotron and PET Radiochemistry Facility is used to produce positron-emitting radiopharmaceuticals (PERs). PERs are injected into patients undergoing a positron emission tomography (PET) scan. The half-life of the radioactive isotopes in PERs is short, which necessitates generating them with a cyclotron that is in close proximity to the clinic where they are used.
The students learned how PERs are produced in the Cyclotron and research being conducted with PERs to advance imaging of complex diseases.
The second group toured Dr. Alexandre Legros’ brain stimulation lab which is part of the Bioelectromagnetics and Human Threshold Research Group at Lawson. Dr. Legros’ research focuses on the effects of specific electromagnetic stimuli - from deep brain stimulation to power-frequency magnetic fields - on human brain processing, motor control and cognitive functions. The students were guided by lab manager, Michael Corbacio, and postdoctoral scholar, Dr. Sebastien Villard.

Above: Dr. Sebastien Villard (second from right) and Michael Corbacio (far right) provide a demonstration of research being conducted in Dr. Alexandre Legros' Bioelectromagnetics and Human Threshold Research Group
The two groups of students then traded places, touring the facility they had not yet visited.
“The H.B Beal senior chemistry class was impressed and grateful with the opportunity to visit the facilities at Lawson Health Research Institute,” said Andrew Holmes, the class’ teacher and head of science at H.B. Beal. “The presentations, cyclotron tour and research lab gave students some valuable insight into some of the roads available to them with a scientific path in education. Students were particularly impressed with how enthusiastic and excited the researchers were in talking about their work at Lawson, and came away with a very positive view of scientific career paths.”
Tools or Products of Research
Tools
Credit and Source: Dr. Joy MacDermid (@email).
- PREPS - Over-night stay
- Shoulder Joint Protection Program (digital version)
- Shoulder Joint Protection Program (print version)
- HULC Shoulder Movement Analysis Mediapipe (test version)
- Miller J, Gross A, MacDermid J, COG, ICON. Should I receive manual therapy and exercise for my neck pain?: A patient decision aid (2012).
- Miller J, Gross A, Rogers T, Willemse J. Manual Therapy and Exercise for Neck Pain: Clinical Treatment Tool-kit (2012).
- Credit and Source: Dr. Joy MacDermid (@email).
Critical Appraisal
Protocols
- FIT- HaNSA (The Functional Impairment Test-Head, and Neck/Shoulder/Arm) Protocol
- This test is a functional endurance test that assesses tasks of the upper limb performed in a standardized way over 15 minutes.
Credit and Source: Dr. Joy MacDermid (@email).
- This test is a functional endurance test that assesses tasks of the upper limb performed in a standardized way over 15 minutes.
- Cold Stress Test and The Ten Test Manual
- Two simple quantitative sensory tests (youtube.com)
- The Cold Stress Test is a standardized cold test that measures pain and vascular response to cold immersion.
Credit and Source: Dr. Zakir Uddin (@email) ) & Dr. Joy MacDermid (@email).
Knowledge Translation
- Pain+
- Free resource on pain evidence to support your clinical decisions
- Free resource on rehab evidence to support your clinical decisions
Please note: if you require an accessible version of files on this page, reach out to us at @email as work is currently underway to code the files attached here.
Top 12 research stories of 2022
As the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, our teams impact the lives of people in Ontario, Canada and around the globe with groundbreaking studies, world firsts and translational research that enhances care, health and wellbeing. Here are some of Lawson Health Research Institute’s top research highlights of 2022.
Researchers looking to better personalize treatment for PTSD

In a new study through Lawson and Western University’s Schulich School of Medicine & Dentistry, scientists are looking at a form of treatment called deep brain reorienting (DBR) for those suffering from post-traumatic stress disorder (PTSD). Read more.
Virtual care associated with significant environmental and patient cost savings

A new study by researchers at ICES, Lawson and Western finds that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs. Read more.
Novel test that could easily diagnose blast injury created by local scientists

In a world first, researchers at Lawson and Defence Research and Development Canada have developed a breath test that could be used to diagnose repetitive blast injury – a mild traumatic brain injury resulting from pressure changes that occur during explosions. The device will soon go through clinical trials to validate its efficacy. Read more.
Local researchers using artificial intelligence to lead the way in bedside lung imaging
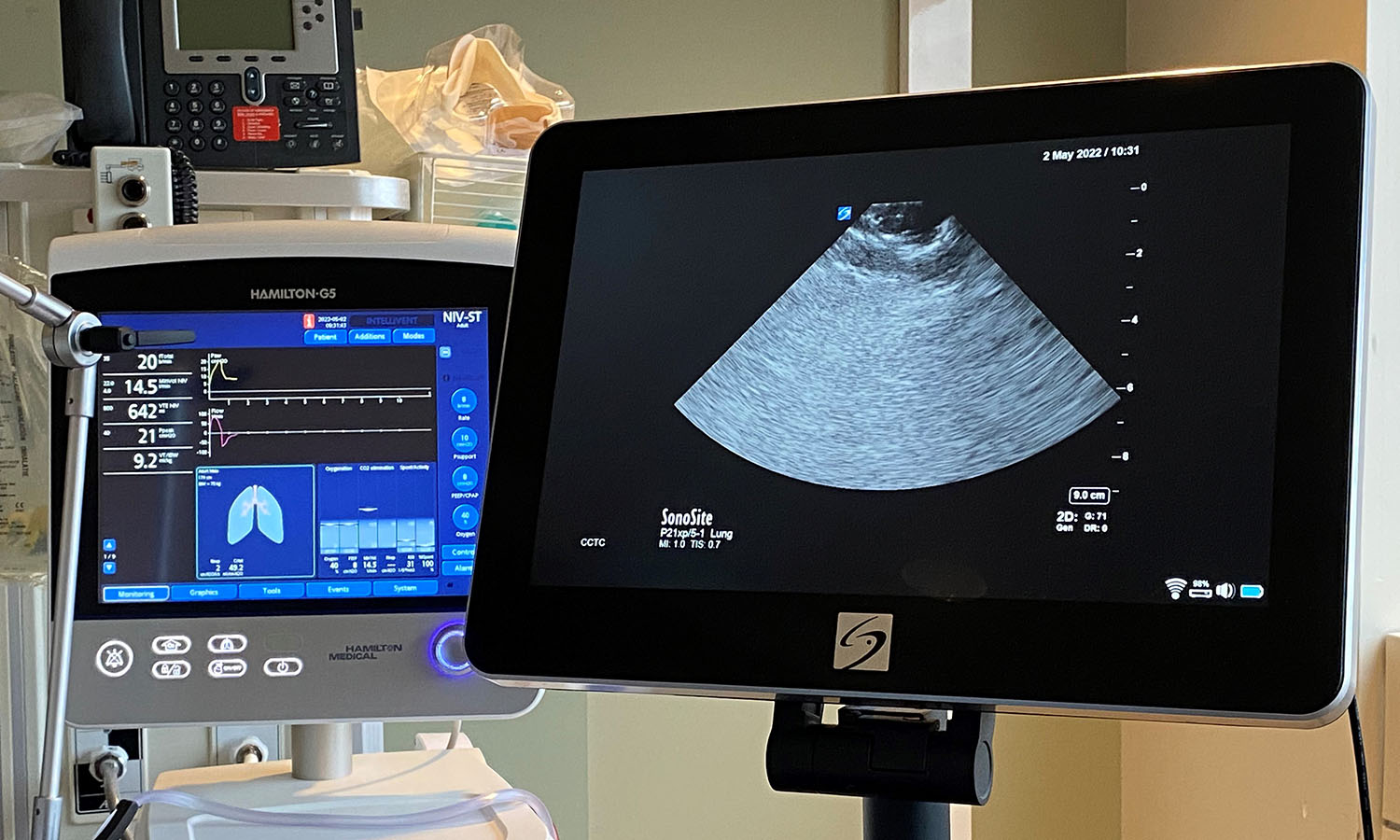
A team at Lawson is testing a new form of artificial intelligence (AI), paired with portable ultrasound machines, to image and identify lung concerns in real time, right at the beside of critically ill patients. Approximately 100 critical care patients at LHSC will be part of this study. Read more.
New tool shows promise in helping people manage traumatic brain injuries one pace at a time

A team at Lawson has developed a new app called MyBrainPacer™ which aims to better assist and treat those living with mild traumatic brain injuries (mTBI), including concussions. mTBI may come with lasting effects that can alter a person’s life. Although a person with a mTBI may appear fine on the outside, many have to pace their day-to-day activities in order to allow the time needed for the brain to properly heal. Much like point tracking used by dieters to monitor food choices, through MyBrainPacer™ App, users can assign values to tasks like driving, grocery shopping, screen use and exercise so they can plan and pace their daily activity. Read more.
Study shows a decline in Veterans' mental health throughout the pandemic

When it comes to mental health conditions, Veterans are an at-risk population, often having higher rates of depression and post-traumatic stress disorder (PTSD). When the COVID-19 pandemic hit, scientists at Lawson wanted to understand its effects on this already at-risk population. They found that more than half of Canadian Veterans reported a decline in their mental health. Read more.
Growing evidence that PSMA imaging improves prostate cancer detection
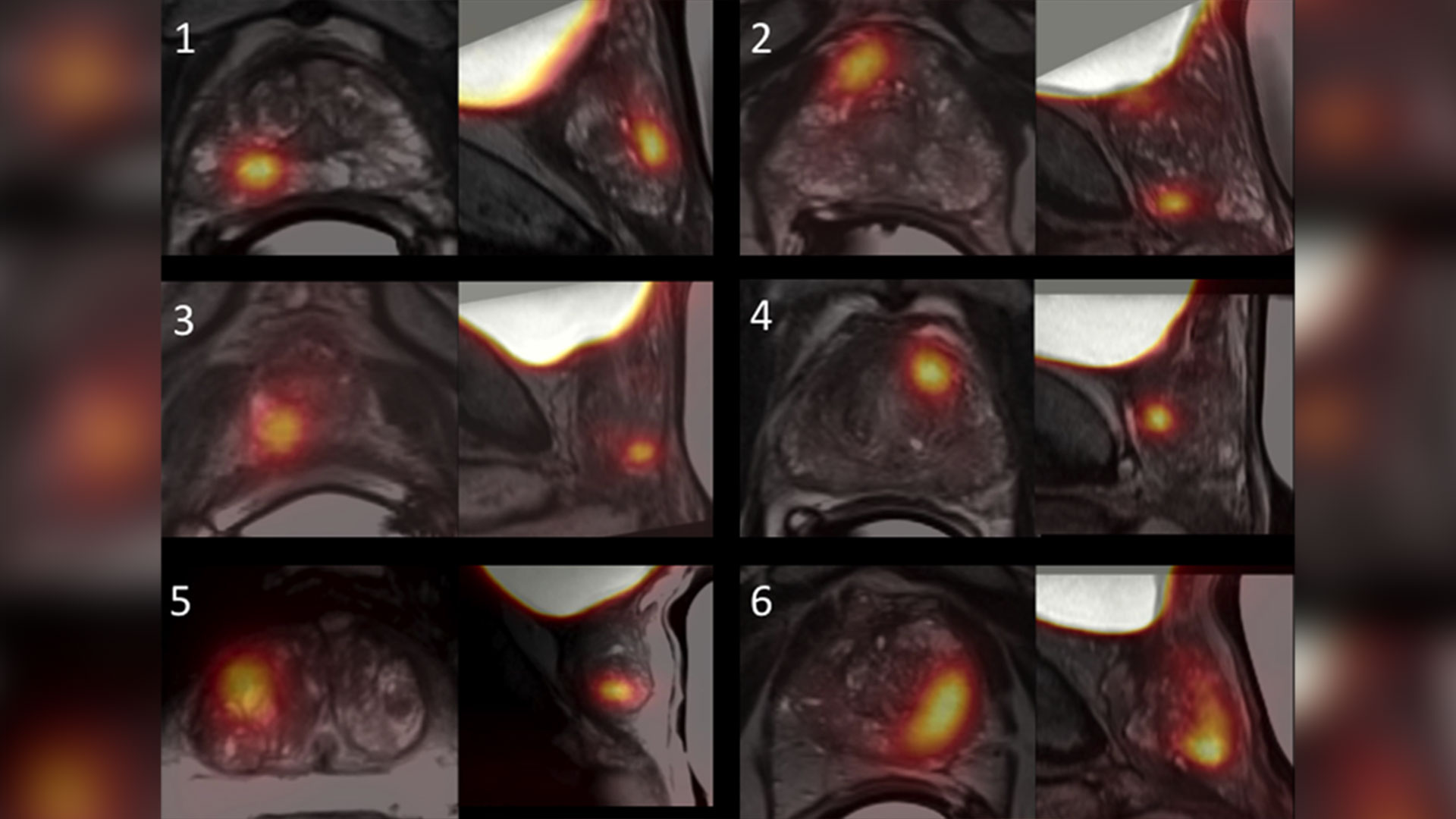
Scientists at Lawson are leading the way in using specialized imaging to detect prostate cancer – the fifth leading cause of cancer death in men around the world. Early evidence indicates that PSMA PET scans have changed how prostate cancer is being treated, but more work is underway to understand the impact of those treatment changes. Read more.
Leveraging virtual reality to manage pain in paediatric patients

A study underway through Lawson and Children’s Hospital at LHSC is using virtual reality (VR) to help paediatric patients during painful and distressing procedures. The study is focusing on paediatric patients who need port access. A port is a little reservoir that sits underneath the skin that allows access to blood or medication with the use of a needle. Ports are most commonly used in paediatric cancer patients. Read more.
Team players: FMT and microbiome research could have widespread impact

There is still much to learn about the human microbiome and its role in fighting disease, but ongoing studies at Lawson, including a focus on fecal microbial transplants (FMT), are making strides in harnessing this complex system. FMT is being studied in connection with conditions as varied as non-alcoholic fatty liver disease, rheumatoid arthritis, atherosclerosis, HIV, cancer and multiple sclerosis. Read more.
London researchers adapt MRI technology to image salt within the kidneys

Scientists at Lawson have adapted PET/MRI technology to accurately image salt within the kidneys of patients with kidney disease. Imaging salt within the kidneys has never been accurately accomplished in patients with kidney disease, but Dr. McIntyre and his team developed new technology and software that was adaptable to a PET/MRI machine at St. Joseph’s. Read more.
London researchers discover novel method to diagnose long COVID
Published in Molecular Medicine, researchers at Lawson have found that patients with post-COVID-19 condition (long COVID) have unique biomarkers in their blood. The team is now working on developing a first of its kind blood test that could be used to diagnose long COVID. The discovery could also lead to new therapeutics for this condition. Read more.
Largest trial ever done in hemodialysis care examines optimal dialysis temperature

Published in the Lancet findings from a large clinical trial through Lawson, ICES Western and Western University suggest that lowering dialysis temperatures does not lead to improved patient outcomes, despite previous studies suggesting otherwise. Read more.
To learn more about Lawson research studies, please visit our News and Media page
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Two Lawson researchers each receive $400K CIHR grants to improve kidney care
Two researchers at Lawson Health Research Institute have each been awarded $400,000 as part of the Canadian Institute of Health Research’s (CIHR) new Health System Impact Embedded Early Career Researcher Awards.
The funding will see the researchers apply their skills to find and implement solutions to improve kidney care by focusing on challenges in the health-care system.
Dr. Kyla Naylor and Dr. Danielle Nash will each spend four years working with provincial organizations. Dr. Naylor will work with the Trillium Gift of Life Network -Ontario Health, which is the organization responsible for coordinating provincial organ and tissue donation and transplant services. Dr. Nash will work with the Ontario Renal Network - Ontario Health, which is the organization responsible for managing delivery of advanced kidney services in the province.

“The treatment options for kidney failure is either a kidney transplant or dialysis. The majority of Canadians who have kidney failure receive dialysis,” says Dr. Naylor, who is an Associate Scientist at Lawson and an Adjunct Scientist at ICES. “However, a kidney transplant compared to dialysis can improve a patients’ quality of life, can give on average 10 more years of survival, and when compared to dialysis, can save the health-care system millions of dollars.”
In her research program, Dr. Naylor will begin by developing a kidney transplant measurement framework that will enable continuous performance monitoring and increase equitable access to transplant.
“The first goal of this project will allow kidney transplant centres and regional renal programs to evaluate their performance and set goals towards improvement,” Dr. Naylor says. “The second is to improve kidney transplant education materials to provide patients with the information to make an informed decision about kidney transplant, and the third is to address geographical barriers to transplantation.”
Dr. Naylor will be using ICES data, which includes administrative health-care data for Ontario’s 14.5 million residents, with the goal of eventually making access to kidney transplantation more equitable for the thousands of Canadians living with kidney failure.
The goal of Dr. Nash’s research program is to use a learning health system model to better understand patient-identified gaps in kidney care across Ontario, and to develop solutions to fill these gaps in collaboration with the Ontario Renal Network and patient partners.
“Chronic kidney disease is a serious illness that can lead to kidney failure. The best way to prevent kidney failure is to detect chronic kidney disease early and provide optimal care during this time,” explains Dr. Nash, who is also an Epidemiologist and Scientist with London Health Science Centre’s (LHSC) Kidney Dialysis and Transplantation Program. “Since many patients do not have symptoms, it can go unnoticed for a long time. However, it can be detected using simple blood and urine tests.”
Province-wide data from ICES Ontario and the Ontario Renal Network will be used for the research data.
As part of both studies, the researchers will also be interviewing health-care providers and patients to assess additional barriers to treatment.
“One in four patients do not see a nephrologist in a timely manner and 60 per cent are not receiving adequate time in multidisciplinary kidney care clinics before initiating dialysis,” says Dr. Nash. “Education on treatment options (typically dialysis or a kidney transplant) needs to happen early for patients who are at high risk for kidney failure, so they can make an informed decision about treatment.”
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
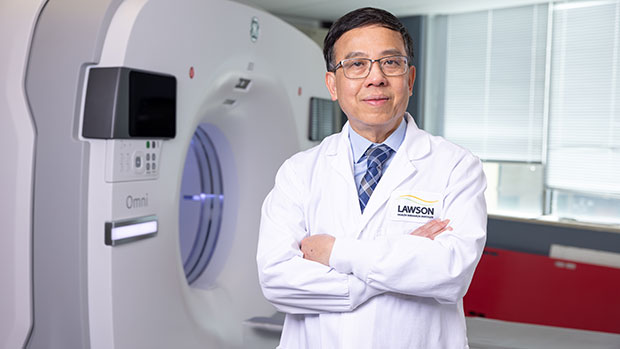
Two new research chairs announced for imaging
In a historical-first, St. Joseph’s Health Care Foundation and Western University announced two research chairs that are a critical step toward new approaches in imaging research and patient care in London and around the world. The combined value of both innovative new research chairs is $6.5M, which will be endowed in perpetuity to advance imaging research at Western University and Lawson Health Research Institute.
The research chairs have been named after the two scientists who are revolutionizing health care through their groundbreaking imaging research – Drs. Ting-Yim Lee and Frank Prato.
“These Chairs build on the legacy of exceptional imaging leadership across our academic, research and healthcare organizations. They are a critical step towards new approaches in medical technology and hospital-based research that will revolutionize patient care,” says Dr. Gillian Kernaghan, President and CEO, St. Joseph’s Health Care London.
Research teams in the city are using state-of-the-art imaging technology to help clinicians better predict and diagnose illnesses before their unset. And uncover why, and how, illness forms to one day find a cure to some of the most devastating diseases in the world.
“We’ve come to know medical imaging as one of the cornerstones of innovation and discovery at Lawson, and the two new research chairs represent two monumental leaps forward in the field of imaging research,” adds Dr. David Hill, Lawson Scientific Director.
The Ting-Yim Lee Chair in Cardiac Computerized Tomography (CT) Imaging Research has been established through the generosity of Ting-Yim and Maggie Lee and a joint funding collaboration between St. Joseph’s Foundation and Western University.
Dr. Ting Yim Lee is a scientist and professor of the Schulich School of Medicine & Dentistry, medical physicist at St. Joseph’s Health Care London and a scientist with Lawson’s Imaging program. Through his leadership, The Ting-Yim Lee Chair in Cardiac Computerized Tomography (CT) Imaging Research will transform the way clinicians diagnose, and prevent, severe tissue damage in persons who have experienced a cardiac event.
“Over the past 28 years, St. Joseph’s and Western have created opportunities for me and supported my research endeavor in many ways. I feel this gift is the best way to repay the help that I have received. We are onto something that is worthwhile and successful. By setting up this Chair, there would be a significant person – a clinician-scientist – to lead the next phase of the cardiac CT program. I am really humbled that the institutions see the value in this research and have contributed to guarantee that we have the necessary leader to carry forth this development,” says Dr. Lee.
This Chair represents the next phase of CT imaging research, focused on developing software and new methods that will save people’s lives.
The Dr. Frank Prato Research Chair in Molecular Imaging has been established to further enhance scientific understanding in the specialty of molecular imaging – building upon St. Joseph’s internationally-recognized leadership in imaging excellence.
Dr. Frank Prato is a scientist and professor of the Schulich School of Medicine & Dentistry, Chief Medical Physicist at St. Joseph’s Health Care London and the Founder and Program Leader of Lawson’s Imaging Program. Through his visionary leadership, The Dr. Frank Prato Research Chair in Molecular Imaging will improve the way clinicians effectively diagnose disease and actively correct the course of treatments in real time for life-threatening illnesses.
“I am truly honoured to have this Research Chair in Molecular Imaging named after myself. Over the past 40 years I have been privileged to work with outstanding people and incredible resources. Today Medical Imaging has become a cornerstone of care at St Joseph's Hospital. Here at St Joseph's we realize patient stewardship includes research as an essential part of the patient care continuum and that discovery, through research, leads to improved patient care. The holder of this chair will help lead us into the next frontier of medical imaging directly benefiting our local, national and global communities,” says Dr. Prato.
This Chair represents the next phase of precision medicine using molecular imaging to distinguish between varying forms of dementias, cancers, and to detect the early onset of cardiac disease and diabetes before symptoms emerge.
“With this historic announcement, we are marking a new phase of partnership and collaboration between our institutions and celebrating the generosity of donors who have helped create two significant research chairs,” explains Dr. Amit Chakma, President and Vice-Chancellor, Western University. “Together we will ensure that London remains at the forefront of medical imaging research and teaching.”
These Chairs will also have a greater role to play in the local health care community by attracting, and retaining, the research talent needed to innovate the way London’s hospitals and Western tackle the most pressing health issues Canadians face today.
Understanding the COVID-19 virus through health research
In the early months of the COVID-19 pandemic, there was little known about the virus that was causing the COVID-19 illness. Hospital researchers in London, Ontario, through Lawson Health Research Institute, quickly got to work to study and better understand the SARS-CoV-2 virus. Lawson is the research arm of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London.
“When the pandemic hit, we were well prepared in London to start research studies. We had existing expertise, laboratories and teams through the hospitals, Lawson and Western University that could be mobilized quickly,” explains Dr. Douglas Fraser, Critical Care Physician at LHSC and Scientist at Lawson. “Patients started coming to hospital with COVID-19 and we began research that involved collecting human samples and bringing them to the lab for analysis.”
Dr. Fraser, who is also a Professor at Western’s Schulich School of Medicine & Dentistry, led the research team studying the samples from COVID-19 patients in hospital. “We learned very quickly that COVID-19 patients were experiencing a strong inflammatory response to the virus. We looked at the molecules involved because many of these are signaling molecules to the immune system.”

Dr. Douglas Fraser, Critical Care Physician (LHSC) and Lawson Scientist
“By studying the molecules, we were able to determine the pathways. This is important because it also points to how we should be targeting our diagnostics and therapeutics,” adds Dr Fraser.
As a hospital research institute, Lawson is uniquely positioned to address the medical questions posed by a new virus. Its Clinical Research Services (LCRS) and Center for Clinical Investigation and Therapeutics (CCIT) teams responded rapidly when researchers initiated COVID-19 studies, including Dr. Fraser’s study to examine the immune response in patients with COVID-19.
“Starting a clinical trial usually takes a certain amount of time to put together, but the pandemic created a perfect storm,” explains Sue Tereschyn, Manager of LCRS at Lawson. “Clinical researchers had to develop studies at a speed they have never seen, and they needed implementation support at the same speed. In Dr. Fraser’s case, we needed samples from the Intensive Care Unit (ICU) and we were processing samples from COVID-19 patients seven days a week. A high level of skill was needed.”
Dr. Fraser and his team soon became the first in the world to understand the immune response and several pathophysiological features of the virus. This work led to a critical understanding of how the virus was impacting patients and potential avenues for therapy.
“It’s important to understand what’s happening in the body when someone has COVID-19 because that gives us information as to why some patients don’t do well and why others recover,” shares Dr. Fraser. “This helps us know who is vulnerable to COVID-19 and how to best offer treatments in the future.”
Read about Dr. Fraser's COVID-19 research:
- Researchers team up with Diagnostics Biochem Canada to study COVID-19
- Study identifies biomarkers that could be used in a quick, inexpensive COVID-19 blood screening tool
- Researchers unravel two mysteries of COVID-19
Work is also underway to find the unique fingerprint that the COVID-19 virus can leave on the lungs. Hospital researchers at Lawson have developed and tested an artificial neural network for diagnosing COVID-19.

Dr. Robert Arntfield, Medical Director, Critical Care Trauma Centre (LHSC) and Lawson Researcher
“The lung ultrasound techniques and the findings of COVID-19 by looking at the lungs didn’t initially look unique when compared to other conditions like pneumonia. Our group wanted to investigate whether or not there were differences that were possibly subvisible,” says Dr. Robert Arntfield, Medical Director of Critical Care Trauma Centre at LHSC and Lawson Researcher. “Through our work, we were able to show that in fact artificial intelligence could outperform a trained clinician in identifying a COVID-19 lung from a similar affected lung that was not due to COVID-19.”
This new technique just scratches the surface of the beneficial use of AI when it comes to medical imaging for patients. “It shone a light on the idea that there were hidden details within all the noise of the image,” adds. Dr. Arntfield. “When you can input that into a machine that is extremely portable the way ultrasounds are, you have a precise diagnostic machine that you can take anywhere a tablet can go.”
The team is now expanding on these findings with further research. Lawson has recently approved Dr. Arntfield’s “Project Deep Breath” which aims to go beyond COVID-19 and explore multiple conditions where lung ultrasounds and AI can be paired together.
Understanding the vaginal microbiome essential to human health
There are trillions of microorganisms inhabiting your body. The majority of these are positive and essential to your health. They include those microorganisms found in the female reproductive system – a highly diverse environment that is crucial to human survival.
Understanding the microorganisms that inhabit the vagina, also known as the vaginal microbiome, is extremely important for women, their offspring and sexual partners. Dr. Gregor Reid recognizes this importance through his research into lactobacilli, the dominant organisms present in the healthy vagina of most women.
Dr. Reid is a Lawson microbiome and probiotics scientist and director of the Canadian Research and Development Centre for Probiotics. His interest in the vaginal microbiome began over 33 years ago.
“In the human gut, the microbiome differs with diet. But there is a global similarity to the vaginal microbiome,” said Dr. Reid. “From early in my career, I suspected a connection between this uniformity and the female’s critical role in reproduction.”
Harmful bacteria, also known as pathogens, can invade the vaginal microbiome to produce a more highly diverse state. This leads to the displacement of lactobacilli. It can also lead to bacterial vaginosis (BV) and the easier contraction of urinary tract infections (UTIs). These two ailments account for numerous physician visits each year and a reduction in a woman’s quality of life.
Mediating pregnancy and infant development
Research suggests that lactobacilli mediate complex changes that occur during pregnancy. If harmful pathogens invade and persist, inflammation and premature delivery can occur during pregnancy.
“The mechanisms behind the displacement of lactobacilli are not clear,” says Dr. Reid. “However, a number of factors can increase risk of BV. These include douching, sexual intercourse, lower estrogen levels and aging. It’s crucial that we conduct further research into these processes.”
Studies also suggest that the human fetus is exposed to the mother’s lactobacilli prior to birth, in addition to exposure during vaginal birthing. Again, understanding of this process and its significance is limited but warrants further investigation, says Reid. We need to further understand how exposure affects an infant’s immunity, metabolism and behavior in both early and later life.
“We’re seeing a dramatic rise in C-sections and a drop in breastfeeding,” says Reid. “If a developing child is not fully exposed to the mother’s lactobacilli, does this provide an opportunity for harmful bacteria to proliferate? This may cause repercussions to the offspring’s own future reproductive health.”
The role of probiotics
As research begins to focus on restoring a lactobacilli-dominant state, probiotics have been explored. However, attempts have presented challenges. “When probiotics are administered vaginally in a dried form, the lactobacilli fail to colonize long-term,” says Dr. Reid. “A study introducing lactobacilli in more natural form may lead to successful colonization. This has been the case in other areas like fecal transplantation.”
Challenges and opportunities
There are a number of other challenges when it comes to the study of the vaginal microbiome. This includes the lack of suitable animal models. While there have been recent developments that may lead to better recreations of a female microbiome, Dr. Reid explains that it will be difficult to mimic the many complexities of the female reproduction system. These include the menstrual cycle, immune responses, the use of douches, sexual intercourse and more.
“To fully understand female health, reproduction and infant development, we need to better understand lactobacilli,” said Dr. Reid. “We know that lactobacilli may help to combat herpes and environmental toxins, improve sperm motility, and even self-cure episodes of UTI and/or BV. What we are slowly uncovering is an understanding of the processes behind these interactions.”
Dr. Reid recently published a paper on this subject, "Cervicovaginal Microbiomes–Threats and Possibilities", in the publication Trends in Endocrinology & Metabolism. Dr. Reid’s own research is currently focused on compounds with the capacity to expand the proportion of lactobacilli at the expense of pathogens. The goal of this research is to improve the health of women across Canada and around the world.
Unique imaging research by Lawson sparks international collaboration
The Bioelectromagnetics and Human Threshold Research Group at Lawson Health Research Institute has an international reputation and expertise on human brain response to time-varying magnetic fields (MFs). This pioneering research has inspired an international collaboration to duplicate Lawson Imaging’s unique experimental expertise in Europe.
The team is now working with EuroMov, a research centre located in France, to duplicate the scientific approach and techniques in a new lab. The goal is to double research capabilities and further stimulate scientific knowledge in this area.
Fluctuating MF induces electric fields and currents in conductive tissues. Above a certain threshold, these fields and currents will change the physiological electric activity within neuronal tissues. Lawson’s team is currently the only one in the world stimulating participants with power-frequency MF of sufficient intensity to result in acute neurophysiological response. This can involve interferences with visual perception, motor output and other cognitive functions.
“An international synergy between the Bioelectromagnetics and Human Threshold Research Group at Lawson and EuroMov will increase the scope of scientific expertise for both institutions” explains Dr. Legros, Director of Bioelectromagnetics and the Human Threshold Research Group at Lawson Imaging. “Both will have access to a wide range of brain stimulation techniques and imaging modalities.”
Through this new collaboration, researchers are excited to merge their expertise and tackle questions together, opening new avenues for original research ideas and projects. This new intercontinental synergy also increases the scope of options for academic funding and international training programs for students.
Furthermore, there is great potential for reinforcing and extending the group’s industry-partnered supporting program, which already associates industry sponsors (such as Hydro-Québec, Électricité De France, Réseau de Transport d’Électricité, NationalGrid/Energy Network Association, Electric Power Research Institute) under an international consortium: the Utilities Threshold Initiative Consortium (UTIC).
The growing network of international scientists working in this field assist international regulation agencies, governments and industries to better understand the impact of electromagnetic exposure on brain activity and physical behaviour. Knowing the thresholds for human responses allows these institutions to adjust their recommendations and policies for when exposures could become unsafe for the public and workers.
The potential applications in research, industry and health care are vast, including the world of video gaming and virtual reality!
“We are excited to see discovered effects and mechanisms translated towards therapeutic applications to the benefit of patients,” says Dr. Legros. “For example, we could improve neuromodulation and neurostimulation technologies to better address movement disorders such as in Parkinson’s Disease. In another application, knowledge of the vestibular responses to stimulation may help to manage symptoms such as motion sickness.”
EuroMov is a university-based European centre for research and innovation in the science of movement. Conducting both fundamental and clinical research, it proposes innovative technological solutions allowing the capture, simulation, learning and rehabilitation of movement. EuroMov contributes to the creation of innovative starts ups and businesses in the field of health, performance, sport, human factors, and rehabilitation.
Dr. Legros is also an Associate Professor in the Departments of Medical Biophysics, Medical Imaging and Kinesiology at Western University’s School of Kinesiology, and an Associate Scientist at EuroMov.
Find out more about his research:

Above: Members of the Bioelectromagnetics and Human Threshold Research Group at Lawson.
From left to right, bottom: Shirin Davarpanah Jazi, Postdoctoral Scholar; Alicia Allen, Masters Candidate; Cadence Maureen Baker, Masters Candidate.
From left to right, top: Michael Corbacio, RA/Lab Manager); Dr. Alexandre Legros, Principal Investigator and group leader; Sebastien Villard, Postdoctoral Scholar.
Missing from the photo: Nicolas Bouisset, PhD Candidate; Lynn Keenliside; Manager Technical Services.
Unlocking boundless potential
Ashmeet Gill had her first PET/CT scan shortly after being diagnosed with Hodgkin’s lymphoma, a cancer of the body’s germ-fighting immune system. She was nervous. Claustrophobia is an issue for the young Stratford resident and the scan, necessary to determine if the cancer had spread beyond the lymph nodes in her neck, would take 34 to 45 minutes, she was told.
Wrapped in a sheet and tucked inside the tube of the PET/CT at St. Joseph’s Health Care London (St. Joseph’s), Ashmeet, then 24, steeled herself to remain calm. But near the end of the scan, a sense of panic set in.
“It was not pleasant but I endured it. I made it through.”
Ashmeet’s next PET/CT scan would be six months later, after six cycles of chemotherapy, to determine if the treatment had worked. She was terrified of another panic episode. By then, however, St. Joseph’s had a brand-new PET/CT – Canada’s first, next generation, state-of-the-art Omni Legend PET/CT from GE HealthCare.
This time, Ashmeet’s scan took “barely 15 minutes or so,” she recalled.
“I thought, seriously? I couldn’t believe I was done. I was so happy.”
With the very first patients scanned with St. Joseph’s new PET/CT machine, it was obvious the breakthrough technology was living up to high expectations.
The machine is fast – decreasing the time it took for a scan from about 45 minutes on the older system to less than 14 – head to toe. Patients are exposed to less radiation, and the ability to precisely detect disease and tiny abnormalities is outstanding.
“This is what we have been waiting for,” says Ting-Yim Lee, a pioneer in the use of machines like PET/CT to gather new, vital information about diseases. “St. Joseph’s new Omni Legend by GE HealthCare is answering the call for patients, clinicians and researchers alike.”
PET/CT is the medical ace in imaging for the assessment and treatment monitoring of cancer, neurodegenerative disorders, and metabolic and cardiovascular diseases. At St. Joseph’s, the possibilities of this technology took a giant leap forward in August 2023, thanks in part to the generosity of donors and a $1 million contribution from St. Joseph’s Health Care Foundation. With the arrival of the new system, St. Joseph’s is set to become Canada’s first national GE HealthCare centre of excellence in molecular imaging and theranostics. This two-pronged approach to diagnosing and treating cancers and other diseases merges molecular imaging with the use of radiopharmaceuticals to identify the location and extent of diseased tissues and selectively destroy the abnormal cells.
“The speed at which we can now do exams means significantly improved comfort for patients while the exceptional image quality changes the game in the hunt for cancerous lesions,” explains Ting, Director of PET/CT Research at Lawson Health Research Institute (Lawson) and medical physicist at St. Joseph’s Hospital.
“For young adults undergoing repeat PET/CT exams due to their medical conditions, managing the radiation dose is critical,” explains Dr. Narinder Paul, Lawson scientist and Chief, Medical Imaging, at St. Joseph’s. “These individuals already face an elevated life-time risk of developing cancer from radiation, and this risk further increases with additional exposures.”
For older adults, the time it takes for the examination is also of great concern. Lying still for long periods can be a hardship due to pain from bone metastases or other conditions, and is a challenge for those who have dementia, are claustrophobic or experiencing other issues, adds Dr. Paul.
“Reducing the exam time is a huge improvement in the patient experience for these individuals.”
While patients hail the new PET/CT experience, clinicians and scientists are raving about the machine’s imaging prowess. The advanced AI-driven image formation technology now empowers the precise detection of cancer within lymph nodes and other anatomical structures, “achieving remarkable accuracy even for very small lesions,” says Dr. Paul.
“The advantages we have seen so far are already impressive but what’s on the horizon in research and care – what we will be able to study and do – is even more exciting,” says Ting.
In particular, the new PET/CT is expected to be the catalyst for ground-breaking clinical research for patients facing breast cancer, Alzheimer’s disease, prostate cancer, epilepsy and obesity. Scientific exploration in these areas is currently being planned at St. Joseph’s that will pave the way for novel treatments, new, non-invasive ways to identify a patient’s risk of disease, the potential to clearly and painlessly view how treatment is working, and the ability to uncover the tiniest abnormalities at play when it comes to diseases and conditions.
The deets on PET-CT
Positron emission tomography (PET) is a medical imaging method that uses a small amount of radioactive material, called a radiotracer or radiopharmaceutical, along with a special camera and computer. This helps doctors see how organs and tissues in the body are working. The radiotracer moves through the body and collects in specific areas, showing where there might be a problem or disease. PET can also be used to check how well a patient is responding to treatment.
A computed tomography (CT) scan takes x-ray images of the body from different angles and uses computer processing to create highly detailed, cross-sectional images (slices) of the body’s structures. It is used to see things that regular X-rays can’t show.
A PET-CT machine allows both types of scans to be performed at the same time and information from these two different types of scans to be viewed on a single set of images. Together, PET-CT provides intricate views with fine details about both the body’s various structures and their functions.
Peering into the future
The following are landmark research projects nearing the starting gate at Lawson Health Research Institute made possible by St. Joseph’s Health Care London’s revolutionary new PET-CT machine.
Breast Cancer
Within the Breast Care Program at St. Joseph’s, research with the new PET-CT scanner will make breast cancer theranostics a clinical reality for the first time worldwide. In other words, it will be possible to treat breast cancer using the powerful, one-two punch of molecular imaging and radiopharmaceuticals to identify the location and extent of diseased tissues and selectively destroy the abnormal cells. Two exciting projects are on the horizon:
The one-two punch: Herceptin is a cancer medicine that interferes with the growth and spread of cancer cells in the body. HER2-positive breast cancer is a type of breast cancer that is more aggressive than other types. By using PET-CT imaging with a specialized form of Herceptin that has been chemically tagged, or "labeled," with a radioactive substance, researchers believe it’s possible for a woman to avoid undergoing a breast biopsy. They will be able to see – literally – if the radiolabeled Herceptin binds to the HER2 proteins and the extent of the HER2-positive cancer. Then, by tagging Herceptin with a therapeutic radioisotope – a special type of atom that emits radiation – the hope is to destroy the breast cancer. St. Joseph’s is investigating this approach first in animal studies before progressing into human trials.
Reducing the risk: Not all breast cancers can be effectively treated with Herceptin. For this group of patients, researchers plan to evaluate newer drugs to reduce the risk of both disease progression and death. The new PET-CT scanner will be able to monitor response from these new treatments.
Alzheimer's disease
The super sensitivity of St. Joseph’s new PET-CT will empower innovative methods to identify individuals at risk of Alzheimer’s disease, those who might benefit from treatment, and early response to treatment. The high-powered machine will allow researchers to simultaneously study both blood flow and glucose metabolism in the brain – something that has not been possible before. Both these mechanisms are believed to be contributing factors in the onset of Alzheimer’s. By measuring both at the same time, researchers hope to uncover early signs that the brain is in trouble and at risk of plaque deposits and toxic proteins that have been linked to the development of Alzheimer’s. Patients will be recruited from St. Joseph’s Aging Brain and Memory Clinic at Parkwood Institute for this ground-breaking study.
Epilepsy
Patients with uncontrolled seizures currently require a hospital stay and the implanting of electrodes deep into the brain to record brain signals that pinpoint where the epileptic seizures are originating. The hospital stay is often long as this method relies on the patient having seizures to properly record and identify the location in the brain responsible. Once the problem area is determined, surgeons intricately remove this part of the brain. Research with the new PET-CT will explore a more efficient approach – the ability to precisely reveal the brain’s seizure epicentre using non-invasive imaging looking at characteristics in the epileptic brain that is present between seizures.
Obesity
In Canada, one in four adults are currently living with obesity, a problem that is causing a surge of obesity-related health challenges. Ozempic is a ground-breaking drug that not only helps people shed weight but also slashes the risk of heart disease by an impressive 20 per cent. However, weight loss attributed to this drug is linked to a reduction in lean muscle mass and the long term effects of that muscle loss remain uncertain. Using PET-CT, researchers will explore potential alterations in muscle energy metabolism resulting from obesity treatment with Ozempic and similar drugs.
Using AI to detect lung cancer recurrence
Lung cancer is the most commonly diagnosed cancer in Canada. While the standard treatment for patients with early-stage lung cancer is surgery, up to half of these patients may develop a recurrence after their treatment.
Jaryd Christie is a Master’s candidate working with Lawson Scientist, Dr. Sarah Mattonen. Together, they are working to develop a new software that uses artificial intelligence (AI) to identify which patients are likely to have recurring cancer.
Currently, basic information like the size of the tumour is extracted from medical images such as a computed tomography (CT) scan to determine a patient’s cancer stage and prognosis. With the new technology, multiple sources of information about the patient will be extracted and used to increase accuracy for determining likelihood of recurrence.
Christie is looking to integrate multi-modal imaging, including CT and positron emission tomography (PET) with a patient’s clinical, pathological and genomic information to build the software. The AI software will find patterns from the data that is extracted and identify imaging features that are associated with recurrence after treatment.
The goal of this research is to improve the ability to identify which patients are likely to be cured. By being able to extract and combine additional information, physicians could provide aggressive treatment options for patients who need it. This would provide lung cancer patients with personalized treatments that could improve their outcomes.
“We also want to look not only at the tumour, but other places like bone marrow and non-cancerous areas in the lung, to see if these additional areas can provide information on disease progression and prognosis,” says Christie, who is completing his Master’s degree in the Department of Medical Biophysics at the Schulich School of Medicine & Dentistry at Western University. “We hope that by combining these different sources of information, we can obtain better disease characterization to more accurately determine if a patient will be cured.”
Christie received a Lawson Internal Research Fund (IRF) Studentship to conduct this research, which will be supervised by Dr. Mattonen.
“Lawson’s IRF is such an important funding opportunity for new investigators. This studentship allows me to support a student while building my research program,” adds Dr. Mattonen. “These funds will allow us to obtain preliminary data that we can use to apply for external funding.”
Using artificial intelligence and brain stimulation to improve treatment for psychosis
Leading the Canadian arm of the project is Dr. Lena Palaniyappan who is using Artificial Intelligence to help personalize treatment for patients with psychosis. Dr. Palaniyappan is an Associate Scientist at Lawson Health Research Institute, Associate Professor at Schulich Medicine & Dentistry and Scientist at Robarts Research Institute.

Dr. Lena Palaniyappan who is using AI to help personalize treatment for patients with psychosis.
In collaboration with five European centres, Dr. Palaniyappan and a team at Robarts Research Institute and Lawson Health Research Institute, the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, will be collecting brain scans and genetic information from more than 60,000 patients in order to understand the relationship between genetics and brain development.
“The study itself involves collecting neuroimaging and genetic information from multiple sites in order to understand the mechanisms of mental illness,” said Dr. Palaniyappan. “The translational portion of this is applying this information to clinic. How genes and brain networks interact to cause mental disorders, and how we can use this information to match patients to specific treatment choices.”
The group is specifically studying a treatment called magnetic stimulation which will be delivered within the mental health care program at St. Parkwood Institute, a part of St. Joseph’s, in collaboration with Dr. Amer Burhan. Dr. Burhan is a Lawson Associate Scientist, Associate Professor at Schulich Medicine & Dentistry and Clinical Physician Lead for Therapeutic Brain Stimulation (ECT and TMS) at Parkwood Institute.

Dr. Lena Palaniyappan is collaborating with Dr. Amer Burhan for this study.
The treatment uses focused magnetic pulses that stimulate a specific group of neurons. Dr. Palaniyappan says the treatment is very effective, but only in one-third of patients.
“We want to know if there are clear markers that show who will respond to this treatment, and who will not. This will help reduce the burden of failed treatment trials for this challenging illness,” said Dr. Palaniyappan.
To enable this, the researchers will look for patterns in a very large amount of imaging and clinical data collected in Europe and Canada. That’s where Artificial Intelligence comes in. In order to understand the patterns that are clinically useful, they use a technique called Machine Learning that trains a computer to recognize expected patterns and then make predictions for new patients.
The data is being collected from six centres, coordinated by Dr. Emanuel Schwarz at the University of Heidelberg, Mannheim, Germany. In addition to the centre here in London, Ontario, other partners include Munich, Germany; Oslo, Norway; Rotterdam, Netherlands; and Montpellier, France.
The research project will also mean that this form of magnetic stimulation treatment will be offered for psychosis patients in London for the first time.
“Magnetic brain stimulation is a safe and well-tolerated treatment that is used currently in London to treat depression, but now we will be able to offer this to patients with psychosis as well,” said Dr. Palaniyappan.
The project will begin in May 2019 and will continue until the end of 2022.
View St. Joseph’s Health Care London's 2017-2018 Annual Report
St. Joseph’s Health Care London’s 2017-2018 Annual Report features stories about patients and residents, and their journey of care and recovery.
The following research is highlighted in the 2017-2018 Annual Report:
- Smart tech, smart treatment: Many mobile applications are on the market to help people struggling with mental health issues, but these aren’t necessarily created or used by health care providers. Creating an entire smart mental health system is one of the strategic priorities of St. Joseph’s and Lawson’s Mental Health Research Group led by Dr. Cheryl Forchuk, Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery. Numerous projects have been identified as components of a plan spanning seven years.
- Walking while talking a possible early predictor of dementia: In a new study, researchers at Lawson and Western University are demonstrating that gait, or motion testing, while simultaneously performing a cognitively demanding task can effectively predict the progression to dementia and eventually help with earlier diagnosis. To date, there is no definitive way for health care professionals to forecast the onset of dementia in a patient with memory complaints.
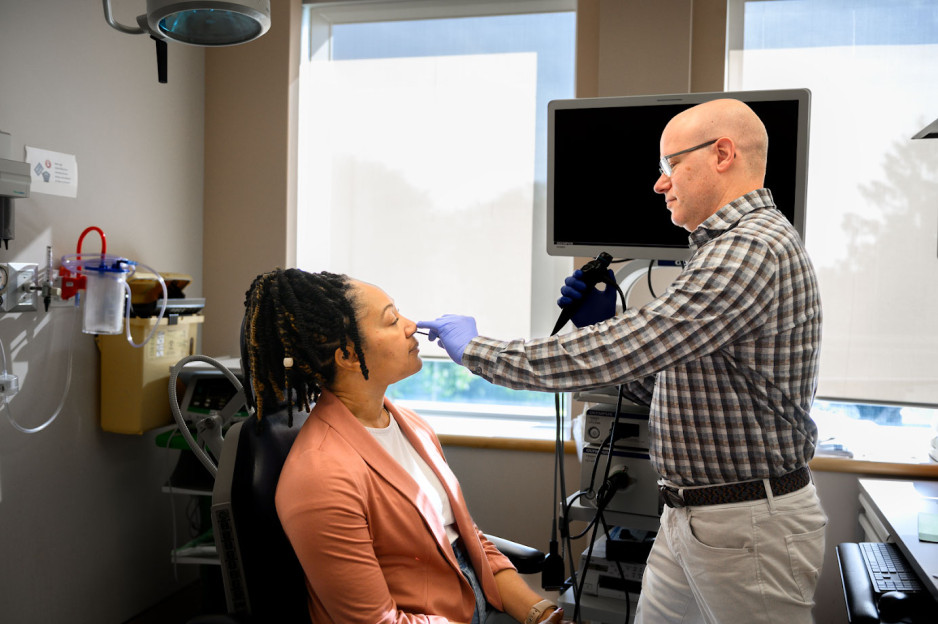
Viral mouth-taping trend ‘sus’ says Canadian sleep expert
Mouth taping, a growing trend on social media channels like TikTok, carries serious health risks, especially for those with sleep-disordered breathing and obstructive sleep apnea, according to a paper published in PLOS One.
The study from Lawson Research Institute (Lawson) of St. Joseph’s Health Care London, London Health Sciences Centre Research Institute (LHSCRI) and Western University’s Schulich School of Medicine & Dentistry also found no strong evidence of health benefits.
The trend involves placing tape over the mouth to stop ‘mouth breathing’ and promote breathing through the nose during sleep. It has been recommended by many social media influencers and celebrities who claim it can lead to better sleep, enhanced oral health and anti-aging results.
“It was concerning to us that celebrities and influencers are endorsing mouth taping without scientific evidence,” says Dr. Brian Rotenberg, researcher at Lawson, LHSCRI and Schulich Medicine & Dentistry. “In the language of social media influencers, it seemed a bit ‘sus,’ so we examined what science is telling us about this trend and whether or not it is safe.”
Rotenberg collaborated with Dr. Elise Graham, paediatric otolaryngologist head and neck surgeon at IWK Health and Jess Rhee a Schulich School of Medicine & Dentistry resident who is training at London Health Sciences Centre (LHSC) on the research. He and his team examined 86 existing scientific studies on the topic, including an in-depth review of 10 studies representing the experience of 213 patients. The team found mouth taping:
- Has no strong scientific evidence of health benefits, contradicting claims on social media.
- Can make existing sleep-disorder breathing worse by restricting airflow, putting additional stress on the respiratory system and increasing risk of suffocation when patients experience a nasal obstruction.
“Our research shows that taping the mouth shut during sleep is dangerous, especially among those who may not be aware they have sleep apnea,” adds Rotenberg, who is also an otolaryngologist and sleep surgeon at St. Joseph’s Health Care London and London Health Sciences Centre (LHSC). “These individuals are unknowingly making their symptoms worse and putting themselves at greater risk for serious health complications like heart disease.”
Rotenberg and his team point to the importance of health research in combatting misinformation and pseudoscience.
“It’s easy for misinformation to run rampant on social media; we’ve seen this countless times over the past few years,” says Rhee. “We need to make health decisions based on strong scientific evidence. Our hope is that people stop taping their mouths during sleep and recognize it is dangerous.”