Search
Search
Leading the conversation on equity, diversity and inclusivity
The city of London, Ontario is home to a vibrant health research community. On Wednesday, May 9, researchers from across the city gathered to discuss the importance of equity, diversity and inclusivity (EDI) in the careers of health researchers. Through participation at Exchange: A London Health Research Day Forum on Diversity & Inclusivity, guests discussed the challenges associated with EDI and potential solutions for the future.
Exchange was held the evening before London Health Research Day, the region’s premier research showcase event which features nearly 400 trainee presentations. Trainees are the future of Canadian science and EDI is crucial to that future. This is a topic of national importance that has garnered attention and action from the federal government, funding agencies and scientists across the country.
Recognizing the importance of this topic, Canada’s Minister of Science, The Honorable Kirsty Duncan, and local Member of Parliament for London North Centre, MP Peter Fragiskatos, shared video greetings with Exchange guests.
“The Exchange event highlights a vital area of discussion. It is important to not only recognize but embrace the differences between scientists and the diverse perspectives they bring to research,” said Rebecca Sullivan, a third year PhD candidate at Western University’s Schulich School of Medicine & Dentistry, training in Savita Dhanvantari’s lab at Lawson Health Research Institute, and one of the organizers of the event. “Becoming aware of our own unconscious biases and trying to change these culturally ingrained implicit associations is the only way to make active change in science!”

Above: Rebecca Sullivan, a third year PhD candidate, leading a scenario-based group activity at Exchange
The evening’s first presenter was Dr. Janet Smylie, Director of the Well Living House Applied Research Centre for Indigenous Infant, Child and Family Health at St. Michael’s Hospital and CIHR Applied Public Health Research Chair in Indigenous Health Knowledge and Information. Dr. Smylie, who also delivered the keynote presentation at London Health Research Day, spoke about the role of anti-Indigenous racism and discrimination within health care professions, including its impact on research. This included a discussion of Dr. Smylie’s own research in the field of Indigenous health.

Above: Dr. Janet Smylie presenting on "Addressing anti-Indigenous racism and discrimination within health care professions"
Greta Bauer, PhD, a professor in the Department of Epidemiology and Biostatistics at Schulich Medicine & Dentistry, spoke about the role of epidemiology as a toolkit for building equity in health research. This included a discussion on incorporating intersectionality and multidimensionality into population health research methodology.
“The purpose of this work is to give researchers the measurement and statistical tools they need to shift the focus from studying broad population average effects to more heterogeneity within populations,” said Greta. “The whole point is to better study not only diversity in health outcomes, but in the processes that generate those outcomes.”

Above: Greta Bauer, PhD, presenting on "Epidemiology as a toolkit for building equity"
This talk was followed by a presentation on Gender-Based Analysis Plus (GBA+). GBA+ is an analytical tool used to assess how diverse groups of women, men and gender-diverse people may experience policies, programs and initiatives. The “plus” in GBA+ acknowledges that GBA goes beyond biological (sex) and socio-cultural (gender) differences. We all have multiple identity factors that intersect to make us who we are; GBA+ also considers many other identity factors, like race, ethnicity, religion, age, and mental or physical disability. GBA+ is a method for collecting and reviewing data in an unbiased manner, one that leaves aside many of the assumptions that can mask the GBA+ impacts of a given initiative. Alysha Croker, PhD, Manager, Tri-Agency Institutional Program Secretariat, discussed how GBA+ is being used in research and grant funding, including at the federal funding agencies.
“Diverse research teams can lead to more innovation, greater collective intelligence and an increased capacity to tackle complex issues,” said Alysha, when discussing the importance of EDI in the careers of health researchers.

Above: Alysha Croker, PhD, presenting on "Incorporating Gender-Based Analysis Plus (GBA+) in research and beyond"
The evening also included a presentation from Shantal Feltham, founder and CEO of Stiris Research, a North American clinical trials management company based in London. Shantal discussed the importance of ensuring that clinical trials are designed to recruit diverse research participants that represent real patient populations. She also discussed her own experiences and perspectives as a female entrepreneur.

Above: Shantal Feltham delivering a presentation titled "That’s a great idea – It’ll never work"
A group of health research trainees concluded the night with a scenario-based presentation and activity. Audience members were divided into small groups and given a diversity scenario to discuss. Topics ranged from the experiences of LGBTQ+ researchers, racial diversity, physical ability barriers in research labs and more. Notes and ideas from these conversations were recorded and displayed the next day at London Health Research Day.
“Exchange highlighted EDI in health research in action. It featured talks by leading female researchers on issues in Indigenous health and LGBTQ health, implementation of equity in the Canada Research Chairs program, and female entrepreneurship in the field of health research,” said Savita Dhavantari, PhD, assistant director and scientist at Lawson and assistant professor at Schulich Medicine & Dentistry. Savita was also one of the Exchange organizers and the facilitator for the event. “Above all, I hope attendees were encouraged to be fearless in advocating for equity, diversity and inclusivity in health research.”

Above: Guests at Exchange discussing a diversity scenario

Above: Savita Dhanvantari, PhD, facilitating the Exchange event
To see more photos from Exchange and London Health Research Day, visit the London Health Research Day website.
Exchange and London Health Research Day are presented in partnership by Lawson Health Research Institute and Western University’s Schulich School of Medicine and Dentistry.
Lens of compassion improves health care
Keynote speaker at joint mental health research day says compassion in action has proven benefit
Compassion in mental health care – and in all health care – is “what separates good from really great” patient outcomes, Calgary-based researcher Shane Sinclair, PhD, told mental health researchers during a conference Oct. 30, 2024, in London.
Sinclair, who heads the Compassion Research Lab at the University of Calgary, was the invited keynote speaker at the Joint Mental Health Research and Innovation Day, attended by about 130 people.
The event was hosted by Lawson Research Institute, London Health Sciences Centre Research Institute and Schulich School of Medicine & Dentistry.
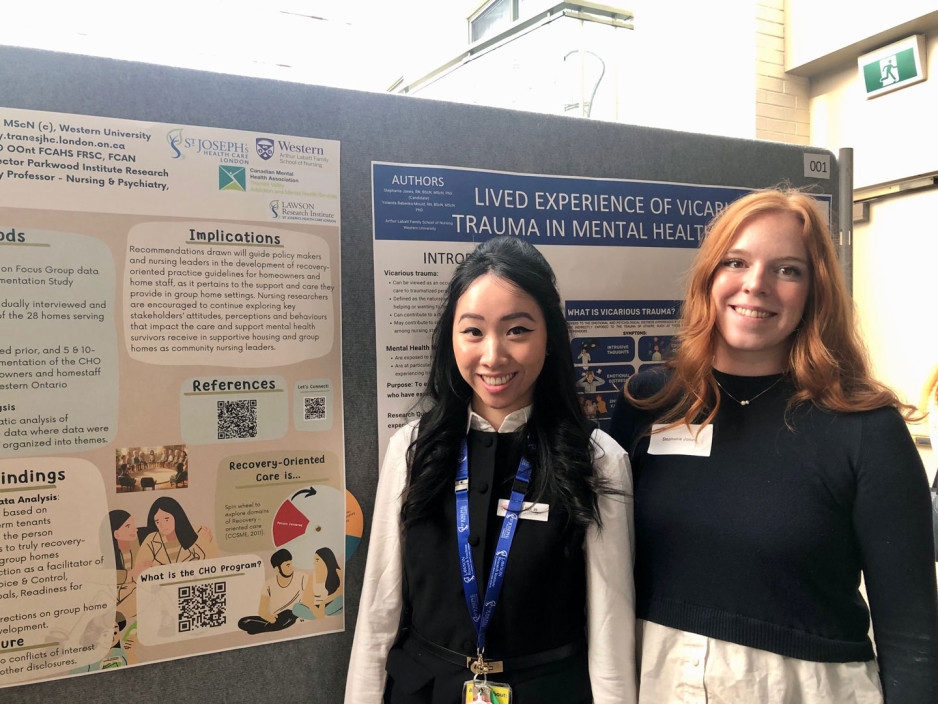
The day also featured 17 poster presentations and 17 oral presentations on different aspects of mental health research. It’s one of the premier annual education-and-development events in mental health science regionally.
This year’s event showcased how compassion could transform health policy, partnerships, systems, care, research and service delivery.
Compassion, respect and excellence are core values of St. Joseph’s Health Care London.
Sinclair noted that the key role of compassion – responding to someone’s suffering with understanding and action – is evidence-based.
“We do patient-informed and patient-targeted research. And we’ve found compassion makes a difference in how people heal.”
-Shane Sinclair, PhD, compassion researcher
His lab examined the outcomes and satisfaction among patients at 14 emergency rooms across Alberta and found compassion to be the greatest predictor of quality care ratings.
“What separates good from really great comes down to compassion. These things matter,” Sinclair said.
“It improves their health and their quality of life. It reduces health-care costs, reduces adverse medical outcomes and helps build patients’ trust in the medical information and direction they receive,” he said.
Leveraging technology to diagnose psychiatric disorders
Psychiatric disorders are often difficult to diagnose. As research advances, we are learning there are multiple subtypes of illness that differ in symptoms and treatment needs, making classification even harder. Post-traumatic stress disorder (PTSD) is one example. Individuals with the more common type of PTSD experience active defensive responses like hyperarousal or outbursts of emotion while those with the dissociative subtype experience additional passive defensive responses like ‘shutting down’ or out-of-body experiences.
In a new study from Lawson Health Research Institute and Western University, researchers combined brain imaging and machine learning to classify with 92 per cent accuracy whether individuals had PTSD and whether or not it was the dissociative subtype. The results highlight the promise of brain imaging as a tool for early diagnosis of psychiatric illness, helping to predict symptom development and treatment needs.
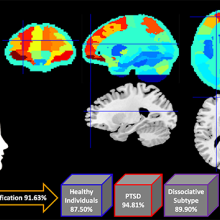
Brains scans and machine learning were combined to classify PTSD with 92 per cent accuracy.
The study involved 181 research participants, including those diagnosed with the more common form of PTSD, the dissociative subtype of PTSD, and healthy individuals with no history of PTSD. They participated in functional magnetic resonance imaging (fMRI) at St. Joseph’s Health Care London and Robarts Research Institute.
Researchers used the high-powered imaging to analyze patterns of resting-state brain activity where participants simply remained in a state of restful wakefulness in an fMRI scanner. The team found that unique patterns of brain activity differed significantly between the three groups.
“Our research group has been leading a number of studies that have shown differences in brain activity and neural connections between healthy individuals and those with different subtypes of PTSD,” says Dr. Ruth Lanius, a researcher at Lawson, professor at Schulich School of Medicine & Dentistry at Western University and psychiatrist at London Health Sciences Centre. “This study further validates that unique patterns of brain activity are associated with different forms of PTSD.”
In the second part of the study, the research team inputted the patterns of brain activity into a machine learning computer algorithm. They found the machine learning system could analyze brain scans to predict whether an individual had PTSD, the dissociative subtype of PTSD or no PTSD with 92 per cent accuracy.
“Our study suggests brain activity can be used to assist diagnosis of psychiatric disorders and help predict symptoms,” says Andrew Nicholson, PhD, lead author on the study and a post-doctoral fellow at Schulich Medicine & Dentistry who is conducting research at Lawson. “Patterns of brain activity are objective biomarkers that could be used to diagnose PTSD and, with more research, even predict response to treatment.”
Objective biomarkers hold promise for transforming psychiatric medicine.
“The field of psychiatry does not currently have objective biomarkers like those used to diagnose and understand other illnesses or diseases like cancer,” says Nicholson. “By discovering and validating patterns of brain activity as biomarkers, we can bring objective measures to psychiatry and transform patient care.”
The study, “Machine learning multivariate pattern analysis predicts classification of posttraumatic stress disorder and its dissociative subtype: A multimodal neuroimaging approach,” is published in Psychological Medicine.
Leveraging virtual reality to manage pain in paediatric patients
London - A new study underway through Lawson Health Research Institute and Children’s Hospital at London Health Sciences Centre (LHSC), using virtual reality (VR) to help pediatric patients during painful and distressing procedures.
“Technology holds immense potential for improving the experience of our young patients and their families,” explains Dr. Naveen Poonai, Lawson Scientist, principal investigator and Emergency Department Physician at Children’s Hospital. “VR is becoming increasingly popular amongst young people and some early research shows VR has been helpful in painful procedures, even in adults.”
The study is focusing on pediatric patients who need port access. A port is a little reservoir that sits underneath the skin that allows access to blood or medication with the use of a needle. Ports are most commonly used in pediatric cancer patients.
“This can be very distressing for a patient and it can set the tone for their entire clinic day and course of treatment,” says Dr. Alexandra Zorzi, Lawson Associate Scientist and Pediatric Oncologist at Children’s Hospital. “Minimizing the stress, anxiety, and pain of the procedure is key to avoiding a negative experience.”
The study team is recruiting 90 pediatric patients with existing medical ports. Participants will be randomized into three groups. One group will be using a VR headset that will allow them to play interactive games. The second group will have access to tablet technology, and the final group will be provided with non-technology distractions. Each procedure and the patient’s response will be recorded. Responses will then be compared using a tool called the ‘Observational Scale of Behavioral Distress’ to determine which intervention leads to the best outcomes.
“My hopes are that we develop a variety of skills we can tailor to patients,” adds Dr. Zorzi. “There are patients who receive all kinds of support but still struggle, so having a variety of techniques available to see what works best is a positive step forward.”
The study is expected to be completed by the end of this year. The research team is already collaborating with Children’s Hospital staff and leadership to use VR as a clinical tool if the study proves the technology to be effective.
“We have plans in place to allow whatever we find as the best option to be part of routine care for kids needing port access,” notes Dr. Poonai. “We are also speaking with various medical teams to determine how we can incorporate this into practices across the hospital.”
The use of the VR devices has been made possible with generous support from the Children’s Health Foundation.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
LHSC and St. Joseph’s introduce new research institutes
Lawson Research Institute at St. Joseph’s and London Health Sciences Centre Research Institute will strengthen hospital-based innovation in London, Ontario
LONDON, Ont. – Today, London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London (St. Joseph’s) unveiled new research institutes designed to strengthen hospital-based innovation. Lawson Research Institute (Lawson) at St. Joseph’s and London Health Sciences Centre Research Institute (LHSCRI) will leverage each hospital’s unique areas of clinical focus while further integrating research with care, helping to advance discoveries that lead to improved patient outcomes.
The new institutes were announced at a launch event with guided open house tours taking place across LHSC’s Victoria Hospital, Children’s Hospital and University Hospital, as well as at St. Joseph’s Hospital and Parkwood Institute. Attendees were able to experience signature research areas, including aging, mental health and microbiome research at Lawson, as well as cancer, children’s and mental health research at LHSCRI. The day included demonstrations of discoveries that are reshaping care in Ontario and around the world, including a new robotic, body-weight support for people with mobility difficulties and studies using artificial intelligence (AI) to diagnose rare diseases.
“When research takes place in a hospital context, scientists have more direct connection to the needs of the patients they serve,” said Roy Butler, President and CEO of St. Joseph’s. “There’s data to show that patients treated in research-intensive hospitals live longer because they have access to cutting-edge science. All patients benefit, not just those involved in clinical trials – and that’s the power of health research. That’s why this milestone day and the discoveries to come are real cause for celebration.”
LHSC and St. Joseph’s have been innovating for more than 150 years. The research institutes will build on the legacy of scientific excellence at both organizations. Their launch marks the completion of the transition from Lawson Health Research Institute, a research brand shared between the two organizations since 2000.
“We’re building on our history while introducing the next era in health research excellence, ensuring we will continue to attract the brightest minds in science and that patients will receive world-class, innovative care,” said David Musyj, Supervisor, LHSC. “We will continue to collaborate with each other, Western University, and health research partners across the country and around the world, bolstering London’s position as a national hub for health research.”
Research teams across Lawson and LHSCRI will continue to collaborate closely on projects and large scientific initiatives. LHSC and St. Joseph’s will also continue to share administrative support for research activities.
Learn more about the new research institutes and their transformative work at:
Lawson Research Institute
London Health Sciences Centre Research Institute
-30-
For more information, please contact:
Celine Zadorsky
Senior Media Relations Consultant
London Health Sciences Centre
(226) 927-2309
OR
Debora (Flaherty) Van Brenk
Communications Consultant
St. Joseph’s Health Care London
226-577-1429 or 519-318-0657
About Lawson Research Institute: Lawson Research Institute, the health innovation arm of St. Joseph’s Health Care London, is committed to making and sharing discoveries that improve lives locally and internationally. Every day, Lawson’s 250-plus scientists work to transform imagination to innovation to patient impact. Lawson leads health-care research. Find us online at sjhc.london.on.ca/research and on social media @stjosephslondon
About London Health Sciences Centre Research Institute: At London Health Sciences Centre Research Institute (LHSCRI), our teams pioneer discoveries that transform the health of adult and paediatric patients around the world. As the research institute of London Health Sciences Centre (LHSC), we conduct research where patient care is delivered, working alongside patients, families, health-care providers and academic partners like Western University. We are leaders in advancing the understanding, diagnosis, treatment and management of diseases and health conditions through a diverse research program that ranges from laboratory-based science to clinical trials. Our research has a global impact as we build on LHSC’s 150-year legacy of health innovation and drive forward medical breakthroughs that make a difference in the lives of patients and their families. Find us online at www.lhscri.ca and on social media @LHSCRI.
LHSC and St. Joseph’s Research Institutes Launch Day
Join us and the London community as we celebrate the launch of our new research institutes at London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London (St. Joseph’s).
This full-day event that is open to the public will showcase the legacy and future of hospital-based research in London. It’s a chance to engage in cutting-edge research, interact with research teams and take part in the unveiling of our new research brands.
LHSC and St. Joseph’s Research Institutes Launch Day
Date: Wednesday, October 16, 2024
Formal presentation:
- 9:30 am to 10:00 am | Parkwood Institute Main Building Auditorium, 550 Wellington Road South, Zone B, Room B2-109 (Entrance C)
Open houses:
- 11:00 am to 1:00 pm | St. Joseph’s Parkwood Institute, 550 Wellington Rd. S. Main Building (entrance C) and Mental Health Care Building (entrance F)
- 12:30 pm to 2:30 p.m. | LHSC’s Victoria Hospital, 800 Commissioners Rd. E. (Zone B entrance)
- 1:30 pm to 3:30 pm | St. Joseph’s Hospital (Cheapside entrance 4)
- 2:30 pm to 4:30 pm | LHSC’s University Hospital, 339 Windermere Rd. (Main entrance)