Search
Search
Changing lives through innovation
It started like any other day. Paul Garrett could never have imagined that by the end of the day, he would be paralyzed from the waist down.
On May 25, 2019, Paul was making coffee before another day’s work as an appliance installer when he noticed a slight tingling in the toes of his right foot. Being fairly fit and in his early sixties, he didn’t think much of it – until the numbness got worse, moving up to the base of his spine and down the other leg. Within 30 minutes of the initial sensation, he lost all feeling and function in his legs.
Paul was rushed to the nearest emergency department. For some reason, he knew his life had changed forever. He assumed he was suffering from a stroke.
“Before the ambulance arrived, it was terrifying and emotional. I had this feeling I would never walk again.”
"... Nothing was working when I got to Parkwood Institute."
It wasn’t a stroke but Paul was right about the life-altering ramifications. After days of testing, he was diagnosed with acute onset transverse myelitis, a rare neuroimmune disorder where inflammation damages the insulating material (myelin) covering the nerves along the spine. Without this protective coating, signals from the brain to the spine and back cannot occur.
Paul came to St. Joseph’s Health Care London’s Spinal Cord Injury (SCI) Rehabilitation Program at Parkwood Institute, where his care team partnered with him and wife Brenda to develop a recovery plan.
“They started from scratch with me, nothing was working when I got to Parkwood Institute,” says Paul.
When occupational therapist Charlie Giurleo asked Paul and Brenda what their initial goals for rehabilitation were, they were quick to answer. Paul wanted to get to his son’s wedding, just a month away. The team, and
Paul, got to work, focusing treatments and exercises on learning how to get out of bed, transfer from the wheelchair to the car, and stand independently.
"... We were able to move on and adapt, thanks to the team..."
“I made it to the wedding, and I was even able to stand for a few pictures with my family. It was amazing.”
Then it was time to set longer term goals for his recovery and Paul knew exactly what he wanted, “I wanted to walk out of the building on my own.”
While the physical recovery was a significant hurdle for the Garretts, so was the emotional recovery.
“The SCI Rehabilitation Program team gave us wonderful support and information on how to live with a spinal cord injury,” says Brenda. “There was a lot of grief in the beginning for a life that was profoundly changed and would never be the same again, but we were able to move on and adapt thanks to the team at Parkwood Institute who were so positive and empowering.”
Emboldened by his care team, Paul was able to remain upbeat. Each time he met a new health care provider, he would tell them, ‘You’re on Team Paul now,’ as he held up his hand for a fist bump.”
Getting stronger
With the support of Team Paul, including his wife, a determined Paul worked on his walking one day at a time. “The team said to me, to go quicker is to go slower… to remain focused every day and get a little bit stronger.”
Paul was fortunate to have access to specialized rehabilitation equipment and expertise of members of St. Joseph’s Gray Centre for Mobility and Activity as part of his treatment.
“The equipment and the expertise in The Gray Centre were instrumental in Paul’s recovery.”
The Gray Centre is focused on expanding and advancing mobility and rehabilitation treatment and prevention solutions through research and collaborations between scientists and health care providers using the latest technology and innovations.
“Current patients of St. Joseph’s rehabilitation programs are already benefiting from The Gray Centre,” says physiotherapist Stephanie Cornell. Stephanie was a big part of Team Paul, supporting his rehabilitation plan and treatment.
“The equipment and the expertise in The Gray Centre were instrumental in Paul’s recovery,” says Stephanie. “Utilizing technology such as the body weight support treadmill, we were able to help Paul relearn a walking pattern and get back to being more active in his community.”
All of Paul’s hard work paid off. After his last rehabilitations session he met his goal and walked out of the building on his own. Members of Team Paul lined his pathway out to cheer him on and mark the momentous occasion.
Our first event
Introducing The Gray Centre for Mobility and Activity
This virtual session on Oct. 21 presented a selection of the latest research and treatments in mobility and activity health care.
Watch a recording of the event.
Hear presentations from:
Sue Peters, PhD
Wireless Neuroimaging During Mobility to Predict Recovery Trajectories after Stroke
Stroke survivors say their top rehabilitation priority is to regain the ability to walk. Yet, one out of three stroke survivors do not walk in their community after discharge from rehabilitation. Though a stroke damages the brain, clinicians fail to use brain measures to guide the rehabilitation process. The problem is that there are no proven neuroimaging predictors of mobility recovery. Excitingly, wireless neuroimaging can now allow us to discover more ecologically valid data. Learn more about the possibilities of collecting neuroimaging data using wireless technology during mobility tasks (e.g., overground walking, stairs) at multiple timepoints during a patient’s rehabilitation stay.
Swati Mehta, PhD
Virtual Physical Activity Programming During Pandemic
The current pandemic has reduced access to safe, monitored physical activity (PA) programs for persons with spinal cord injury (SCI). Inactivity can contribute to a multitude of secondary complications including worsening physiological and psychosocial health. Learn about the use of telerehabilitation for continuing activity engagement without the risk of virus exposure.
Dr. Manuel Montero-Odasso
Mobility and Cognition. The Collision of 2 Giants
Until recently, cognitive and mobility research in older persons has been performed in silos, creating knowledge gaps and obscuring the shared mechanisms that cause both cognitive and mobility impairments. Considering cognitive and mobility impairments separately is not only inefficient but it does not acknowledge the reality that leads to insidious disability in older people caused by dementia and falls. Learn more about our research in cognition and mobility.
Stephanie Cornell, MPT
Who, What, When? Using Technology in Rehab
Parkwood Institute is home to specialized rehabilitation programs with access to some of the most advanced rehab technologies in Canada. Effective and appropriate use of rehab technology means that our patients receive the best care possible, when they need it. But there needs to be a coordinated plan in place to ensure both competency in technology use and sustainability over the long-term. Learn more about our training, education and evaluation model for utilizing rehabilitation technology in practice.
Recipients of the Gray Centre 2022 Catalyst Grant Competition
The Gray Centre for Mobility and Activity recently completed the 2022 Catalyst Grant Competition. Catalyst grants are intended to provide seed funding to develop innovative research and clinical ideas and better position these projects to secure subsequent larger grants from external agencies. The Catalyst Grant Evaluation Committee reviewed several very strong proposals and selected four studies for funding:
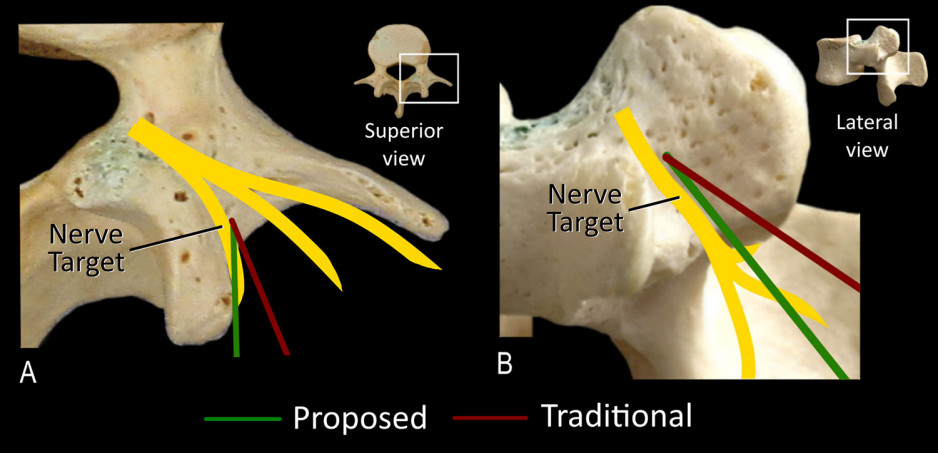
Evaluation of a novel technique for lumbar medial branch denervation to treat chronic mechanical low spinal pain originating from the facet joint:
Lead Investigator: Dr. Eldon Loh
A common treatment for chronic mechanical low back pain is to guide a small radiofrequency electrode towards specific joints in the spine and destroy the surrounding sensory nerves that are signaling pain to the brain. When successful there is substantial pain relief for the patient but the results are inconsistent, likely due to inaccurate site targeting of the electrode. In this work, Dr. Eldon Loh and his colleagues will first test in cadavers the safety and efficacy of a potentially more accurate method of guiding the electrode to these spinal joints. If successful, this method will then be used clinically in a small cohort of consenting patients to determine whether a larger randomized control trial testing this novel method should be conducted.
Pilot of an online, integrated behaviour change and physical activity program for those with neurological conditions:
Lead Co-Investigators: Swati Mehta PhD, Dalton Wolfe PhD
There is significant disparity in access to physical activity programs for people with mobility impairments, which greatly impacts mobility, function and long-term wellbeing. Swati Mehta, PhD, Dalton Wolfe, PhD, and their colleagues will test an online, group-based intervention consisting of exercise and behaviour activation strategies targeting these and other outcomes. Importantly, this programming will be applied to patient groups across several clinical programs at Parkwood Institute.
Study into the effect of transcutaneous vagus nerve stimulation on upper limb function in individuals with paralysis caused by spinal cord injury
Lead Co-Investigators: Drs. Keith Sequeira, Eldon Loh, and David Allison, PhD
The vagus nerve normally plays an important role in many of the body’s functions. Unfortunately, following spinal cord injury the activity of the vagus nerve is commonly reduced. Artificially stimulating the vagus nerve through a process known as vagus nerve stimulation (VNS) can help to increase the activity of this nerve and new evidence from animal models has shown that this treatment can improve physical recovery after spinal cord injury. For this study, Drs. Keith Sequeira, Eldon Loh, and David Allison, PhD, will test whether VNS in addition to traditional rehabilitation services lead to better mobility outcomes for patients with spinal cord injury compared to traditional rehabilitation services alone.
Evaluation of the perspectives of individuals with chronic neurological conditions regarding existing activity programs at Parkwood Institute:
Lead Investigator: Janelle Unger, PhD
One of the main goals of the Gray Centre is to expand the mobility and activity programming that Parkwood Institute offers to community members living with chronic conditions. A critical component to this expansion is evaluating existing programs to identify their strengths and challenges. In this work, Janelle Unger, PhD, and her colleagues will conduct a large series of interviews to explore the lived experiences of individuals participating in Parkwood Institute’s existing activity programs. The research team will then develop recommendations for how to best modify these current programs and optimally develop future program and service provisions.
The Gray Centre is excited to support these innovative projects. Congratulations to all the 2022 catalyst grant recipients.
Rehabilitation following lower limb loss
The fastest growing age group in Canada are those over 80 years old. This age demographic is most likely to have chronic medical conditions such as vascular disease and diabetes, which are also two of the primary causes for why individuals undergo lower limb amputation. Unfortunately, very little research focuses on the rehabilitation and long-term health outcomes of this oldest age cohort following this life changing procedure.
The Gray Centre’s Mobility Experts, Drs. Michael Payne, Ricardo Viana and Susan Hunter (PhD), along with their collaborators, Drs. Courtney Frengopoulos and Katherine Fuller, recently published an article in Prosthetics and Orthotics International, which synthesized all the existing scientific knowledge regarding prosthetic rehabilitation for those over 80 years old after lower limb amputation. Although much more research is needed, the research group found that this oldest age cohort can often perform normal activities of daily living and be discharged to home following a rehabilitation program but may need support from a caregiver or family member. Dr. Frengopoulos explains the full scope of their findings in the video below.
Using technology to support motor recovery following stroke: A panel discussion
An ever-growing body of evidence supports the use of technology-based interventions for physical rehabilitation in stroke, yet their use in clinical practice has traditionally been low compared to behavioral interventions.
This presentation provides an overview of the technologies and devices for motor rehabilitation post stroke, the evidence for their use, and the results from a national survey of awareness and use of these technologies among physical and occupational therapists.
The panel discussion examines the barriers that limit awareness and use of technologies, how to implement these therapeutic options in practice and educate more researchers, clinicians and patients on their importance. The panel consists of researchers, a therapist, an administrator, a physiatrist and a person with lived experience.
Presenters: Amanda McIntyre, Marcus Saikaley, Manny Paiva, Karen O'Neil, Vern Robinson, Robert Teasell
View the video event: Using Technology to Support Motor Recovery Following Stroke
This event took place on June 30, 2022
Ali Bateman
Ali Bateman, MD
Assistant Professor, Schulich School of Medicine and Dentistry
Acquired and Traumatic Brain Injury; Spinal Cord Injury
Dr. Ali Bateman is a physiatrist at Parkwood Institute and an Assistant Professor in the Department of Physical Medicine and Rehabilitation Schulich School of Medicine & Dentistry at Western University. She is also an Associate Scientist at Lawson Health Research Institute, and the Quality Improvement Lead in the Department of Physical Medicine & Rehabilitation.
Dr. Bateman completed her medical degree and residency training at Western University, and is currently completing a master’s degree in Quality Improvement and Patient Safety through the Institute of Health Policy, Management, and Evaluation at the University of Toronto. She is also certified by the Canadian Society of Clinical Neurophysiologists and holds the designation of CSCN Diplomate (EMG). As a consultant physiatrist, Dr. Bateman provides care in acquired brain injury and spinal cord injury rehabilitation programs and the electrodiagnostic laboratory at Parkwood Institute.
Her research interests centre on quality improvement, patient safety, and knowledge translation with the aim of achieving best practices so that all persons with spinal cord and/or brain injury receive the best quality care.

Caitlin Cassidy
Caitlin Cassidy, MD
Assistant Professor, Schulich School of Medicine and Dentistry
Childhood Onset Conditions; Implementation Science and Education
Dr. Caitlin Cassidy is a physiatrist at Parkwood Institute and an Associate Professor in the Department of Physical Medicine and Rehabilitation, and is also cross appointed to the Department of Paediatrics. Her primary clinical and research roles revolve around the Transitional and Lifelong Care (TLC) program at Parkwood Institute. The TLC program provides longitudinal rehabilitative care to adolescents and adults living with a physical disability of childhood onset, many of whom experience mobility challenges and may struggle to find accessible opportunities to increase their fitness and activity levels.
Dr. Cassidy’s research interests include the natural history and long-term outcomes of people with these conditions, and collaborates closely with Dr. Laura Brunton from the School of Physical Therapy at Western University to determine the impacts that access to activity and wellness programming have on pain, fatigue and other outcomes for people with cerebral palsy and spina bifida. Dr. Cassidy also acts as the discipline lead for Musculoskeletal Medicine in undergraduate medical education at Schulich School of Medicine & Dentistry at Western University.

Dalton L. Wolfe
Dalton L. Wolfe, PhD
Lawson Scientist, Parkwood Institute Research
Implementation Science and Education; Spinal Cord Injury
Dalton Wolfe is a Scientist at Lawson Health Research Institute, an Assistant Professor in the Faculty of Health Science and leads the Research 2 Practice (R2P) team, which is a unique research program within Parkwood Institute that focuses on strategies for generating evidence and implementing best practice within rehabilitation. Professor Wolfe’s primary research interest is in the area of knowledge mobilization and best practice implementation with a focus on physical activity and activity-based therapies in spinal cord injury and brain injury rehabilitation.
Professor Wolf also co-leads the Ontario SCI Implementation, Evaluation and Quality Care Consortium, which focuses on implementation of quality indicators towards the enhancement of care across the 5 academic health centres involved in SCI rehabilitation in Ontario. As part of the Parkwood Rehabilitation Innovations in Mobility Enhancement initiative (PRIME), Professor Wolfe is focused on enhancing clinical decision-making to improve locomotor and other movement-related outcomes with activity-based therapies such as robotic, manual and FES-assisted therapies. As with many of the R2P initiatives this involves implementation science and participatory research methods to put in place practice-based research infrastructure that enables iterative knowledge generation as well as implementation. Trainees work alongside clinicians, administrators and persons with lived experience to tackle clinically relevant questions.

Eldon Loh
Eldon Loh , MD
Associate Professor, Schulich School of Medicine and Dentistry
Chronic Pain
Dr. Eldon Loh is a Physiatrist at Parkwood Institute and an Associate Professor in the Department of Physical Medicine and Rehabilitation at the Schulich School of Medicine and Dentistry at Western University. He completed residency training in Physical Medicine and Rehabilitation at the University of Alberta in 2010 and a clinical fellowship in interventional pain management in 2011. His research interests include improving the management of chronic neuropathic pain after spinal cord injury, and the development of novel and improved techniques for interventional pain management of axial spine pain.
He is Chair of the panel that developed and updates the Canadian Best Practice Guidelines for Neuropathic Pain after spinal cord injury and works with international partners to improve point-of-care tools for implementing the guidelines. His interventional pain research focuses heavily on a bench to bedside approach, utilizing anatomical findings to inform clinical practice. He has also examined the impact of Ontario’s healthcare utilization of different interventional procedures such as radiofrequency ablation and paravertebral nerve blocks.